Imagine the incredible journey of a child who has battled and overcome Acute Lymphoblastic Leukemia (ALL). This journey not only requires immense strength and resilience but also leaves a lasting impact on their long-term health and well-being. In this article, we will explore the survivorship and long-term effects of ALL in children, shedding light on the challenges they may face even after conquering this formidable disease. From potential physical and psychological effects to strategies for support and care, join us as we delve into the world of survivorship in ALL patients, providing a compassionate and informative perspective.
Introduction
Welcome to this comprehensive article on survivorship and long-term effects of Acute Lymphoblastic Leukemia (ALL) in children. In recent years, there have been significant improvements in the survival rates for children diagnosed with ALL, which is the most common type of childhood cancer. However, being a survivor comes with its own set of challenges, both physically and emotionally. In this article, we will explore the improvements in survival rates, the challenges faced by survivors, and the psychosocial impact of survivorship. We will also delve into the long-term effects of ALL, including the physical, cognitive, and emotional effects that survivors may experience. Additionally, we will discuss the importance of monitoring and interventions to mitigate the long-term effects of ALL, as well as promote survivorship. Finally, we will explore the current research and future directions in this field, aiming to enhance the quality of life for survivors of childhood ALL.
Survivorship
Improvements in survival rates
Over the past few decades, there have been remarkable advancements in the treatment and management of childhood ALL, leading to significantly improved survival rates. In the 1960s, the overall survival rate for childhood ALL was merely 10%. However, with the development of more effective chemotherapy regimens and supportive care strategies, the survival rate has now increased to approximately 90%. This incredible progress can be attributed to a combination of factors, including multi-agent chemotherapy protocols, better risk stratification, the use of targeted therapies, and improved supportive care measures.
Challenges faced by survivors
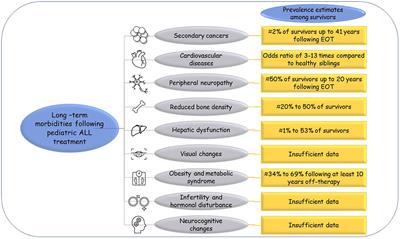
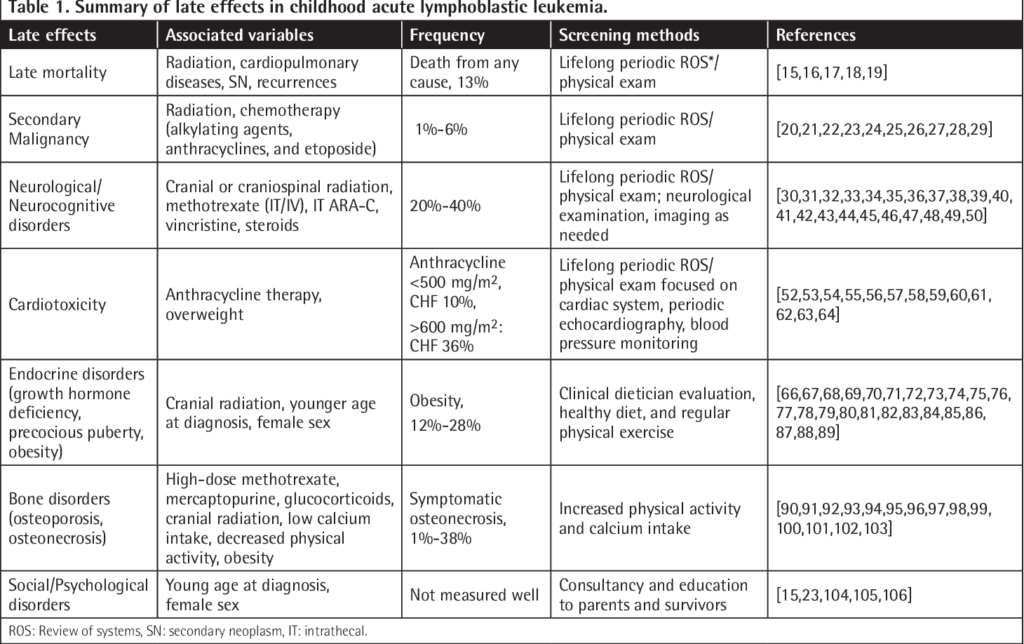
While the increasing survival rates are undoubtedly a cause for celebration, survivors of childhood ALL face a myriad of challenges in their post-treatment journey. One of the primary challenges is the risk of relapse or the development of secondary cancers later in life. Long-term survivors also encounter various physical, cognitive, and emotional effects that may impact their overall well-being. Additionally, survivors often face difficulties in transitioning back to their normal lives, such as reintegrating into school or finding employment. It is crucial to acknowledge and address these challenges to ensure the holistic well-being of childhood ALL survivors.
