Understanding Gastroesophageal Reflux Disease, commonly known as GERD, is crucial in maintaining a healthy digestive system. This condition occurs when stomach acid flows back into the esophagus, resulting in uncomfortable symptoms such as heartburn and regurgitation. By gaining a deeper understanding of GERD and its causes, you can effectively manage your symptoms and improve your quality of life.
Overview of Gastroesophageal Reflux Disease
Definition and Description
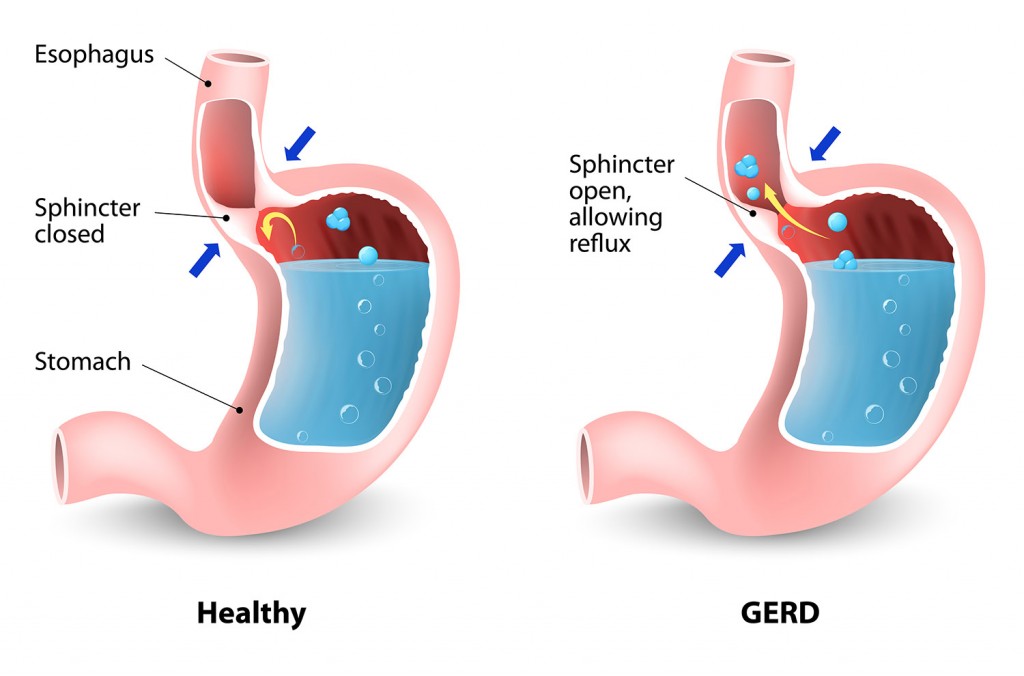
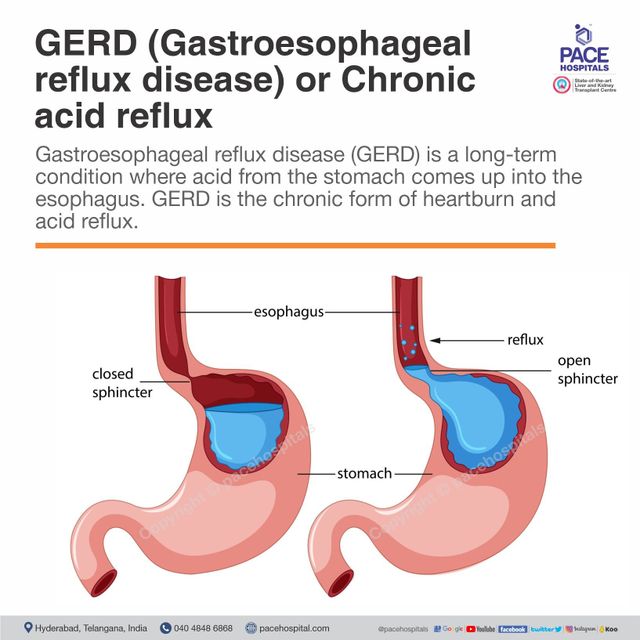
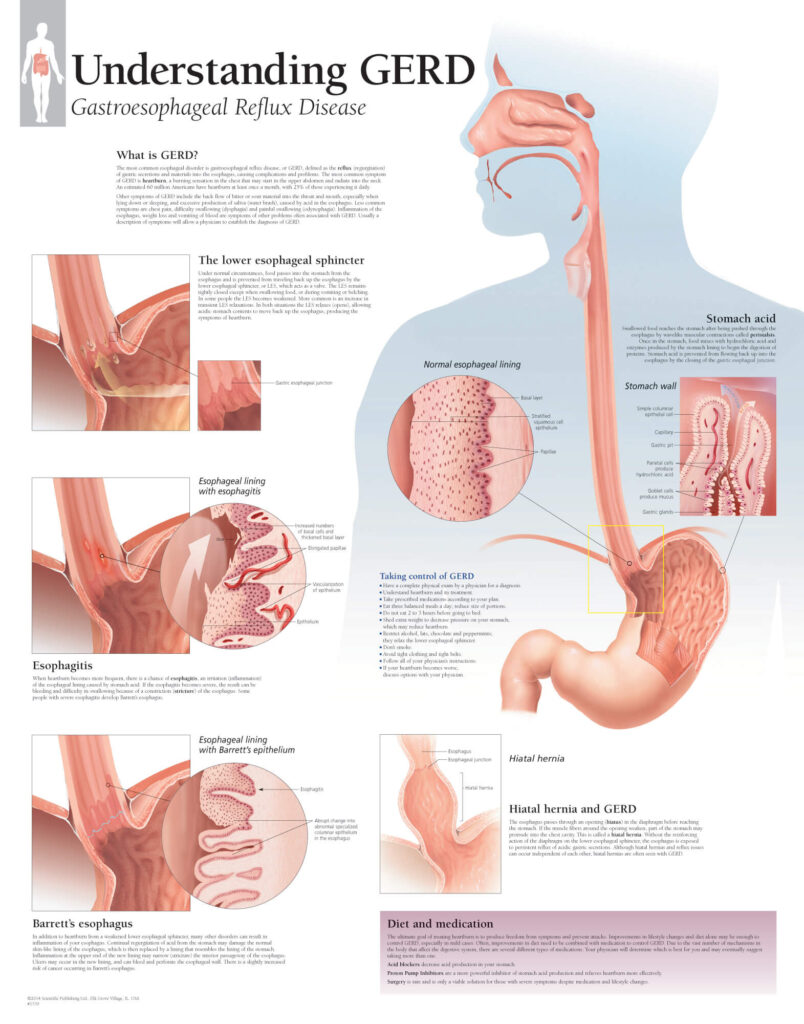
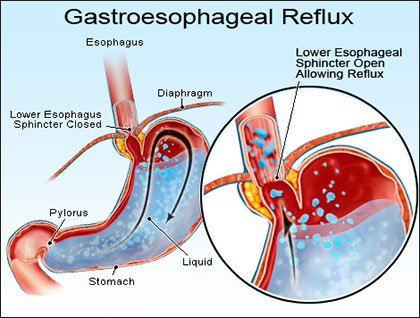
Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid and other stomach contents backflow into the esophagus, causing irritation and discomfort. This occurs when the lower esophageal sphincter, which usually acts as a valve to prevent the contents of the stomach from flowing upward, becomes weak or relaxes inappropriately. GERD can lead to various symptoms such as heartburn, chest pain, regurgitation, and difficulty swallowing.
Prevalence and Incidence
GERD is a common condition worldwide, affecting people of all ages. It is estimated that around 20% of the population in the United States experiences symptoms of GERD at least once a week. The incidence of GERD has been increasing in recent years, likely due to changes in lifestyle and dietary habits. While more prevalent in adults, GERD can also affect children and adolescents.
Causes of Gastroesophageal Reflux Disease
