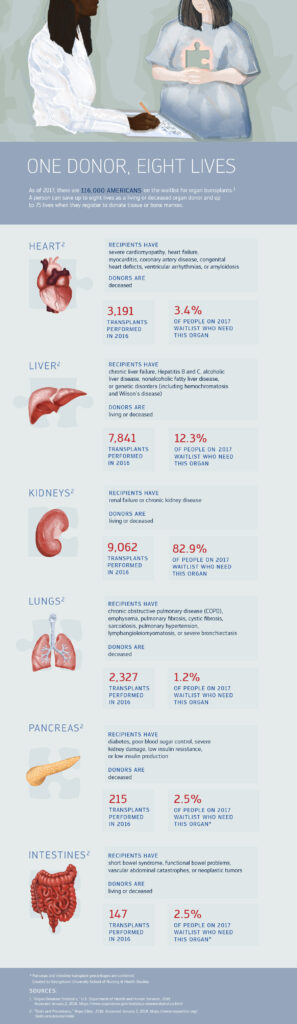
In the realm of healthcare, organ transplantation is a critical procedure that saves countless lives. As a nurse, it is essential to be well-versed in the important nursing considerations and nursing management for organ transplants. From pre-transplant assessment to postoperative care, understanding the unique challenges and intricacies of this process is crucial in ensuring the best possible outcomes for patients. This article delves into the key aspects that nurses should consider when caring for patients undergoing organ transplantation, providing valuable insights and guidance for providing optimal support and care throughout the journey.
Preoperative Nursing Considerations
Assessment of the recipient’s physical and emotional health
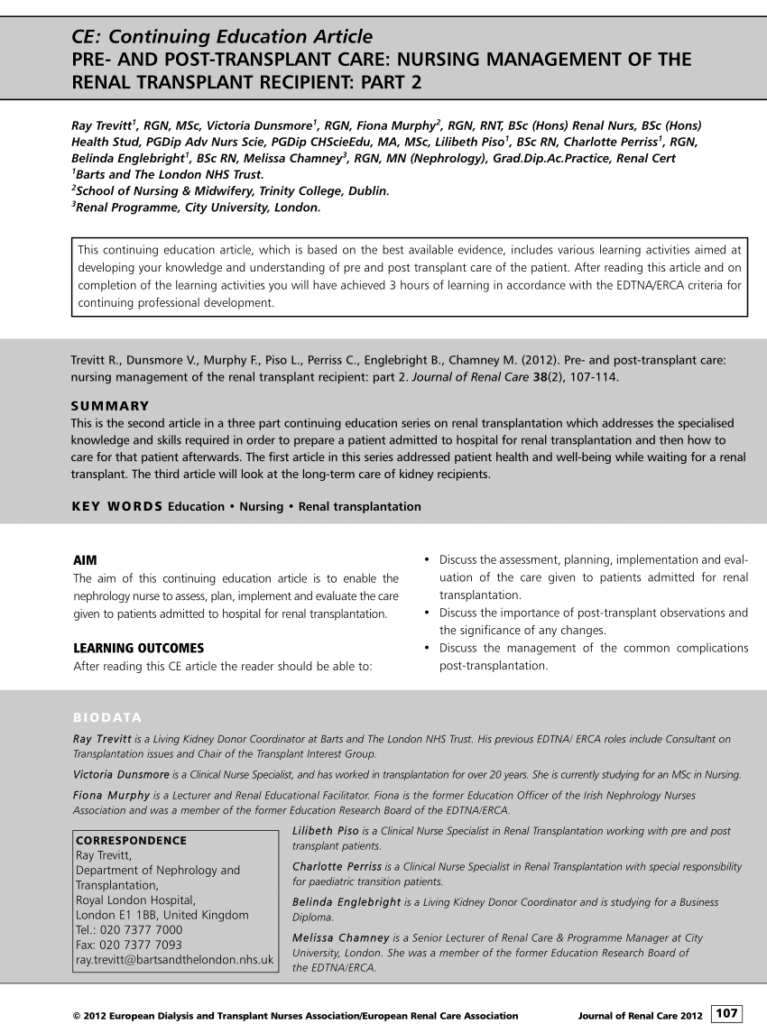
During the preoperative phase of organ transplantation, a thorough assessment of the recipient’s physical and emotional health is crucial. This assessment includes evaluating the recipient’s medical history, current medication use, and any underlying health conditions. It is important to identify any potential contraindications or risks that may affect the outcome of the transplant. Additionally, assessing the recipient’s emotional well-being and support system is essential to ensure they are mentally and emotionally prepared for the transplant process.