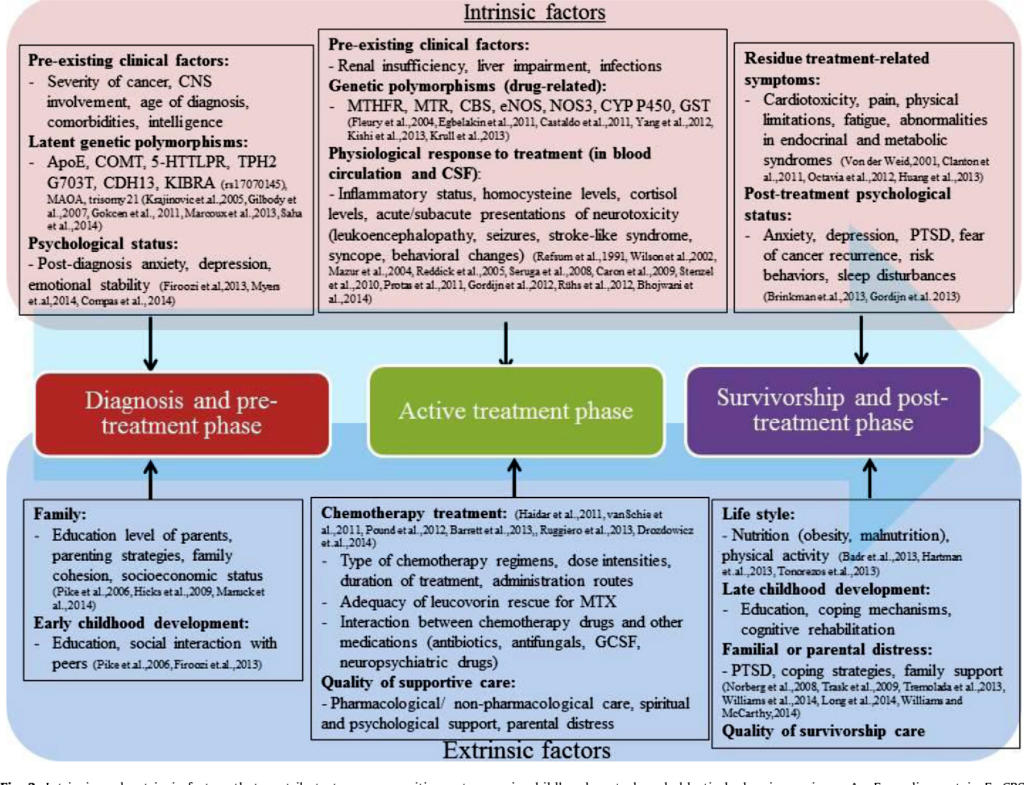
Psychosocial impact of survivorship
Survivorship can have a profound psychosocial impact on individuals who have been through the experience of childhood. Survivors may struggle with anxiety, depression, and post-traumatic stress disorder (PTSD) due to the traumatic nature of their diagnosis and treatment. The fear of relapse, which can persist throughout their lives, can also contribute to emotional distress. It is important to provide comprehensive psychosocial support and counseling to help survivors navigate these challenges and promote their mental health and well-being.
Long-term Effects
Physical effects
Childhood ALL and its treatment can have lasting physical effects on survivors. These effects can manifest in various ways, such as late effects on growth and development, organ damage, and the development of chronic health conditions. Survivors may experience growth abnormalities, such as stunted growth or delayed puberty. Organ damage, particularly to the heart, lungs, and reproductive system, can occur as a result of certain chemotherapy agents or radiation therapy. Additionally, survivors have an increased risk of developing chronic health conditions, including cardiovascular disease, osteoporosis, and fertility issues.
