If you’ve ever wondered about the risks and challenges that elderly patients face when it comes to acute renal failure, then look no further. In this article, we will explore the specific concerns that arise when older adults are diagnosed with this condition. From the potential causes to the unique treatment approaches, get ready to gain a better understanding of the complex factors that contribute to acute renal failure in elderly patients. So, grab a cup of tea and prepare to dive into this insightful exploration!

Understanding Acute Renal Failure in Elderly Patients
Acute Renal Failure, also known as acute kidney injury (AKI), refers to a sudden and rapid decline in kidney function. This condition is particularly concerning in elderly patients due to the increased vulnerability of their kidneys and the potential impact on their overall health and well-being. Understanding the causes, risk factors, clinical presentation, management approaches, complications, preventive measures, challenges, prognosis, and patient support for acute renal failure is crucial in providing effective care for elderly individuals.
Definition of Acute Renal Failure
Acute Renal Failure is defined as a sudden loss of kidney function, leading to an accumulation of metabolic waste products and disturbances in fluid and electrolyte balance. This condition is characterized by a rapid decline in glomerular filtration rate (GFR), which is a measure of the kidneys’ ability to filter waste and excess fluid from the blood. Acute Renal Failure can be classified into three categories: prerenal, intrinsic renal, and postrenal. Prerenal AKI refers to a decrease in blood flow to the kidneys, intrinsic renal AKI involves damage to the kidney tissue itself, and postrenal AKI results from obstruction of the urinary tract.
Impact of Acute Renal Failure on Elderly Patients
Acute Renal Failure poses unique challenges and risks to elderly patients. Due to the aging process, the kidneys undergo structural and functional changes, making them more susceptible to injury and dysfunction. Additionally, elderly individuals often have comorbidities and chronic diseases, which can further compromise kidney function. The consequences of acute renal failure in the elderly population include increased morbidity and mortality rates, prolonged hospital stays, heightened risk of complications, and compromised quality of life. To ensure optimal outcomes, it is essential to address the specific needs and risks associated with acute renal failure in elderly patients.
Risk Factors for Acute Renal Failure
Several factors contribute to the development of acute renal failure in the elderly population. These include age-related factors, comorbidities and chronic diseases, medications and prescriptions, and dehydration and fluid imbalance.
Age-related Factors
The aging process itself is a significant risk factor for acute renal failure. As individuals age, their kidneys undergo structural and functional changes, including a reduction in kidney size, decreased blood flow, and diminished glomerular filtration rate. These age-related changes make elderly patients more susceptible to acute kidney injury and hinder their ability to recover from such an insult.
Comorbidities and Chronic Diseases
Elderly individuals often have underlying comorbidities and chronic diseases, such as hypertension, diabetes, heart disease, and chronic kidney disease (CKD). These conditions can impair kidney function and increase the risk of developing acute renal failure. The presence of multiple comorbidities also complicates the treatment and management of acute renal failure in elderly patients.
Medications and Prescriptions
The use of certain medications and prescriptions can contribute to acute renal failure in elderly patients. Some medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, and contrast agents, are known to have nephrotoxic effects and can cause kidney damage. Polypharmacy and inappropriate prescribing practices can further increase the risk of medication-induced acute renal failure in elderly individuals.
Dehydration and Fluid Imbalance
Dehydration and fluid imbalance are common risk factors for acute renal failure, particularly in elderly patients. These individuals may have reduced thirst sensations, impaired renal concentrating ability, and limited access to fluids, all of which can contribute to dehydration. Additionally, conditions such as vomiting, diarrhea, excessive sweating, and impaired fluid intake can further disrupt fluid balance and increase the risk of acute kidney injury in the elderly population.
Clinical Presentation and Diagnosis
Recognizing the symptoms and signs of acute renal failure is crucial for early intervention and management. However, diagnosing acute renal failure in elderly patients can be challenging due to age-related changes in physiology and atypical presentations.