Evaluation of the recipient’s readiness for transplantation
Determining the recipient’s readiness for transplantation involves a comprehensive evaluation of their overall health status. This evaluation includes assessing the recipient’s organ function, laboratory values, and overall physical fitness. It is important to assess the recipient’s ability to tolerate the surgical procedure and the potential complications that may arise post-transplant. This evaluation helps in identifying any necessary interventions or adjustments in the care plan to optimize the recipient’s outcomes.
Education and counseling for the recipient and their family regarding the transplant process
Educating and counseling the recipient and their family about the transplant process is essential for their understanding and empowerment. It is important to provide comprehensive information about the procedure, potential risks and benefits, and the post-transplant care requirements. This education helps the recipient and their family make informed decisions, prepare for the surgery, and actively participate in their care plan. Additionally, providing emotional support and counseling throughout the process can help alleviate anxiety and promote a positive attitude towards the transplant.
Coordination of preoperative diagnostic tests and procedures
Coordinating preoperative diagnostic tests and procedures is a crucial aspect of preoperative nursing care for organ transplantation. This includes arranging and facilitating various tests, such as blood work, imaging studies, and cardiac evaluations, to ensure that the recipient is in optimal condition for the surgery. By coordinating these tests, nurses ensure that the recipient’s medical team has all the necessary information to make informed decisions regarding the transplant and plan for any potential complications.
Review of the recipient’s medical history and current medication use
A thorough review of the recipient’s medical history and current medication use is vital in the preoperative phase of organ transplantation. This review helps identify any medical conditions or medications that may impact the transplant surgery or postoperative care. It is important to assess the recipient’s medication regimen for drug interactions, adverse effects, and potential surgical complications. By reviewing the medical history and current medication use, nurses can collaborate with the healthcare team to optimize the recipient’s medication management and reduce the risk of complications.
Intraoperative Nursing Considerations
Preparation of the operating room and surgical equipment
Preparing the operating room and surgical equipment is essential to ensure a safe and efficient surgical procedure. Nurses play a critical role in setting up the operating room, sterilizing equipment, and ensuring that all the necessary tools and supplies are available. By meticulously preparing the operating room, nurses contribute to maintaining aseptic conditions, reducing the risk of infection, and ensuring a smooth surgical process.
Assistance with induction of anesthesia and positioning of the recipient
Assisting with the induction of anesthesia and positioning the recipient is a vital role for nurses during organ transplantation. Nurses collaborate with the anesthesia team to ensure the safe administration of anesthesia and monitor the recipient’s vital signs during the induction process. Proper positioning of the recipient on the operating table is crucial to facilitate optimal access to the surgical site and minimize the risk of complications. Nurses provide assistance and support to ensure the recipient’s comfort and safety during this phase of the procedure.
Monitoring of vital signs and response to anesthesia during the procedure
Monitoring the recipient’s vital signs and response to anesthesia is a crucial responsibility of intraoperative nurses. Throughout the surgical procedure, nurses continuously monitor the recipient’s heart rate, blood pressure, oxygen saturation, and other vital signs to identify any deviations from the norm. They also closely observe the recipient’s response to anesthesia, ensuring that they are maintaining appropriate levels of anesthesia and are free from any adverse reactions or complications.