Cognitive effects
The treatment of childhood ALL can also impact the cognitive functioning of survivors. Neurocognitive deficits, such as difficulties with attention, memory, and executive functioning, have been observed in a significant portion of survivors. These deficits can manifest in academic settings, leading to challenges in learning and may necessitate special educational accommodations. Learning disabilities, such as dyslexia or dyscalculia, are also more prevalent in survivors of childhood ALL. The cognitive effects of ALL treatment highlight the importance of providing appropriate support and accommodations to optimize the educational outcomes of survivors.
Emotional effects
Survivors of childhood often grapple with a range of emotional effects that can stem from their cancer experience. Anxiety and depression are commonly reported among survivors, possibly due to the traumatic nature of the diagnosis, treatment, and the uncertainty of the future. Additionally, PTSD may develop as survivors cope with the emotional scars left by their cancer journey. The fear of relapse can also contribute to heightened anxiety levels. Recognizing and addressing these emotional effects is essential to support survivors in maintaining their emotional well-being and overall quality of life.
Physical Effects
Late effects on growth and development
One of the physical long-term effects of childhood ALL treatment is the impact on growth and development. Certain chemotherapy agents and radiation therapy can lead to delayed growth, resulting in shorter stature or delayed puberty. Endocrine dysfunction, such as thyroid abnormalities or adrenal insufficiency, may also affect growth and development in survivors. Regular monitoring and appropriate interventions, such as hormone replacement therapies, can help mitigate these late effects and promote healthy growth and development.
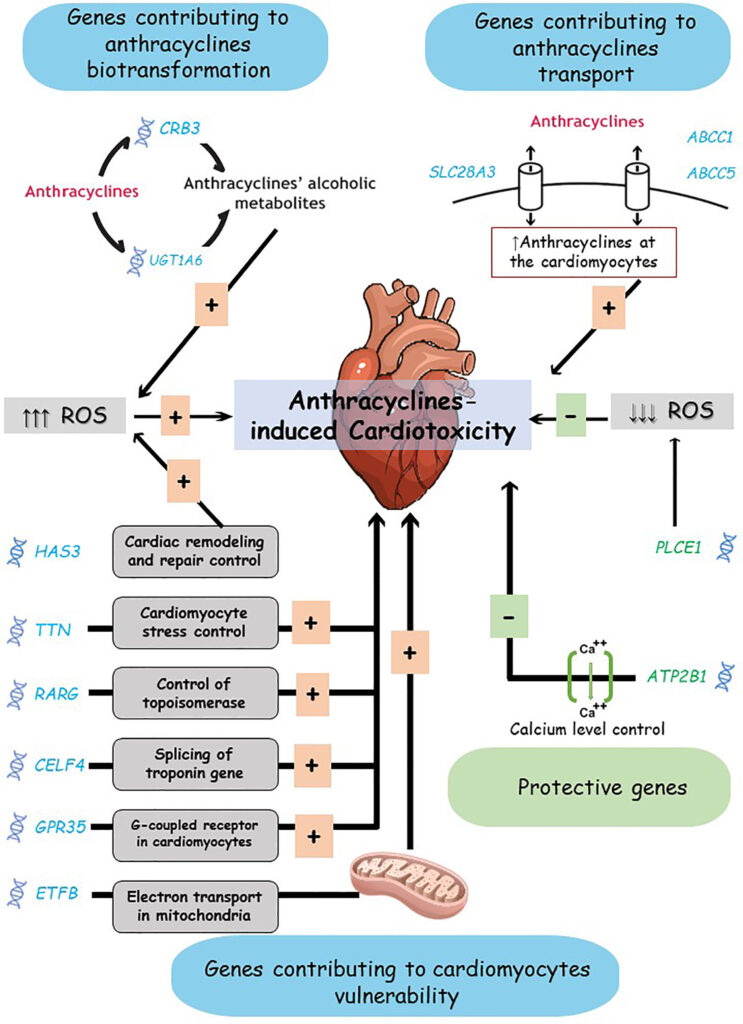
Organ damage and chronic health conditions
Childhood ALL treatment, particularly intensive chemotherapy and radiation therapy, can cause damage to vital organs, leading to the development of chronic health conditions. The heart, lungs, and reproductive organs are particularly vulnerable to the toxic effects of treatment. Survivors may experience cardiac abnormalities, pulmonary fibrosis, or compromised fertility. It is imperative to closely monitor survivors for signs of organ damage and provide appropriate medical interventions to minimize the long-term consequences on their health.
