Are you looking for valuable nursing insights on managing and considering bronchitis? Look no further! This article provides essential information regarding nursing considerations for bronchitis, ensuring you have the knowledge and skills necessary to offer the best care possible for your patients. With a focus on nursing management and considerations, you’ll be equipped with the tools to effectively assist individuals suffering from this respiratory condition. Stay tuned to discover expert tips and guidance on providing optimal care for your patients with bronchitis.
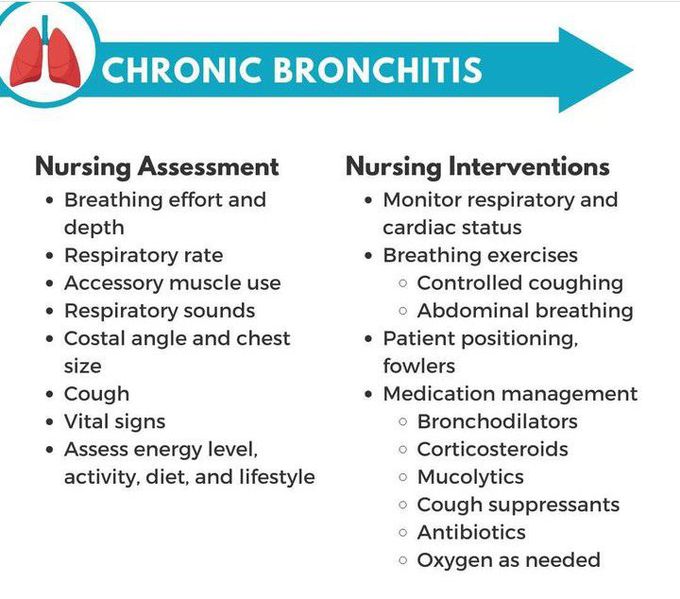
Assessment Considerations
Patient History
When assessing a patient with bronchitis, it is important to gather a comprehensive patient history. This includes any past medical conditions, such as asthma or allergic rhinitis, as well as any recent respiratory infections or exposure to irritants. It is also important to take note of the patient’s smoking history and occupation, as these factors can contribute to the development of bronchitis.
Signs and Symptoms
The signs and symptoms of bronchitis may vary depending on the type of bronchitis (acute or chronic) and the severity of the condition. Common symptoms include cough, which may produce yellow or green mucus, chest discomfort or pain, shortness of breath, wheezing, and fatigue. Some individuals with acute bronchitis may also experience fever and body aches.
Physical Examination
During the physical examination, the nurse should assess the patient’s respiratory status by observing their breathing pattern, lung sounds, and use of accessory muscles. The nurse should also assess the patient’s vital signs, looking for signs of increased respiratory rate, elevated temperature, and decreased oxygen saturation levels.
Diagnostic Tests
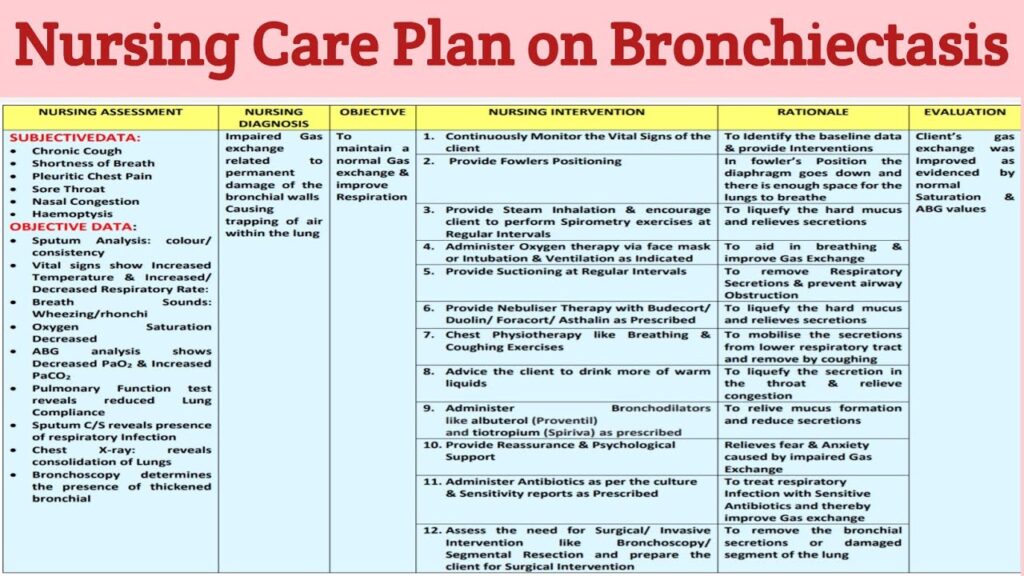
To confirm the diagnosis of bronchitis, diagnostic tests may be ordered by the healthcare provider. These can include a chest X-ray to rule out other conditions such as pneumonia, as well as sputum culture and sensitivity to identify the causative organism. Pulmonary function tests may also be done to assess the patient’s lung function and determine the severity of bronchial obstruction.