Collaboration with the surgical team to ensure aseptic technique and surgical site integrity
Collaborating with the surgical team is imperative to maintain aseptic technique and preserve surgical site integrity during organ transplantation. Intraoperative nurses work closely with the surgical team to ensure proper sterility measures are followed, such as scrubbing in, donning sterile attire, and maintaining a sterile field. By actively participating in maintaining aseptic conditions, nurses help reduce the risk of surgical site infections and promote optimal outcomes for the recipient.
Documentation and communication of intraoperative events
Accurate and timely documentation of intraoperative events is essential for continuity of care and legal purposes. Intraoperative nurses meticulously record and communicate important information, such as vital signs, anesthesia administration, surgical interventions, and any changes in the recipient’s condition. This documentation helps facilitate effective communication among the healthcare team, ensures smooth transitions of care, and provides a comprehensive record of the surgical procedure for future reference.
Postoperative Nursing Considerations
Assessment of postoperative recipient status, including vital signs and surgical site appearance
The postoperative assessment of the recipient’s status is a crucial aspect of nursing care after organ transplantation. Nurses regularly assess the recipient’s vital signs, such as heart rate, blood pressure, respiratory rate, and oxygen saturation, to monitor their overall stability and detect any signs of potential complications. Additionally, nurses carefully observe the appearance of the surgical site for signs of infection, hematoma, or any other abnormalities that may require immediate attention.
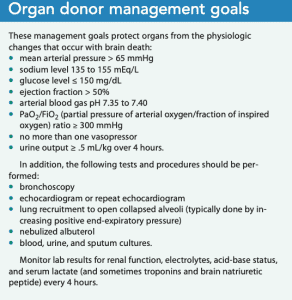
Monitoring of fluid and electrolyte balance, hemodynamics, and laboratory values
Monitoring the recipient’s fluid and electrolyte balance, hemodynamics, and laboratory values is essential for optimal postoperative care. Nurses closely monitor the recipient’s intake and output, as well as their electrolyte levels, to ensure adequate hydration and prevent complications such as dehydration or fluid overload. Additionally, nurses assess the recipient’s hemodynamic parameters, such as blood pressure and cardiac output, to monitor their cardiovascular stability. Regular monitoring of laboratory values, including renal function and immunosuppressive medication levels, helps identify any abnormalities and allows for timely interventions.
Pain assessment and management
Assessing and managing pain is a crucial aspect of postoperative nursing care for organ transplantation. Nurses use standardized pain assessment tools and closely monitor the recipient’s self-reported pain levels to ensure optimal pain management. This includes administering appropriate pain medications, both pharmacological and non-pharmacological, as prescribed and evaluating their efficacy. By effectively managing pain, nurses promote the recipient’s comfort, facilitate early mobility, and enhance their overall recovery process.
Administration of immunosuppressive medications and monitoring for adverse effects
Administering immunosuppressive medications and closely monitoring for adverse effects is a vital nursing responsibility in the postoperative period of organ transplantation. Nurses ensure timely and accurate administration of these medications, strictly following the prescribed regimen and monitoring the recipient’s response. This includes assessing for signs of medication side effects, such as infection, gastrointestinal disturbances, or renal dysfunction. By closely monitoring immunosuppressive medication use, nurses help prevent rejection episodes, detect and manage potential complications, and promote the recipient’s long-term graft survival.
Wound care and infection prevention
Providing appropriate wound care and infection prevention strategies is crucial for the recipient’s postoperative recovery. Nurses meticulously assess the surgical incision site, clean and dress the wound following aseptic techniques, and assess for any signs of infection or complications. Careful monitoring, early detection, and prompt intervention in case of any wound-related issues help prevent infection and ensure optimal healing. Nurses also educate the recipient and their family on proper wound care techniques, signs of infection, and the importance of adhering to the prescribed care plan to minimize the risk of complications.
