Living with Dermatitis Herpetiformis, a chronic skin condition linked to gluten intolerance, can be challenging. However, there are coping strategies and support available to help you manage the symptoms and lead a fulfilling life. From adopting a gluten-free diet to seeking emotional support from support groups and healthcare professionals, this article explores various ways that can assist you in navigating the complexities of living with Dermatitis Herpetiformis.
Understanding Dermatitis Herpetiformis
What is dermatitis herpetiformis?
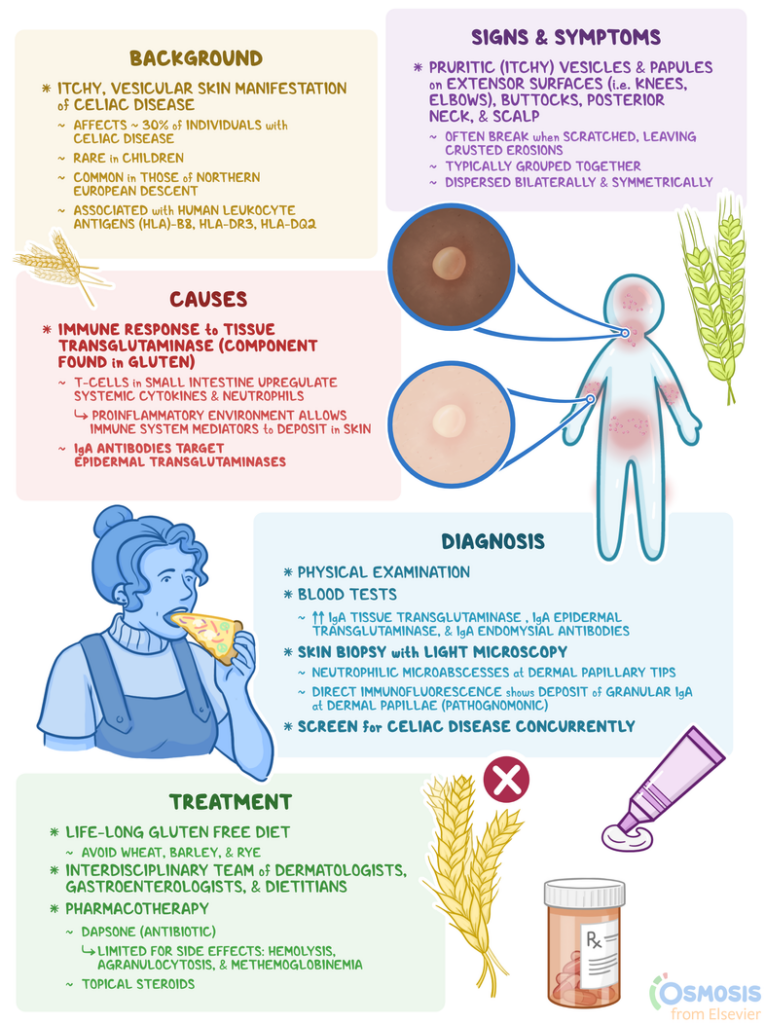
Dermatitis herpetiformis is a chronic skin condition characterized by intensely itchy and blistering skin rashes. It is an autoimmune disorder that occurs as a result of an immune reaction to gluten, a protein found in wheat, barley, and rye. The name “dermatitis herpetiformis” is somewhat misleading, as the condition is not related to herpes or caused by a virus. The term was coined because the skin lesions resemble those seen in herpes infections.
Causes of dermatitis herpetiformis
The exact cause of dermatitis herpetiformis is not fully understood, but it is believed to be strongly associated with gluten intolerance or celiac disease. When individuals with dermatitis herpetiformis consume gluten, their immune system recognizes it as a threat and mounts an attack on the skin, resulting in the characteristic rash. This immune response is mediated by certain antibodies called IgA antibodies, which bind to gluten in the small intestine and then migrate to the skin, causing inflammation and blister formation.