Impaired immune system function
ALL treatment can also impair the immune system function of survivors, increasing their susceptibility to infections. Chemotherapy drugs can cause temporary suppression of the immune system, making survivors more vulnerable to bacterial and viral infections. Some treatment protocols may also have long-term effects on immune function, resulting in immunodeficiency disorders. Regular monitoring of immune function and appropriate preventive measures, such as vaccinations and prophylactic antibiotics, can help safeguard the health of survivors.
Cognitive Effects
Impact on academic performance
The cognitive effects of childhood ALL treatment can impact the academic performance of survivors. Neurocognitive deficits, including difficulties with attention, memory, and executive functioning, can affect learning and information processing. Survivors may experience challenges in keeping up with the curriculum or learning at the same pace as their peers. It is crucial for educators and parents to be aware of these cognitive effects and provide necessary accommodations, such as extra time for exams or individualized learning plans, to support the educational needs of survivors.
Neurocognitive deficits
Research has shown that a significant proportion of childhood ALL survivors exhibit neurocognitive deficits, which can manifest in various ways. Attention deficits, difficulties with working memory, and impaired executive functioning are commonly observed in survivors. These deficits may result from the direct effects of chemotherapy and radiation therapy on the developing brain, as well as the neurotoxicity of certain treatment agents. Early identification of neurocognitive deficits and the provision of targeted interventions, such as cognitive rehabilitation programs, can help mitigate the long-term cognitive effects and enhance the cognitive functioning of survivors.
Learning disabilities
In addition to general neurocognitive deficits, survivors of childhood ALL may also be at a higher risk of developing learning disabilities. Conditions such as dyslexia, dyscalculia, or specific language impairments may be more prevalent in this population. Learning disabilities can further impact academic achievement and learning outcomes. Early identification through comprehensive neuropsychological assessments and the implementation of appropriate educational support, such as specialized education programs or accommodations, can significantly improve the educational experience and success of survivors.
Emotional Effects
Anxiety and depression
Surviving childhood ALL can elicit significant emotional distress, including anxiety and depression. The traumatic experience of the diagnosis and treatment, coupled with the uncertainty of the future and fear of relapse, can contribute to heightened anxiety levels among survivors. Additionally, the emotional and physical side effects of treatment can impact mood and lead to depressive symptoms. It is vital to provide survivors with access to mental health resources, such as counseling or therapy, to address and manage anxiety and depression effectively.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is another emotional impact that childhood ALL survivors may experience. The traumatic nature of the diagnosis, the invasive medical procedures, and the emotional toll of facing mortality can leave lasting emotional scars. Symptoms of PTSD, such as intrusive memories, avoidance behaviors, and hyperarousal, may persist long after treatment. Early detection and appropriate interventions, such as trauma-focused therapies, can help survivors manage and heal from their traumatic experiences.
Fear of relapse
One of the most significant emotional challenges for childhood survivors is the fear of relapse. Being in remission does not eliminate the fear of cancer returning, which can be a constant source of anxiety and distress for survivors. The fear of relapse can impact various aspects of life, including relationships, decision-making, and long-term planning. Providing survivors with adequate psychosocial support, information, and resources can help them navigate this fear and promote their emotional well-being.
Late Effects Monitoring
Regular medical check-ups
Regular medical check-ups are crucial for monitoring and managing the long-term effects of childhood ALL. Survivors should undergo comprehensive physical examinations, including cardiac assessments, lung function tests, and hormonal evaluations, among others. These check-ups allow healthcare providers to identify and address any potential late effects early, leading to better outcomes and improved quality of life for survivors. Collaborative efforts between oncologists, pediatricians, and other specialists are essential in providing holistic and comprehensive care to survivors.
Screening for secondary cancers
Survivors of childhood ALL have an increased risk of developing secondary cancers later in life, making regular screening an integral part of their long-term follow-up care. These screenings typically include monitoring for solid tumors, such as breast, lung, or colon cancers, as well as blood-related malignancies. The frequency and type of screenings may vary based on individual risk factors and treatment history. Early detection through appropriate screening protocols can significantly improve the prognosis and survival rates of secondary cancers in survivors.