Psychosocial Considerations
Support and counseling for the recipient and their family throughout the transplant process
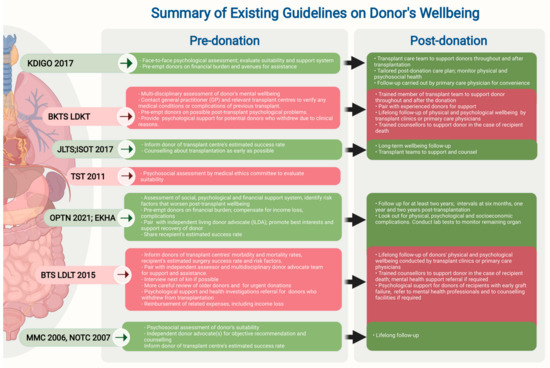
Supporting and counseling the recipient and their family throughout the transplant process is crucial for their emotional well-being and overall adaptation. Nurses provide empathetic and non-judgmental support, actively listening to their concerns and addressing their emotional needs. By providing emotional support and counseling, nurses help alleviate anxiety, stress, and fears associated with the transplant process, facilitating a positive psychological environment.
Evaluation of the recipient’s coping mechanisms and emotional well-being
Evaluating the recipient’s coping mechanisms and emotional well-being is important to identify any challenges or potential psychological issues they may encounter during the transplant process. Nurses assess the recipient’s coping strategies and mental health, addressing any signs of anxiety, depression, or other psychological distress. By identifying and promoting healthy coping mechanisms, nurses provide the recipient with the tools and support they need to navigate the emotional challenges of organ transplantation.
Assistance with coordination of support services and resources after transplantation
Assisting with the coordination of support services and resources after transplantation is crucial to ensure the recipient’s successful transition to their new life post-transplant. nurses collaborate with social workers, psychologists, and other healthcare professionals to help the recipient and their family access appropriate support networks, such as support groups, counseling services, and financial assistance programs. This coordinated effort enhances the recipient’s psychosocial well-being and facilitates their overall adaptation to life after transplantation.
Addressing the potential for organ rejection and its impact on the recipient’s mental health
Addressing the potential for organ rejection and its impact on the recipient’s mental health is a vital aspect of psychosocial nursing care during organ transplantation. Nurses provide education and emotional support to help the recipient understand the signs and symptoms of rejection, the importance of medication adherence, and the role they play in managing their own health. By addressing the potential for rejection and offering ongoing support, nurses help alleviate anxiety and empower the recipient to take an active role in their post-transplant care.
Collaboration with social workers and psychologists to ensure holistic care
Collaborating with social workers and psychologists is crucial to ensure holistic care for the recipient throughout the transplant process. Nurses work closely with these professionals to assess and address the recipient’s social, emotional, and financial needs. They help facilitate appropriate referrals for counseling, financial assistance programs, and other support services to enhance the recipient’s overall well-being and ensure a successful transition to life post-transplant.
Complications and Emergency Management
Recognition and prompt intervention for signs of rejection, infection, or graft failure
Prompt recognition and intervention for signs of rejection, infection, or graft failure are essential to prevent further complications and ensure timely treatment. Nurses carefully monitor the recipient for any symptoms or laboratory findings that may indicate rejection, infection, or graft failure. In collaboration with the healthcare team, they promptly initiate appropriate interventions, such as adjusting immunosuppressive medications or administering antibiotics, to mitigate the risk and minimize the impact of these complications.
Administration of emergency medications and interventions to stabilize the recipient
In emergency situations, nurses play a critical role in administering necessary medications and interventions to stabilize the recipient. This may include administering emergency medications, such as vasopressors or antiarrhythmics, to maintain stable hemodynamics or initiating advanced life support measures if needed. Nurses are trained to respond quickly, efficiently, and calmly in these situations, ensuring the recipient’s safety and optimizing their chances of recovery.
Communication and collaboration with the transplant team in emergency situations
Effective communication and collaboration with the transplant team are vital in emergency situations. Nurses promptly communicate any changes in the recipient’s condition, initiate appropriate interventions, and collaborate with the transplant team to develop a comprehensive plan of care. This collaboration ensures a seamless response to emergency situations, facilitates timely decision-making, and optimizes the recipient’s outcomes.