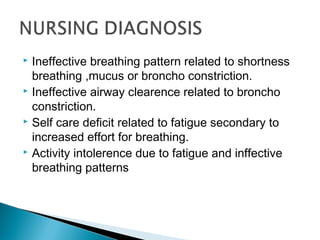
Nursing Diagnosis
Impaired Gas Exchange
Impaired gas exchange is a common nursing diagnosis for patients with bronchitis. The inflammation of the bronchial tubes can lead to a decrease in the exchange of oxygen and carbon dioxide in the alveoli, resulting in decreased oxygenation of tissues. It is important for the nurse to monitor the patient’s oxygen saturation levels and provide interventions to improve gas exchange, such as administering supplemental oxygen and promoting deep breathing exercises.
Ineffective Airway Clearance
The excessive production of mucus in bronchitis can lead to ineffective airway clearance. The nurse should assess the patient’s ability to clear secretions through coughing and suction if necessary. Additionally, the nurse should encourage the patient to drink fluids and use humidifiers to help loosen the mucus and promote effective airway clearance.
Ineffective Breathing Pattern
Bronchitis can also cause an ineffective breathing pattern due to bronchial constriction and increased work of breathing. The nurse should monitor the patient’s respiratory rate and effort and provide interventions to promote effective breathing, such as administering bronchodilators and teaching the patient relaxation techniques.
Planning and Goals
Improve Gas Exchange
The goal is to improve gas exchange to ensure adequate oxygenation of tissues. This can be achieved by providing supplemental oxygen as needed, monitoring oxygen saturation levels, and encouraging the patient to practice deep breathing exercises to expand the lungs and improve ventilation.
Maintain Clear Airway
The goal is to maintain a clear airway by promoting effective airway clearance. This can be accomplished by assisting the patient with coughing and suctioning if necessary, encouraging fluids intake to thin the mucus, and providing humidification to break up thick secretions.
Achieve Effective Breathing Pattern
The goal is to achieve an effective breathing pattern by reducing bronchial constriction and promoting relaxed breathing. This can be achieved by administering bronchodilators as prescribed, teaching the patient relaxation techniques, and monitoring respiratory rate and effort.
Interventions
Oxygen Therapy
If the patient has low oxygen saturation levels, oxygen therapy may be initiated. The nurse should ensure that the appropriate oxygen delivery device is used and monitor the patient’s oxygen saturation levels closely to maintain a target range. It is important to educate the patient on the proper use of oxygen therapy and the potential risks and benefits.
Airway Clearance Techniques
To promote effective airway clearance, the nurse should assist the patient with coughing and suctioning if necessary. Teaching the patient deep breathing exercises and huffing techniques can also help mobilize secretions and improve airway clearance. Fluid intake and humidification are additional interventions that can be used to facilitate the thinning and removal of mucus.
Breathing Exercises
Breathing exercises can help improve lung function and promote effective breathing patterns. The nurse should teach the patient techniques such as diaphragmatic breathing, pursed lip breathing, and incentive spirometry. Regular practice of these exercises can help strengthen respiratory muscles and improve oxygenation.
Medication Administration
Bronchodilators, such as beta-agonists and anticholinergics, are commonly used to relieve bronchial constriction and improve breathing in patients with bronchitis. The nurse should administer these medications as prescribed and closely monitor the patient for any adverse reactions or side effects. It is important to educate the patient about the purpose of these medications and how to use them correctly.
Patient Education
Self-care Techniques
Patient education plays a crucial role in managing bronchitis. The nurse should teach the patient self-care techniques, such as proper hand hygiene to prevent the spread of infection, and the importance of staying hydrated to help thin the mucus. It is also important to educate the patient about the need to quit smoking and avoid exposure to respiratory irritants to prevent exacerbations of bronchitis.
Medication Compliance
Compliance with medication regimens is essential for managing bronchitis effectively. The nurse should educate the patient about the prescribed medications, including their purpose, potential side effects, and proper administration techniques. It is important to emphasize the importance of taking medications as prescribed and following up with healthcare providers for any changes in symptoms.
Lifestyle Modifications
Lifestyle modifications can help prevent further respiratory issues and promote overall health. The nurse should educate the patient about the benefits of regular exercise, a healthy diet, and maintaining a smoke-free environment. It is important to assess the patient’s readiness to make these changes and provide support and resources as needed.
Monitoring and Evaluation
Respiratory Status
The nurse should continuously monitor the patient’s respiratory status, including respiratory rate, depth, and effort. Any changes in respiratory status, such as increased work of breathing or decreased breath sounds, should be promptly reported to the healthcare provider. The patient’s ability to effectively expectorate and maintain a patent airway should also be assessed regularly.