Symptoms of dermatitis herpetiformis
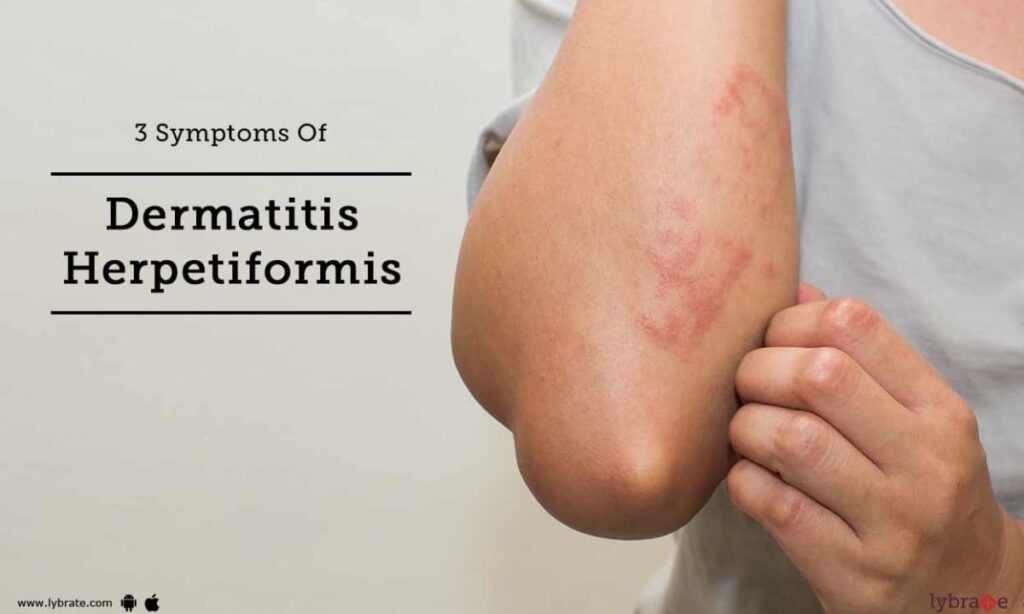
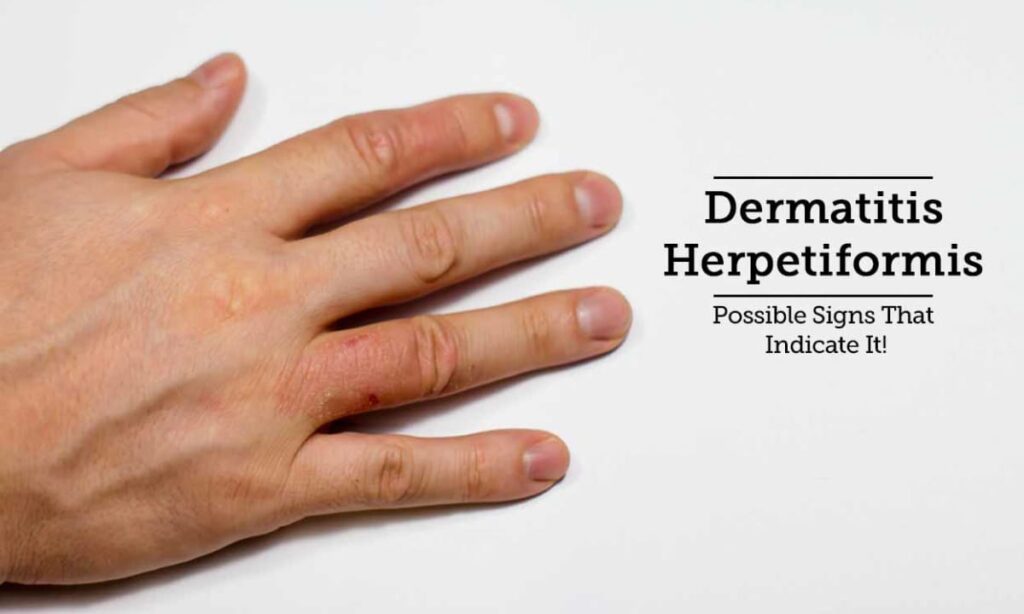
The main symptom of dermatitis herpetiformis is intensely itchy and blistering skin lesions. These lesions typically occur symmetrically and are commonly found on the elbows, knees, buttocks, and scalp. The blisters may be small and scattered or grouped together in a cluster. Scratching the affected areas can lead to excoriation and secondary infection. Other accompanying symptoms of dermatitis herpetiformis include a burning sensation, stinging, and redness of the skin.