Educating the recipient and their family on signs and symptoms of potential complications
Nurses play a crucial role in educating the recipient and their family about the signs and symptoms of potential complications. By providing comprehensive education, nurses empower the recipient and their family to recognize early warning signs and seek appropriate medical attention. This education includes information on infection symptoms, signs of organ rejection, and the importance of adhering to the prescribed medication regimen. By promoting early recognition and intervention, nurses help prevent further complications and facilitate better outcomes for the recipient.
Determining appropriate interventions during emergency situations
In emergency situations, nurses must quickly assess the recipient’s condition and determine appropriate interventions. This may involve initiating cardiopulmonary resuscitation (CPR), administering medications, or preparing for urgent surgical interventions. Nurses are trained to think critically and promptly respond to emergent situations, ensuring the recipient receives the necessary care in a timely manner and potentially preventing further deterioration.
Ethical Issues in Organ Transplantation
Understanding the ethical considerations surrounding organ allocation and transplantation
Understanding the ethical considerations surrounding organ allocation and transplantation is essential for nurses providing care to organ transplant recipients. Nurses should have knowledge of the ethical principles (autonomy, beneficence, non-maleficence, and justice) guiding organ transplantation and be familiar with the policies and guidelines governing organ allocation. This understanding enables nurses to advocate for equitable and ethical practices throughout the transplant process and ensure the recipient’s rights and well-being are respected.
Advocacy for equitable organ allocation and the promotion of ethical practices
Nurses are advocates for equitable organ allocation and the promotion of ethical practices in organ transplantation. They play a vital role in ensuring fair and transparent organ allocation processes are followed, while also advocating for the recipient’s best interests. Nurses collaborate with the healthcare team to address any conflicts or concerns related to organ allocation, ethically navigating challenging situations and promoting equitable care.
Addressing conflicts of interest and ensuring transparency in the transplantation process
Addressing conflicts of interest and ensuring transparency in the transplantation process is a crucial ethical consideration for nurses. They actively promote transparency in organ allocation decisions, ensuring open communication with the recipient and their family regarding the process. Nurses also collaborate with the healthcare team to identify and manage any conflicts of interest, ensuring that the recipient’s best interests are prioritized and their care is not compromised.
Informed consent and patient autonomy in decision-making
Respecting the recipient’s autonomy and obtaining informed consent are fundamental ethical principles in organ transplantation. Nurses advocate for the recipient’s right to make informed decisions regarding their care, ensuring they have a clear understanding of the benefits, risks, and alternatives of organ transplantation. Nurses facilitate the informed consent process by providing comprehensive education, answering questions, and addressing any concerns or ambiguities raised by the recipient and their family.
Supporting the recipient and their family during ethical dilemmas
Ethical dilemmas can arise during the organ transplantation process, and nurses play a vital role in supporting the recipient and their family during these challenging situations. Nurses provide emotional support, actively listen to the concerns and values of the recipient and their family, and help navigate the decision-making process. By offering guidance and empathy, nurses help the recipient and their family resolve ethical dilemmas while ensuring their welfare and well-being are prioritized.
Cultural Considerations
Respecting cultural beliefs and practices regarding organ donation and transplantation
Respecting cultural beliefs and practices regarding organ donation and transplantation is crucial in providing culturally sensitive care. Nurses recognize and respect the diversity of cultural beliefs and practices, ensuring that the recipient’s cultural values are incorporated into their care plan. By understanding and respecting cultural beliefs surrounding organ donation and transplantation, nurses promote trust, effective communication, and holistic care.
Collaboration with interpreters and cultural liaisons to facilitate effective communication
Collaboration with interpreters and cultural liaisons is essential to facilitate effective communication with recipients from diverse cultural backgrounds. Nurses work closely with interpreters and cultural liaisons to bridge language and cultural barriers, ensuring accurate exchange of information, and promoting culturally sensitive care. By ensuring effective communication, nurses can provide optimal care tailored to the recipient’s cultural needs and preferences.