Symptoms and Signs of Acute Renal Failure
The clinical presentation of acute renal failure in elderly patients may vary, and some symptoms may be subtle or non-specific. Common symptoms include decreased urine output (oliguria or anuria), fatigue, generalized swelling (edema), shortness of breath, confusion, nausea, and difficulty concentrating. Physical examination findings may include fluid overload, elevated blood pressure, abnormal heart sounds, and signs of dehydration.
Diagnostic Tests and Biomarkers
Diagnosing acute renal failure in elderly patients involves a combination of clinical assessment and laboratory tests. Common diagnostic tests include blood tests to measure kidney function, such as serum creatinine and blood urea nitrogen (BUN) levels. Imaging studies, such as ultrasound, may also be used to assess kidney structure and identify potential obstructions. Additionally, urinary tests, including urinalysis and urine electrolyte measurements, can provide valuable information about kidney function and the possible underlying cause of acute renal failure.
Challenges in Diagnosis in Elderly Patients
Diagnosing acute renal failure in elderly patients can be challenging due to several factors. Firstly, the symptoms may be masked or attributed to other conditions commonly seen in the elderly population, such as heart failure or chronic obstructive pulmonary disease (COPD). Secondly, age-related changes in kidney function make it difficult to establish a baseline and identify the extent of decline. Finally, comorbidities and chronic diseases can further complicate the diagnostic process, requiring a comprehensive evaluation and consideration of multiple factors to make an accurate diagnosis.
Management Approaches for Acute Renal Failure
The management of acute renal failure in elderly patients requires a multidisciplinary approach to address the specific needs and challenges associated with this condition. Medical interventions, nutritional considerations, pharmacological interventions, and fluid and electrolyte management play crucial roles in optimizing outcomes for elderly patients with acute renal failure.
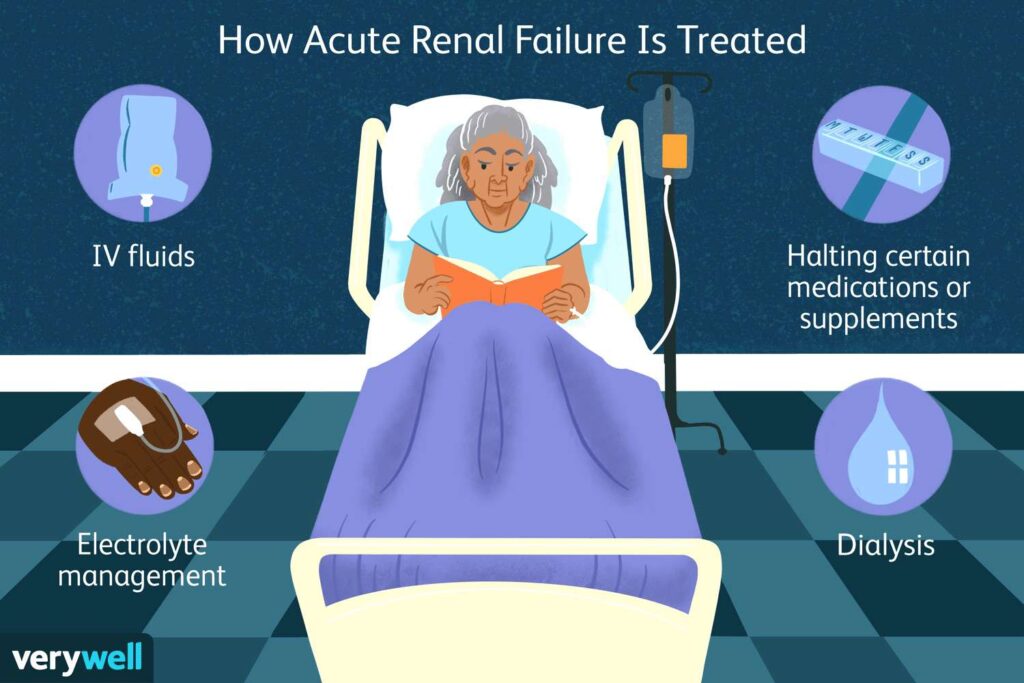
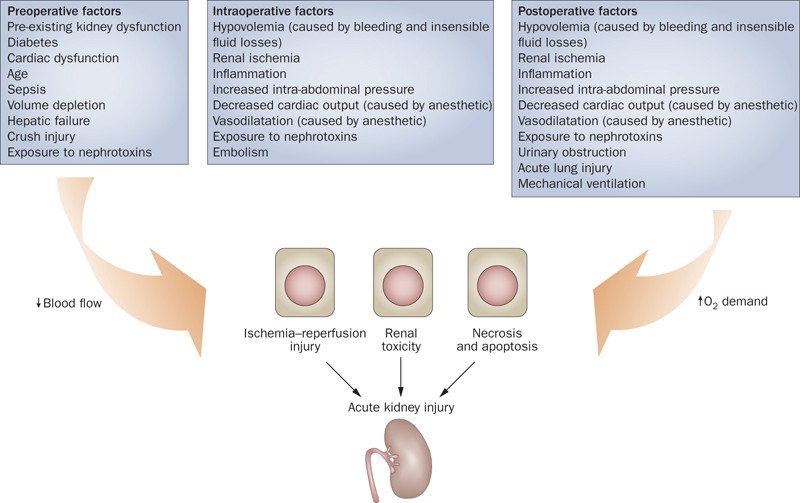
Medical Interventions and Treatments