There are several factors that can contribute to the development of GERD. One of the main causes is a weakened or dysfunctional lower esophageal sphincter (LES), which allows the stomach acid to flow back into the esophagus. This can be due to factors such as obesity, certain medications, smoking, and certain disorders like hiatal hernia. Certain lifestyle habits and dietary choices, including consuming spicy or fatty foods, eating large meals, and lying down immediately after eating, can also trigger or exacerbate GERD symptoms.
Risk Factors for Gastroesophageal Reflux Disease
Obesity
Obesity is a significant risk factor for GERD. Excess weight can exert pressure on the abdomen, leading to increased pressure on the stomach and the LES. This pressure can cause the LES to weaken, making it easier for stomach acid to reflux into the esophagus. Losing weight through a combination of diet and exercise can significantly reduce the symptoms of GERD.
Pregnancy
During pregnancy, hormonal changes and the growing uterus can put pressure on the stomach and LES, causing frequent episodes of GERD. Additionally, the relaxation of smooth muscles due to pregnancy hormones can contribute to the reflux of stomach acid. Pregnant women with GERD symptoms should consult with their healthcare provider for appropriate treatment options.
Hiatal Hernia
A hiatal hernia is a condition where a portion of the stomach protrudes into the chest cavity through the diaphragm. This anatomical abnormality can weaken the LES and increase the risk of GERD. Hiatal hernias are commonly associated with reflux symptoms, although not everyone with a hiatal hernia experiences GERD. Treatment options for GERD in individuals with hiatal hernia may include medication and surgical interventions.