Oxygen Saturation
Monitoring oxygen saturation levels is essential to ensure adequate oxygenation of tissues. The nurse should use a pulse oximeter to regularly assess the patient’s oxygen saturation levels and maintain them within the target range. Any significant deviations from the target range should be reported promptly.
Breathing Patterns
Observing the patient’s breathing patterns can provide important information about their respiratory function. The nurse should monitor for any signs of increased respiratory rate, shallow breathing, or prolonged expiration. Improvement in breathing patterns, such as regular and effortless breaths, indicates progress in managing bronchitis.
Symptom Improvement
Monitoring and evaluating the patient’s overall symptom improvement is essential to gauge the effectiveness of interventions. The nurse should assess the patient’s cough, mucus production, chest discomfort, and shortness of breath regularly. Improvement in these symptoms indicates a positive response to treatment, while worsening or persistent symptoms may require further interventions or reassessment.
Collaborative Care
Medical Management
Collaborative care involves working with other healthcare professionals to provide comprehensive and coordinated care for patients with bronchitis. The nurse should collaborate with the healthcare provider to develop an individualized care plan, address any concerns, and ensure appropriate medication management. Regular communication and follow-up with the healthcare provider are essential to monitor the patient’s progress and make any necessary adjustments to the treatment plan.
Multidisciplinary Team Involvement
In severe cases of bronchitis, involvement of a multidisciplinary team may be necessary to provide specialized care. This may include respiratory therapists, physical therapists, nutritionists, and social workers. The nurse should work collaboratively with these team members to meet the specific needs of the patient and provide holistic care.
Referrals
Referrals to other healthcare professionals or services may be necessary to address specific aspects of bronchitis management. For example, a referral to a pulmonologist may be warranted if the patient’s bronchitis is severe or recurrent. The nurse should facilitate these referrals and ensure that the patient receives the appropriate care and resources.
Prevention Strategies
Vaccination
Vaccination plays a vital role in preventing infectious respiratory illnesses, such as influenza and pneumonia, which can exacerbate bronchitis. The nurse should educate patients about the importance of annual influenza vaccination and discuss the benefits of pneumococcal vaccination for those at high risk. It is important to debunk any myths or misconceptions surrounding vaccinations and provide evidence-based information.
Hand Hygiene
Hand hygiene is one of the most effective ways to prevent the spread of respiratory infections. The nurse should educate patients about proper handwashing techniques and the importance of frequent hand hygiene, especially during cold and flu seasons. Providing alcohol-based hand sanitizers at convenient locations can also promote compliance with hand hygiene practices.
Avoiding Irritants
Avoiding respiratory irritants, such as cigarette smoke and air pollutants, is essential in the prevention of bronchitis exacerbations. The nurse should educate patients about the harmful effects of smoking and provide resources and support for smoking cessation. Additionally, patients should be encouraged to minimize exposure to environmental pollutants and use appropriate protective measures when necessary.
Complications
Pneumonia
Pneumonia is a potential complication of bronchitis, especially in older adults and those with weakened immune systems. The nurse should monitor for signs and symptoms of pneumonia, such as high fever, increased cough with purulent sputum, and chest pain. Timely recognition and appropriate management of pneumonia can help prevent further respiratory complications.
Respiratory Failure
Severe cases of bronchitis can lead to respiratory failure if left untreated. The nurse should monitor for signs of respiratory distress, such as cyanosis, altered mental status, and increasing oxygen requirements. Prompt intervention, such as oxygen therapy and escalating respiratory support, should be initiated if respiratory failure is suspected.
Chronic Bronchitis
Chronic bronchitis is a long-term condition characterized by recurrent episodes of bronchial inflammation and mucus production. The nurse should educate patients with chronic bronchitis about the need for ongoing disease management, including regular follow-up appointments, medication compliance, and lifestyle modifications. Providing support and resources for self-management can help prevent exacerbations and improve the patient’s overall quality of life.
Ethical Considerations
Respecting Patient Autonomy
Respecting patient autonomy is essential in providing patient-centered care. The nurse should engage in open and respectful communication with the patient, ensuring that their preferences, values, and goals are considered in the decision-making process. Informed consent should be obtained before any invasive procedures or treatments are initiated.
Informed Consent
Obtaining informed consent is crucial in promoting patient autonomy and ensuring that the patient understands the risks, benefits, and alternatives to proposed interventions. The nurse should explain the purpose and potential outcomes of diagnostic tests, medications, and procedures in a clear and understandable manner. It is important to give the patient ample opportunity to ask questions and make informed decisions about their healthcare.
Confidentiality
Maintaining patient confidentiality is a fundamental ethical principle in healthcare. The nurse should ensure that all patient information is kept secure and only shared with authorized healthcare providers involved in the patient’s care. Respecting the patient’s privacy and confidentiality fosters trust in the nurse-patient relationship and upholds professional ethical standards.