The primary goal of medical interventions in acute renal failure is to identify and treat the underlying cause while promoting kidney recovery. Prerenal causes may require fluid resuscitation or addressing hemodynamic instability. In intrinsic renal and postrenal causes, interventions may include removing obstructions, treating infections, or discontinuing nephrotoxic medications. In severe cases, renal replacement therapy, such as hemodialysis or continuous renal replacement therapy, may be necessary to support kidney function and remove waste products.
Nutritional Considerations
Elderly patients with acute renal failure require careful attention to their nutritional needs to prevent further complications and optimize recovery. Dietary modifications, such as restriction of sodium, phosphorus, and potassium, may be necessary to maintain fluid and electrolyte balance. Adequate protein intake is essential for preventing malnutrition, while fluid restriction may be required in certain cases of fluid overload. In some instances, enteral or parenteral nutrition may be necessary to meet the nutritional needs of elderly patients with acute renal failure.
Pharmacological Interventions
Pharmacological interventions play a crucial role in managing acute renal failure in elderly patients. Medications may be prescribed to address underlying comorbidities, manage symptoms, and prevent further kidney injury. Examples include antihypertensive medications to control blood pressure, diuretics to promote urine output, and medications to manage electrolyte imbalances. It is important to consider the pharmacokinetics and pharmacodynamics of medications in elderly patients, as age-related changes can affect drug metabolism and clearance.
Fluid and Electrolyte Management
Maintaining fluid and electrolyte balance is essential in the management of acute renal failure in elderly patients. Fluid status should be carefully monitored and adjustments made accordingly to prevent fluid overload or dehydration. Electrolyte imbalances, such as hyperkalemia or hyponatremia, should be promptly addressed to prevent cardiac arrhythmias and other complications. Close collaboration between healthcare providers and the individual’s healthcare team is necessary to monitor and adjust fluid and electrolyte management in elderly patients.

Complications of Acute Renal Failure in Elderly Patients
Acute renal failure in elderly patients can lead to various complications that impact their overall health and well-being. Recognizing and addressing these complications is crucial in optimizing outcomes and ensuring the best possible quality of life for elderly individuals.