Diagnosis of dermatitis herpetiformis
Diagnosing dermatitis herpetiformis usually involves a combination of clinical evaluation, skin biopsy, and blood tests. During the clinical evaluation, a dermatologist will examine the skin lesions, inquire about symptoms, and ask about any family history of celiac disease or gluten sensitivity. A skin biopsy is typically performed to examine the characteristics of the skin lesions under a microscope. Blood tests are also used to check for the presence of specific antibodies, such as IgA antibodies and antibodies against tissue transglutaminase (TTG).
Medical Treatment Options
Topical medications for dermatitis herpetiformis
Topical medications can be used to manage the symptoms of dermatitis herpetiformis and provide relief from itching and inflammation. These medications may include corticosteroid creams or ointments, which help reduce inflammation and alleviate itching. Additionally, topical antibiotics may be prescribed to prevent or treat secondary bacterial infection caused by scratching.
Oral medications for dermatitis herpetiformis
In addition to topical treatments, oral medications are often used to control the immune response and reduce the severity of symptoms in dermatitis herpetiformis. The most commonly prescribed medication for this condition is dapsone, which is an antibiotic that suppresses the immune system and reduces inflammation. However, dapsone has potential side effects and requires close monitoring by a healthcare professional.
Lifestyle changes to manage dermatitis herpetiformis
Making certain lifestyle changes can also help manage dermatitis herpetiformis. The most important change is adopting a strict gluten-free diet. Eliminating gluten from your diet can significantly improve the symptoms and prevent future outbreaks. It is important to read food labels carefully, as gluten can be found in many processed foods, condiments, and even non-food items like medications and cosmetics. Other lifestyle modifications that may be helpful include maintaining good skin hygiene, avoiding harsh soaps and detergents, and minimizing exposure to irritants and triggers.
Maintaining a Gluten-Free Diet
Understanding gluten and its effects on dermatitis herpetiformis
Gluten is a protein composite found in wheat, barley, and rye. In individuals with dermatitis herpetiformis, gluten triggers an immune response that leads to the characteristic skin lesions. It is important to understand that even small traces of gluten can cause a reaction, so strict adherence to a gluten-free diet is essential for managing the condition effectively.
Foods to avoid on a gluten-free diet
To maintain a gluten-free diet, it is important to avoid foods that contain wheat, barley, and rye. This includes products such as bread, pasta, cereals, cakes, and cookies. In addition, individuals with dermatitis herpetiformis should be cautious of cross-contamination, which can occur when gluten-free foods come into contact with surfaces or utensils that have been in contact with gluten-containing foods.
Gluten-free alternatives and substitutions
Fortunately, there are many gluten-free alternatives and substitutions available. These include grains like rice, corn, quinoa, and millet, as well as gluten-free flours, such as almond flour, coconut flour, and chickpea flour. Many gluten-free products are now readily available in supermarkets and health food stores, making it easier to maintain a gluten-free diet. It is also important to note that naturally gluten-free foods, such as fruits, vegetables, meat, poultry, and fish, can be enjoyed without worry.
Skin Care for Dermatitis Herpetiformis
Gentle skincare routines for dermatitis herpetiformis
When it comes to skincare for dermatitis herpetiformis, a gentle approach is crucial. Avoiding harsh products and excessive scrubbing is important to minimize irritation and prevent further damage to the skin. Cleanse the skin using mild, soap-free cleansers, and pat dry gently with a soft towel. After cleansing, apply a moisturizer that is hypoallergenic and fragrance-free to help hydrate the skin and reduce dryness.
Choosing suitable skincare products
When selecting skincare products for dermatitis herpetiformis, it is important to choose products that are suitable for sensitive skin. Look for labels that indicate the product is hypoallergenic, fragrance-free, and free from potential irritants. Avoid products that contain harsh detergents, alcohol, or strong fragrances, as these can further irritate the skin. It may also be helpful to do a patch test before using a new product on a larger area of the skin to ensure it does not cause any adverse reactions.