Smoking
Smoking has been linked to a higher risk of developing GERD. The chemicals in tobacco smoke can weaken the LES and impair the normal function of the esophagus, increasing the likelihood of acid reflux. Quitting smoking can not only reduce the risk of GERD but also improve overall health and reduce the risk of other smoking-related diseases.
Symptoms and Complications of Gastroesophageal Reflux Disease
Common Symptoms
The most common symptom of GERD is heartburn, which is characterized by a burning sensation in the chest that may radiate to the throat. Other common symptoms include regurgitation, where stomach contents or acid flow back into the mouth, and difficulty swallowing. Some individuals may also experience persistent cough, hoarseness, or a sore throat.
Atypical Symptoms
In addition to the typical symptoms, GERD can sometimes manifest with atypical symptoms, which can make the diagnosis challenging. These include asthma-like symptoms, such as wheezing and shortness of breath, as well as dental erosions, chronic sore throat, and even ear pain. It is important to discuss these atypical symptoms with a healthcare provider for proper evaluation and diagnosis.
Complications
If left untreated, GERD can lead to various complications. Chronic exposure to stomach acid can cause inflammation and damage to the esophagus, leading to a condition called esophagitis. Over time, this continuous irritation can result in the formation of strictures, which are narrowed areas in the esophagus that can make swallowing difficult. In rare cases, GERD can contribute to the development of Barrett’s esophagus, a condition that increases the risk of esophageal cancer.
Diagnosis of Gastroesophageal Reflux Disease
Medical History and Physical Examination
To diagnose GERD, a healthcare provider will typically start by taking a detailed medical history and performing a physical examination. They will inquire about symptoms, their frequency and severity, as well as any triggering factors. The physical examination may involve checking for signs of acid reflux, such as inflammation in the throat or teeth erosion.
Diagnostic Tests
If the medical history and physical examination suggest GERD, additional diagnostic tests may be recommended. These can include an upper endoscopy, which allows the healthcare provider to visualize the esophagus, stomach, and duodenum using a flexible tube with a camera. Other tests may include esophageal pH monitoring, where a small catheter is placed in the esophagus to measure acid levels, and esophageal manometry, which assesses the function and coordination of the esophageal muscles.
Treatment Options for Gastroesophageal Reflux Disease
Lifestyle Modifications
Lifestyle modifications play a crucial role in managing GERD symptoms. These include avoiding trigger foods such as spicy and fatty foods, chocolate, caffeine, and alcohol. Eating smaller, more frequent meals and avoiding lying down immediately after eating can also help reduce reflux. Elevating the head of the bed by using pillows or a wedge can assist in preventing acid reflux during sleep. Weight loss for those who are overweight or obese is highly recommended.
Medications
There are several medications available to treat GERD. Proton pump inhibitors (PPIs) reduce stomach acid production, providing relief from symptoms and allowing the esophagus to heal. H2 blockers are another class of medications that can reduce acid production. Antacids can provide temporary relief by neutralizing stomach acid. It is important to use these medications under the guidance of a healthcare provider to ensure appropriate dosing and long-term safety.
Surgical Interventions
In severe cases of GERD that do not respond to lifestyle modifications and medications, surgical interventions may be considered. The most common procedure is called fundoplication, where the upper part of the stomach is wrapped around the lower esophagus to strengthen the LES. This surgery aims to prevent the reflux of stomach acid. Other less invasive procedures, such as endoscopic treatments, may also be options for select individuals.
Prevention of Gastroesophageal Reflux Disease
Dietary Adjustments
Making certain dietary adjustments can help prevent or reduce GERD symptoms. This includes avoiding trigger foods, as mentioned earlier, and opting for a diet rich in fruits, vegetables, whole grains, and lean proteins. Eating smaller meals and avoiding heavy meals before bedtime can also be beneficial.
Maintaining a Healthy Weight
Maintaining a healthy weight is crucial in preventing GERD. Excess weight can put pressure on the abdomen, leading to increased pressure on the stomach and LES, and increasing the risk of acid reflux. Adopting a well-balanced diet and incorporating regular physical activity can contribute to weight management and minimize the chances of developing GERD.
Avoiding Trigger Foods
Identifying and avoiding trigger foods can significantly reduce the occurrence of GERD symptoms. Common trigger foods include spicy foods, citrus fruits, tomatoes, chocolate, caffeinated beverages, and alcohol. It may be helpful to keep a food diary to identify which foods worsen symptoms and then make necessary dietary adjustments.
Managing Symptoms and Reducing Reflux
Elevating the Head of the Bed
Elevating the head of the bed by using pillows or a wedge can help prevent stomach acid from flowing back into the esophagus during sleep. This simple measure can help alleviate nighttime symptoms of GERD and reduce the frequency of acid reflux episodes.