Cardiovascular Complications
Acute renal failure significantly increases the risk of cardiovascular complications in elderly patients. These individuals are already prone to cardiovascular diseases, and acute kidney injury further exacerbates this vulnerability. Complications may include congestive heart failure, arrhythmias, myocardial infarction, and even sudden cardiac death. Close monitoring and appropriate management of fluid status, blood pressure, and electrolyte balance are essential in preventing and managing cardiovascular complications.
Infections and Sepsis
Elderly patients with acute renal failure are more prone to infections and sepsis due to compromised immune function and impaired renal clearance of pathogens. Urinary tract infections, pneumonia, bloodstream infections, and surgical site infections are common in this population. Early recognition and treatment of infections, together with careful attention to aseptic techniques during medical interventions, are necessary to prevent the development and progression of sepsis in elderly patients with acute renal failure.
Impaired Wound Healing
Elderly patients with acute renal failure may experience impaired wound healing, which can lead to delayed recovery and increased morbidity. Kidney dysfunction affects the body’s ability to repair and regenerate tissues, making wounds more susceptible to infection and other complications. Close monitoring of wounds, appropriate wound care, and prompt treatment of underlying infections are essential in promoting optimal wound healing in elderly patients.
Risk of Chronic Kidney Disease
Acute renal failure in elderly patients increases the risk of developing chronic kidney disease (CKD) in the long term. The initial insult to the kidneys, coupled with underlying age-related changes and comorbidities, predisposes these individuals to ongoing kidney dysfunction. This highlights the importance of regular follow-up and monitoring of kidney function to detect early signs of CKD and initiate appropriate interventions to slow disease progression.
Preventive Measures for Acute Renal Failure
Prevention plays a vital role in reducing the burden of acute renal failure in elderly patients. By addressing modifiable risk factors and implementing preventive measures, healthcare providers can significantly reduce the incidence and impact of this condition in the elderly population.
Regular Monitoring and Screenings
Regular monitoring of kidney function and early detection of risk factors is essential in preventing acute renal failure in elderly patients. Healthcare providers should incorporate routine kidney function tests, such as serum creatinine and estimated glomerular filtration rate (eGFR) measurements, into the standard care for elderly individuals. Additionally, identifying and addressing modifiable risk factors, such as uncontrolled hypertension and diabetes, can help prevent the development of acute renal failure.
Optimizing Medication Regimen
Polypharmacy and inappropriate prescribing practices contribute to the development of acute renal failure in elderly patients. Healthcare providers should carefully review and optimize medication regimens to minimize the risk of nephrotoxicity and drug-induced kidney injury. This includes adjusting dosages based on renal function, considering alternative medications when necessary, and promoting regular medication reviews to prevent medication-related adverse events.
Hydration and Fluid Management
Maintaining adequate hydration and fluid balance is crucial in preventing acute renal failure in the elderly population. Elderly patients should be educated about the importance of regular fluid intake, and strategies should be implemented to ensure access to fluids throughout the day. In cases of underlying conditions or medications that increase the risk of dehydration, additional measures may be necessary to prevent fluid imbalance and subsequent kidney injury.
Renal Function Preservation Strategies
Implementing strategies to preserve renal function is essential in preventing acute renal failure in elderly patients. This may include lifestyle modifications such as a healthy diet, regular exercise, and smoking cessation, which help reduce the risk of underlying comorbidities. Healthcare providers should also promote the appropriate use of medications and encourage regular follow-up to detect and manage kidney dysfunction at an early stage. By focusing on renal function preservation, healthcare providers can reduce the incidence and impact of acute renal failure in elderly patients.

Challenges in Acute Renal Failure Management
Managing acute renal failure in elderly patients poses several challenges that require a comprehensive and multidisciplinary approach. These challenges include the complexity of elderly patients’ care, addressing polypharmacy issues, a multidisciplinary approach, and dilemmas in dialysis decision-making.