Protecting the skin from irritants
To minimize the risk of triggering or aggravating dermatitis herpetiformis, it is important to protect the skin from irritants and allergens. This can be achieved by wearing protective clothing, such as gloves, long sleeves, and hats, when necessary. Avoid prolonged contact with harsh chemicals or substances that may irritate the skin, and choose hypoallergenic and fragrance-free laundry detergents and fabric softeners. It may also be helpful to use a broad-spectrum sunscreen to protect the skin from the sun’s harmful UV rays.

Managing Itch and Discomfort
Over-the-counter itch relief options
Over-the-counter itch relief options can provide temporary relief from the intense itching associated with dermatitis herpetiformis. These may include topical creams or ointments containing ingredients like hydrocortisone or calamine, which can help soothe the skin and reduce itching. Antihistamine medications taken orally can also be effective in relieving itching and promoting better sleep.
Prescription medications for itch and discomfort
For more severe cases of dermatitis herpetiformis, prescription medications may be necessary to manage itch and discomfort. These may include prescription-strength corticosteroid creams or ointments, which can help reduce inflammation and itching. In some cases, stronger systemic medications, such as antihistamines or immune-suppressing drugs, may be prescribed by a healthcare professional to provide relief.
Home remedies and natural treatments
In addition to medical treatments, there are several home remedies and natural treatments that may help alleviate itch and discomfort associated with dermatitis herpetiformis. Taking cool showers or baths can help soothe the skin and relieve itching. Applying cool compresses or using gentle, natural ingredients like aloe vera gel or oatmeal baths can also provide relief. However, it is important to consult with a healthcare professional before trying any home remedies, as they may not be suitable for everyone and could potentially worsen symptoms.
Coping with Emotional Challenges
Understanding the emotional impact of dermatitis herpetiformis
Living with dermatitis herpetiformis can have a significant emotional impact on individuals. The intense itching, discomfort, and visible skin lesions can cause feelings of embarrassment, self-consciousness, and frustration. These emotional challenges can often lead to increased stress, anxiety, and a decreased overall quality of life. It is important to recognize and address these emotional aspects while managing the physical symptoms of the condition.
Finding support and understanding
Finding support and understanding from family, friends, and healthcare professionals is vital when coping with the emotional challenges of dermatitis herpetiformis. Friends and family members can provide a supportive network and offer a listening ear. It may also be beneficial to join support groups or online communities where individuals with dermatitis herpetiformis can connect with others facing similar challenges. Additionally, speaking candidly with healthcare providers about the emotional impact of the condition can lead to additional resources and support.
Mental health resources for coping
In severe cases, the emotional impact of dermatitis herpetiformis may require professional mental health support. Therapists, counselors, or psychologists who specialize in dermatology or chronic illness can provide guidance and support in managing stress, anxiety, and depression related to the condition. Seeking professional help may be beneficial in developing coping strategies, improving self-esteem, and enhancing overall mental well-being.
Building a Support System
Educating family and friends about dermatitis herpetiformis
One of the key elements in building a support system is educating family and friends about dermatitis herpetiformis. It is important for them to understand the nature of the condition, its triggers, and the impact it has on daily life. By providing this information, loved ones can better support individuals with dermatitis herpetiformis, both emotionally and practically.
Finding support groups and online communities
Support groups and online communities can offer a wealth of information, empathy, and understanding. These platforms allow individuals with dermatitis herpetiformis to connect with others who share similar experiences and challenges. Support groups and online communities provide a safe space to ask questions, share tips, and find solace in the company of others who understand the unique struggles of living with this condition.
Engaging with medical professionals and healthcare providers
Developing a strong relationship with medical professionals and healthcare providers is essential for managing dermatitis herpetiformis effectively. Regular check-ups, follow-up appointments, and open communication are crucial for staying informed about the condition and its treatment options. Building trust and rapport with healthcare professionals can ensure that individuals with dermatitis herpetiformis receive the best care and support possible.