Avoiding Large Meals Before Bedtime
Consuming large meals shortly before bedtime can increase the likelihood of acid reflux. It is recommended to eat smaller, more frequent meals throughout the day and to avoid heavy meals within a few hours of going to bed. This allows the stomach to digest food more efficiently and reduces the chances of experiencing nighttime acid reflux.
Avoiding Certain Exercises and Positions
Certain exercises and activities that involve bending forward or putting pressure on the abdomen can trigger acid reflux episodes. Avoiding exercises such as sit-ups or wearing tight-fitting clothing can help reduce the risk of reflux. Similarly, maintaining an upright position after meals rather than lying down immediately can prevent stomach acid from flowing back into the esophagus.
Not Lying Down Immediately After Eating
Lying down immediately after eating can promote the backward flow of stomach acid into the esophagus. It is advisable to stay in an upright position for at least two to three hours after meals to allow sufficient time for digestion. This practice can help minimize the occurrence of acid reflux and its associated symptoms.
Potential Complications and Long-Term Outlook
Esophageal Strictures
If left untreated, chronic exposure to stomach acid can lead to the development of esophageal strictures. These are narrowed areas in the esophagus that can make swallowing difficult and uncomfortable. Treatment for esophageal strictures typically involves dilation, a procedure where a special instrument is used to stretch and widen the narrowed part of the esophagus.
Barrett’s Esophagus
Barrett’s esophagus is a condition in which the lining of the esophagus undergoes changes due to chronic exposure to stomach acid. This condition increases the risk of developing esophageal cancer. Regular endoscopic surveillance is typically recommended for individuals with Barrett’s esophagus to monitor for any signs of dysplasia or cancer.
Esophageal Cancer
In rare cases, long-standing and untreated GERD can lead to the development of esophageal cancer. Regular screenings and early detection are crucial in improving the prognosis of esophageal cancer. Prompt medical attention for GERD symptoms and adherence to recommended treatment plans can help mitigate the risk of developing esophageal cancer.
Lifestyle Modifications and Self-Care Strategies
Dietary Changes
In addition to dietary changes mentioned earlier, certain food and lifestyle habits can contribute to the management of GERD symptoms. Chewing food slowly and thoroughly can aid digestion and reduce the likelihood of acid reflux. It is also recommended to avoid eating within three hours of bedtime and to elevate the head of the bed during sleep.
Weight Loss Strategies
For individuals who are overweight or obese, weight loss can significantly improve GERD symptoms. Adopting a well-balanced diet, portion control, and regular exercise can contribute to gradual and sustainable weight loss. Consulting with a healthcare provider or registered dietitian can provide guidance on a personalized weight loss strategy.
Stress Reduction Techniques
Stress and anxiety can exacerbate GERD symptoms in some individuals. Engaging in stress reduction techniques such as meditation, deep breathing exercises, and regular physical activity can help manage stress levels and potentially reduce the frequency and severity of reflux episodes. It is important to find strategies that work best for each individual’s unique needs.
The Role of Acid Reducing Medications in Gastroesophageal Reflux Disease
Proton Pump Inhibitors
Proton pump inhibitors (PPIs) are commonly prescribed medications for the treatment of GERD. They work by reducing the production of stomach acid, providing relief from symptoms and allowing the esophagus to heal. PPIs are usually taken once a day before breakfast and should be used under the guidance of a healthcare provider due to potential side effects and long-term safety considerations.
H2 Blockers
H2 blockers are another class of medications used to reduce stomach acid production. They work by blocking histamine receptors on the stomach cells, thus reducing acid secretion. H2 blockers are typically taken before meals or at bedtime and can provide relief from GERD symptoms. As with any medication, it is important to use H2 blockers as directed and consult with a healthcare provider if symptoms persist.
Antacids
Antacids are over-the-counter medications that provide quick relief from heartburn and mild symptoms of GERD. They work by neutralizing stomach acid, reducing its corrosive effects on the esophagus. Antacids are available in various forms, including chewable tablets, liquids, and effervescent powders. While effective for immediate symptom relief, antacids are not a long-term solution for managing GERD and may have limitations in controlling acid reflux throughout the day.
In conclusion, gastroesophageal reflux disease is a common condition that can cause significant discomfort and potentially lead to complications if left untreated. By understanding the causes, risk factors, symptoms, and treatment options for GERD, individuals can take proactive steps to manage their condition effectively. Lifestyle modifications, medications, and, in severe cases, surgical interventions can all play a role in improving symptoms and enhancing the quality of life for those affected by GERD. It is essential to work closely with healthcare providers to develop personalized management strategies and to seek medical attention promptly for prompt diagnosis and appropriate treatment. With proper care and adherence to recommended strategies, individuals with GERD can successfully manage their symptoms and prevent long-term complications.