Multidisciplinary Approach
Effectively managing acute renal failure in elderly patients requires a multidisciplinary approach. This involves close collaboration between healthcare providers, including nephrologists, geriatricians, nurses, dietitians, pharmacists, and social workers. Each member of the healthcare team brings unique expertise and perspectives to optimize care and address the specific needs of elderly patients with acute renal failure. Regular interdisciplinary team meetings and communication facilitate a comprehensive and coordinated approach to treatment and management.
Complexity of Elderly Patients’ Care
Elderly patients with acute renal failure often have multiple comorbidities, polypharmacy, and functional impairments, making their care complex. Healthcare providers must consider the interactions between various conditions and medications in order to provide safe and effective interventions. Adjustments to treatment plans may be necessary to accommodate the specific needs and limitations of elderly patients while addressing the underlying cause of acute renal failure.
Addressing Polypharmacy Issues
Polypharmacy, or the use of multiple medications, is common in elderly patients with acute renal failure. This increases the risk of medication-related adverse events and interactions. Healthcare providers must carefully review medication regimens, assess the appropriateness of each medication, and consider potential drug-drug and drug-renal function interactions. Educating patients about their medications, promoting medication adherence, and encouraging regular medication reviews can help address polypharmacy issues and minimize the risk of medication-induced acute renal failure.
Dilemmas in Dialysis Decision-making
For some elderly patients with acute renal failure, the decision to initiate renal replacement therapy, such as dialysis, can be challenging. The benefits and risks of dialysis must be carefully considered, taking into account the patient’s overall health status, comorbidities, functional status, life expectancy, and personal preferences. Shared decision-making between the patient, their family, and healthcare providers is crucial in ensuring that the treatment plan aligns with the patient’s goals and values.
Prognosis and Outcomes
The prognosis for elderly patients with acute renal failure depends on various factors, including the underlying cause, comorbidities, and timely intervention. Understanding the potential outcomes and considering the impact on quality of life is essential in providing appropriate care and support.
Mortality Rates and Survival
Acute renal failure in elderly patients is associated with increased mortality rates compared to younger individuals. Elderly patients often have multiple comorbidities and reduced physiological reserve, which can contribute to poorer outcomes. However, with timely and appropriate intervention, including renal replacement therapy when indicated, survival rates can be improved. Close monitoring and individualized care are essential to optimize survival rates for elderly patients with acute renal failure.
Quality of Life Considerations
Quality of life is an important consideration in the management of acute renal failure in elderly patients. The impact of the condition, treatment modalities, and associated complications can significantly affect an individual’s physical, psychological, and social well-being. Healthcare providers should prioritize patient-centered care, taking into account the patient’s preferences, goals, and values. By addressing the specific needs and concerns of elderly patients, healthcare providers can help improve their quality of life despite the challenges posed by acute renal failure.
Functional Decline and Rehabilitation
Acute renal failure in elderly patients can lead to functional decline and loss of independence. Muscle wasting, decreased mobility, and overall weakness are common consequences of prolonged hospital stays and chronic illness. Rehabilitation plays a crucial role in minimizing functional decline and promoting independence in elderly patients with acute renal failure. Physical therapy, occupational therapy, and tailored exercise programs should be integrated into the treatment plan to optimize outcomes and enhance the individual’s functional capacity.
Long-term Renal Function
Long-term renal function is a significant consideration for elderly patients with acute renal failure. The initial insult to the kidneys and age-related changes can contribute to the development or progression of chronic kidney disease. Regular monitoring of kidney function, managing underlying comorbidities, and implementing renal function preservation strategies are essential to mitigate the risk of CKD and preserve long-term renal function in elderly individuals.
Patient Education and Support
Educating patients and their caregivers about acute renal failure is crucial in enabling them to actively participate in their care and make informed decisions. Additionally, providing support and addressing their psychological and emotional needs is essential to promote overall well-being.