Identifying Triggers and Prevention
Recognizing common triggers of dermatitis herpetiformis outbreaks
Identifying common triggers of dermatitis herpetiformis outbreaks can help individuals manage the condition and prevent future flare-ups. Some common triggers include the ingestion of gluten-containing foods, such as bread, pasta, and pastries. Other triggers may include stress, hormonal changes, certain medications, and infections. It is important to be mindful of these triggers and take appropriate steps to minimize their impact.
Preventing flare-ups and managing triggers
Preventing flare-ups of dermatitis herpetiformis involves strict adherence to a gluten-free diet. By eliminating gluten from the diet, individuals can significantly reduce the occurrence and severity of outbreaks. Additionally, managing stress levels through relaxation techniques, exercise, and seeking emotional support can be beneficial. Identifying and avoiding other triggers, such as certain medications or personal care products, can also help prevent flare-ups.
Keeping a symptom and trigger journal
Keeping a symptom and trigger journal can be an effective way to identify patterns and gain insight into individual triggers for dermatitis herpetiformis. By documenting symptoms, activities, stress levels, and diet, it becomes easier to identify potential triggers and make informed decisions about managing the condition. Sharing this information with healthcare professionals can also aid in developing personalized treatment plans and preventive strategies.
Navigating Social Settings and Lifestyle
Eating out and attending social gatherings
Navigating social settings and maintaining a gluten-free diet can be challenging, particularly when eating out or attending social gatherings. It is important to communicate dietary restrictions and food sensitivities to hosts and restaurant staff in advance. Researching gluten-free options at restaurants and carrying gluten-free snacks can help ensure that individuals with dermatitis herpetiformis have suitable food choices. By being proactive and prepared, it is possible to enjoy social events and meals without compromising health or comfort.
Traveling with dermatitis herpetiformis
Traveling with dermatitis herpetiformis requires careful planning to maintain a gluten-free diet away from home. Before traveling, research gluten-free options available at the destination, including restaurants, hotels, and local grocery stores. Pack gluten-free snacks and staple items to have on hand during the trip. It may also be helpful to carry a letter from a healthcare professional explaining the dietary restrictions for added convenience and understanding.
Adapting to everyday living with dermatitis herpetiformis
Adapting to everyday living with dermatitis herpetiformis involves making long-term adjustments to accommodate the condition. This may include dedicating time to meal planning and cooking at home, educating oneself about gluten-free alternatives, and establishing a routine for skincare and medication management. While it may initially feel overwhelming, with time and practice, managing the condition becomes more seamless and incorporated into daily life.
Handling Relapses and Recurrences
Understanding the possibility of relapses and recurrences
It is important to understand that relapses and recurrences are common in dermatitis herpetiformis, even with strict adherence to a gluten-free diet. Factors such as accidental gluten exposure, underlying autoimmune conditions, and hormonal changes can contribute to relapses. It is essential to be prepared for the possibility of relapses and to approach them with resilience and a proactive mindset.
Steps to take when experiencing a relapse
When experiencing a relapse, it is crucial to revisit the gluten-free diet and ensure strict adherence. Reviewing food choices, cross-contamination risks, and potential hidden gluten sources is important. Additionally, seeking prompt medical attention and adjusting medication dosages, if necessary, can help manage symptoms. It is also beneficial to revisit self-care strategies and emotional support mechanisms during relapses to maintain overall well-being.
When to seek medical help for recurrent episodes
While many individuals with dermatitis herpetiformis can effectively manage relapses on their own, there are instances where seeking medical help is necessary. If symptoms worsen, become unbearable, or are accompanied by signs of infection, it is important to consult a healthcare professional. Moreover, if the current treatment plan seems ineffective or if there are concerns about medication side effects, a healthcare professional can provide guidance and adjust the treatment approach accordingly.
Living with dermatitis herpetiformis can present unique challenges, but with the right support, self-care strategies, and treatment options, individuals can successfully manage the condition and maintain an overall good quality of life. By understanding the nature of dermatitis herpetiformis, adopting a gluten-free diet, implementing proper skincare routines, identifying triggers, and building a strong support system, individuals with this condition can navigate through the physical and emotional aspects, empowering themselves to lead fulfilling lives.