Assessment of psychosocial well-being
In addition to physical monitoring, assessing the psychosocial well-being of childhood ALL survivors is of paramount importance. Regular evaluations for emotional well-being, including anxiety, depression, and PTSD symptoms, should be incorporated into the follow-up care. Tools such as validated questionnaires or interviews can help healthcare providers identify areas of concern and offer appropriate support and interventions. Collaborating with mental health professionals and providing access to counseling services or support groups can further enhance the psychosocial well-being of survivors.
Interventions and Support
Physical rehabilitation
Physical rehabilitation plays a vital role in supporting survivors in regaining and maintaining their physical well-being. Survivors may benefit from various interventions, such as physiotherapy, occupational therapy, or exercise programs, to address any functional limitations resulting from their cancer treatment. These interventions can improve strength, endurance, and overall functional abilities, allowing survivors to lead more independent and fulfilling lives. It is essential for healthcare providers to assess and provide appropriate referrals for physical rehabilitation services based on individual needs.
Special education programs
Given the cognitive and academic challenges that childhood survivors may face, access to special education programs is crucial. These programs can provide tailored support, accommodations, and individualized learning plans to address the specific educational needs of survivors. Special education teachers and professionals can work closely with survivors and their families to identify areas of difficulty and implement strategies for academic success. By providing an inclusive and supportive educational environment, special education programs can empower survivors to reach their full potential.
Counseling and support groups
Psychosocial support is paramount in promoting the emotional well-being of childhood survivors. Counseling and therapy services can provide a safe space for survivors to express their feelings, address anxiety or depression, and develop coping strategies. Support groups specifically designed for childhood ALL survivors offer the opportunity for peer support, shared experiences, and a sense of belonging. The presence of a strong support network, whether through professional counseling or support groups, can significantly enhance the emotional resilience and overall quality of life of survivors.
Promoting Survivorship
Early detection and diagnosis
Early detection and diagnosis play a crucial role in promoting survivorship and positive treatment outcomes for children with ALL. Timely medical intervention allows for prompt initiation of curative treatments, increasing the chances of successfully eradicating the cancer. Awareness campaigns to educate parents, healthcare providers, and the general public about the early warning signs of ALL can facilitate early detection and ensure children are diagnosed at the earliest possible stage. Early diagnosis sets the foundation for a more hopeful and optimistic prognosis for childhood ALL survivors.
Improved treatment protocols
Continuous research and improvement in treatment protocols have contributed to the remarkable increase in survival rates for childhood ALL. The refinement of chemotherapy regimens, the introduction of targeted therapies, and advancements in supportive care measures have all played a critical role in enhancing treatment outcomes. Improved treatment protocols not only increase the chances of cure but also aim to minimize the long-term physical and cognitive effects of treatment. By constantly striving for better treatment options, we can continue to improve the overall survivorship experience for children with ALL.
Enhanced survivorship care
Ensuring comprehensive and holistic care throughout the survivorship journey is crucial for promoting the long-term health and well-being of childhood ALL survivors. Enhanced survivorship care involves the coordination of various healthcare providers, including oncologists, primary care physicians, psychologists, and specialists in late effects monitoring. Collaborative efforts among these professionals allow for the continuity of care, monitoring for late effects, and addressing survivors’ physical and emotional needs. By providing survivorship care that is tailored to the unique needs of childhood ALL survivors, we can optimize their quality of life and overall outcomes.