Educating Patients and Caregivers
Patients and caregivers should receive comprehensive education about acute renal failure, its causes, risk factors, symptoms, treatment options, and self-care strategies. Healthcare providers should explain the importance of adhering to medication regimens, dietary restrictions, and fluid management protocols. Educating patients and caregivers about warning signs, such as changes in urine output or worsening symptoms, also empowers them to seek timely medical attention.
Supportive Care Measures
Supportive care measures are essential in addressing the psychosocial and emotional needs of elderly patients with acute renal failure. This may involve providing information about support groups and community resources, assisting with transportation to medical appointments, and offering emotional support and counseling. Encouraging open communication and involving family members in the care process can alleviate anxiety and enhance the overall support network for elderly patients.
Providing Psychological Support
Acute renal failure can have a significant psychological impact on elderly patients. Feelings of fear, anxiety, depression, and frustration are common. Healthcare providers should offer psychological support through counseling, referrals to mental health professionals, and involvement of support services. By addressing the psychological well-being of elderly patients, healthcare providers can enhance their overall quality of life and facilitate better coping strategies.
Navigating End-of-Life Care
In some cases, elderly patients with acute renal failure may face end-of-life decisions. Healthcare providers should engage in open and honest conversations about prognosis, goals of care, and the potential benefits and burdens of ongoing treatment. Advanced care planning and exploration of palliative care options are essential to ensure that the individual’s preferences and wishes are respected. Providing compassionate and comprehensive end-of-life care is crucial in supporting elderly patients with acute renal failure and their families.
Future Research and Innovations
Continued research and innovation hold promise in advancing our understanding and management of acute renal failure in elderly patients.
Exploring Novel Treatment Approaches
Ongoing research aims to identify novel treatment approaches for acute renal failure in elderly patients. This includes investigating new medications, therapeutic agents, and interventions that can preserve renal function, improve outcomes, and reduce the burden of complications. Clinical trials and studies are essential in expanding treatment options and tailoring interventions to the specific needs of elderly individuals.
Identifying Biomarkers and Predictive Tools
Biomarkers and predictive tools play a crucial role in diagnosing, assessing severity, and prognosticating acute renal failure. Ongoing research focuses on identifying specific biomarkers that can aid in the early detection, prediction of outcomes, and assessment of treatment response in elderly patients. These biomarkers may provide valuable insights into the mechanisms and progression of acute renal failure and guide individualized treatment plans.
Advancements in Renal Replacement Therapies
Renal replacement therapies, such as hemodialysis and continuous renal replacement therapy, continue to evolve and improve. Advancements in technology, such as the development of more efficient dialysis machines and novel dialysis membranes, enhance the efficacy and tolerability of these therapies in elderly patients. Ongoing research aims to optimize renal replacement therapies for elderly individuals, improving outcomes and quality of life.
Understanding Age-related Renal Changes
Further research into age-related changes in renal function is essential in refining the management of acute renal failure in elderly patients. This includes understanding the molecular and cellular mechanisms underlying age-related renal changes, identifying modifiable risk factors, and developing targeted interventions. By deepening our understanding of age-related renal changes, healthcare providers can tailor treatment plans and implement strategies to prevent and manage acute renal failure in elderly individuals.
Acute renal failure in elderly patients presents unique challenges and risks. Understanding the definition, impact, risk factors, clinical presentation, management approaches, complications, preventive measures, challenges, prognosis, and patient support for acute renal failure is vital in providing comprehensive and effective care. By considering the specific needs and vulnerabilities of elderly individuals, healthcare providers can optimize outcomes, enhance quality of life, and ensure the best possible care for this population.
Watch This Video Below
Related Terms About Acute Renal Failure in Elderly Patients
Acute Kidney Failure In Old Age, Acute Kidney Failure In Older Cats, Acute Kidney Failure Symptoms In Elderly, Acute Renal Failure Age Group, Acute Renal Failure In Elderly Prognosis, Acute Renal Failure In Senior Cats, Acute Renal Failure Symptoms In Elderly, What Are The Complications Of Acute Renal Failure