Educating healthcare providers on cultural competence and sensitivity in transplant care
Educating healthcare providers on cultural competence and sensitivity in transplant care is critical to ensure culturally appropriate care for recipients. Nurses play a key role in providing education on cultural competence, encouraging healthcare providers to expand their cultural knowledge and challenge biases or stereotypes. By promoting cultural competence, nurses contribute to a more inclusive and respectful healthcare environment for recipients from different cultural backgrounds.
Adapting nursing care plans to meet the cultural needs and preferences of the recipient
Adapting nursing care plans to meet the cultural needs and preferences of the recipient is essential in providing individualized care. Nurses embrace a patient-centered approach, tailoring care plans to incorporate the recipient’s cultural values, beliefs, and practices. By adapting care plans to respect cultural diversity, nurses enhance the recipient’s comfort, adherence to the care plan, and overall satisfaction with their healthcare experience.
Promoting cultural diversity and inclusion in the transplantation setting
Promoting cultural diversity and inclusion in the transplantation setting is vital to foster an environment of respect and acceptance. Nurses actively engage in promoting cultural diversity by encouraging the celebration of different cultural traditions and beliefs. By fostering a culturally inclusive environment, nurses contribute to creating a supportive and collaborative healthcare setting for both recipients and healthcare providers.
Transition to Long-Term Care
Preparing the recipient and their family for the transition to long-term care
Preparing the recipient and their family for the transition to long-term care is crucial to ensure a smooth and successful transition. Nurses provide comprehensive education on the recipient’s post-transplant care plan, including medication management, follow-up appointments, and lifestyle modifications. They also address any concerns or questions the recipient and their family may have, promoting their confidence and readiness to assume responsibility for their ongoing care.
Coordination of home healthcare services and follow-up appointments
Coordinating home healthcare services and follow-up appointments is essential to support the recipient’s long-term care. Nurses collaborate with home healthcare agencies to ensure a seamless transition from the hospital to home care. They also assist the recipient in scheduling and coordinating necessary follow-up appointments with the transplant team, ensuring continuity of care and ongoing monitoring of the recipient’s progress.
Education on self-care management, including medication adherence and monitoring
Education on self-care management is crucial to empower the recipient to actively participate in their post-transplant care. Nurses provide detailed instruction on medication adherence, including proper dosing, administration, and potential side effects. They also educate the recipient on monitoring techniques, such as self-assessment of vital signs and infection symptoms, enabling them to recognize and report any abnormalities promptly. By promoting self-care management, nurses support the recipient’s independence and long-term graft health.
Counseling on lifestyle modifications and the importance of ongoing healthcare surveillance
Counseling on lifestyle modifications and the importance of ongoing healthcare surveillance is essential for the recipient’s long-term well-being. Nurses provide guidance on healthy lifestyle behaviors, such as regular exercise, balanced nutrition, and smoking cessation, to optimize the recipient’s overall health and minimize the risk of complications. They also emphasize the significance of ongoing healthcare surveillance, including routine check-ups, laboratory tests, and immunosuppressive medication monitoring, to ensure early detection and management of any issues.
Supporting the recipient in maintaining a high quality of life post-transplant
Supporting the recipient in maintaining a high quality of life post-transplant is a paramount nursing goal. Nurses provide ongoing support, guidance, and resources to assist the recipient in adapting to life after transplantation. They address any challenges or concerns the recipient may have and help them find ways to enjoy activities that contribute to their overall well-being. By supporting the recipient in maintaining a high quality of life, nurses empower them to live their lives to the fullest and fully embrace the opportunities granted by transplantation.

Interprofessional Collaboration
Effective communication and collaboration with the multidisciplinary transplant team
Effective communication and collaboration with the multidisciplinary transplant team is essential for providing comprehensive care to organ transplant recipients. Nurses actively engage in interdisciplinary rounds and meetings, effectively communicating the recipient’s progress, care needs, and any changes in their condition. This collaboration ensures continuity of care, promotes shared decision-making, and enhances the overall outcomes for the recipient.