Research and Future Directions
Long-term follow-up studies
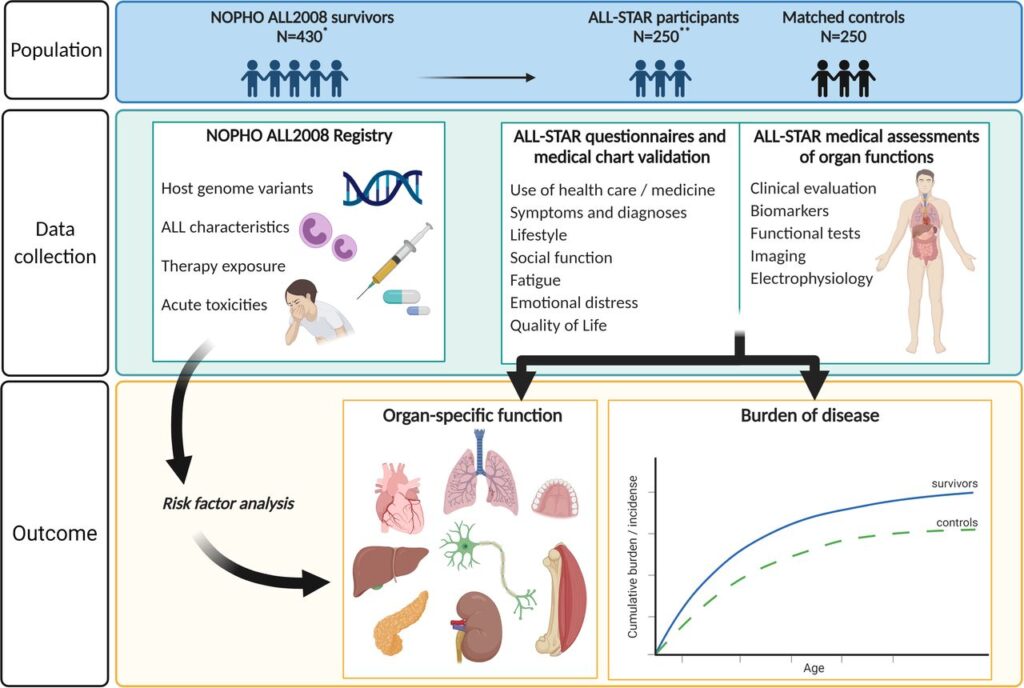
Ongoing research and long-term follow-up studies are essential in understanding the comprehensive impact of childhood ALL and its treatments on survivors. These studies evaluate the long-term physical, cognitive, and emotional effects experienced by survivors, allowing for evidence-based interventions and support strategies. Furthermore, long-term follow-up studies help identify risk factors for late effects, inform screening protocols, and guide survivorship care guidelines. Continued research in this field is instrumental in improving the long-term outcomes and quality of life for childhood ALL survivors.
Advancing treatment options
Advancing treatment options is a crucial aspect of future directions in childhood ALL research. Continued efforts to develop novel targeted therapies, reduce the toxicities of chemotherapy regimens, and personalize treatment plans can further improve survival rates while minimizing long-term effects. Research aims to identify specific genetic markers and molecular pathways to guide individualized treatment decisions and optimize treatment efficacy. By staying at the forefront of medical research, we can offer childhood ALL survivors the best possible chances of a healthy and fulfilling life.
Integrating survivorship care into pediatric oncology
A vital area of focus for future directions is the integration of survivorship care into pediatric oncology practice. This involves seamlessly transitioning survivors from active treatment to long-term follow-up care, incorporating comprehensive monitoring, and addressing their physical and psychosocial needs throughout their survivorship journey. Collaborative care between oncologists, primary care physicians, and specialists will ensure the provision of holistic care to survivors and improve their long-term outcomes. By integrating survivorship care into pediatric oncology, we can create a robust system that supports survivors at each stage of their post-treatment life.
Survivorship and long-term effects of Acute Lymphoblastic Leukemia in children warrant significant attention and support. While advancements in survival rates are promising, survivors face unique challenges, both physically and emotionally. Childhood ALL and its treatments can have a lasting impact on the individual’s growth, development, cognition, and emotional well-being. Regular monitoring and early interventions can help mitigate the long-term effects and promote the overall quality of life for survivors. Furthermore, continued research and advancements in treatment and survivorship care are pivotal in improving outcomes and enhancing the survivorship experience for children with ALL. By ensuring comprehensive and holistic care, we can empower childhood ALL survivors to thrive and live fulfilling lives beyond their cancer journey.
Watch This Video Below
Related Terms About Survivorship and Long-term Effects of Acute Lymphoblastic Leukemia in Children
Acute Lymphoblastic Leukemia Child Care, Acute Lymphoblastic Leukemia Child Causes, Acute Lymphoblastic Leukemia Child Relapse, Acute Lymphoblastic Leukemia Child Stories, Acute Lymphoblastic Leukemia Child Survival Rate, Acute Lymphoblastic Leukemia Child Treatment, Acute Lymphoblastic Leukemia Child Uk, Acute Lymphoblastic Leukemia Childhood Cancers, Acute Lymphoblastic Leukemia Cincinnati Children’s, Acute Lymphoblastic Leukemia In 3 Year Old