Participation in interdisciplinary rounds and meetings to ensure coordinated care
Participation in interdisciplinary rounds and meetings allows nurses to contribute their unique perspective and advocate for the recipient’s needs within the healthcare team. Nurses actively engage in discussions regarding the recipient’s care plan, challenges, and goals, actively collaborating with other healthcare professionals to ensure coordinated and holistic care. Their input helps facilitate optimal care outcomes and promotes a patient-centered approach to care.
Advocating for the recipient’s needs and preferences within the healthcare team
Nurses serve as advocates for the recipient’s needs and preferences within the healthcare team. By actively communicating the recipient’s desires and concerns, nurses ensure that their preferences are considered in the development of the care plan and decision-making. By advocating for their needs, nurses help bridge any communication gaps between the recipient and the healthcare team, fostering a collaborative and patient-centered approach to care.
Collaboration with pharmacists, nutritionists, and physical therapists for comprehensive care
Collaboration with pharmacists, nutritionists, and physical therapists is crucial to provide comprehensive care to organ transplant recipients. Nurses work closely with these professionals to ensure medication management, optimize nutritional status, and promote physical rehabilitation. This collaborative approach ensures that the recipient receives individualized care that addresses their specific needs and maximizes their overall recovery and well-being.
Inclusion of the recipient and their family as active members of the healthcare team
Inclusion of the recipient and their family as active members of the healthcare team is essential for patient-centered care. Nurses encourage the recipient and their family to actively participate in care planning, self-management, and decision-making processes. By involving them as active members of the healthcare team, nurses foster a collaborative and empowering environment, resulting in improved satisfaction, adherence to the care plan, and overall outcomes for the recipient.
Professional Development and Education
Continuing education on advancements in organ transplantation and nursing practices
Continuing education on advancements in organ transplantation and nursing practices is essential for nurses providing care to organ transplant recipients. Nurses actively seek opportunities for professional development, attending conferences, seminars, and workshops focused on transplant nursing. By staying abreast of the latest research, clinical guidelines, and innovations in transplantation, nurses enhance their knowledge and skills, ensuring the provision of safe and evidence-based care.
Engagement in professional organizations and networks for knowledge exchange
Engagement in professional organizations and networks is valuable for knowledge exchange and professional growth. Nurses actively participate in organ transplant nursing associations and networks, collaborating with colleagues to share best practices, challenge each other’s thinking, and learn from collective experiences. By engaging in professional organizations and networks, nurses contribute to advancements in the field and continuously enhance their transplant nursing practice.
Participation in research initiatives and evidence-based practice development
Participating in research initiatives and evidence-based practice development is essential for nurses to contribute to the growth and improvement of transplant nursing care. Nurses actively seek opportunities to participate in research studies, quality improvement projects, and evidence-based practice initiatives. By collecting and analyzing data, implementing evidence-based interventions, and disseminating findings, nurses enhance the scientific basis of transplant nursing care and facilitate continuous improvement.
Self-reflection and ongoing professional growth to enhance transplant nursing skills
Self-reflection and ongoing professional growth are essential for nurses to enhance their transplant nursing skills. Nurses regularly reflect on their practice, seeking feedback from colleagues and supervisors, and engaging in self-directed learning. By identifying areas of improvement and actively pursuing professional growth, nurses enhance their skills, competence, and confidence in providing high-quality care to organ transplant recipients.
Mentoring and precepting for aspiring transplant nurses
Mentoring and precepting aspiring transplant nurses are vital roles that experienced transplant nurses play in professional development. They provide guidance, support, and mentorship to new nurses entering the field, sharing their knowledge and wisdom. Through mentorship and precepting, experienced nurses inspire and empower the next generation of transplant nurses, ensuring the continuity of expert care for organ transplant recipients.