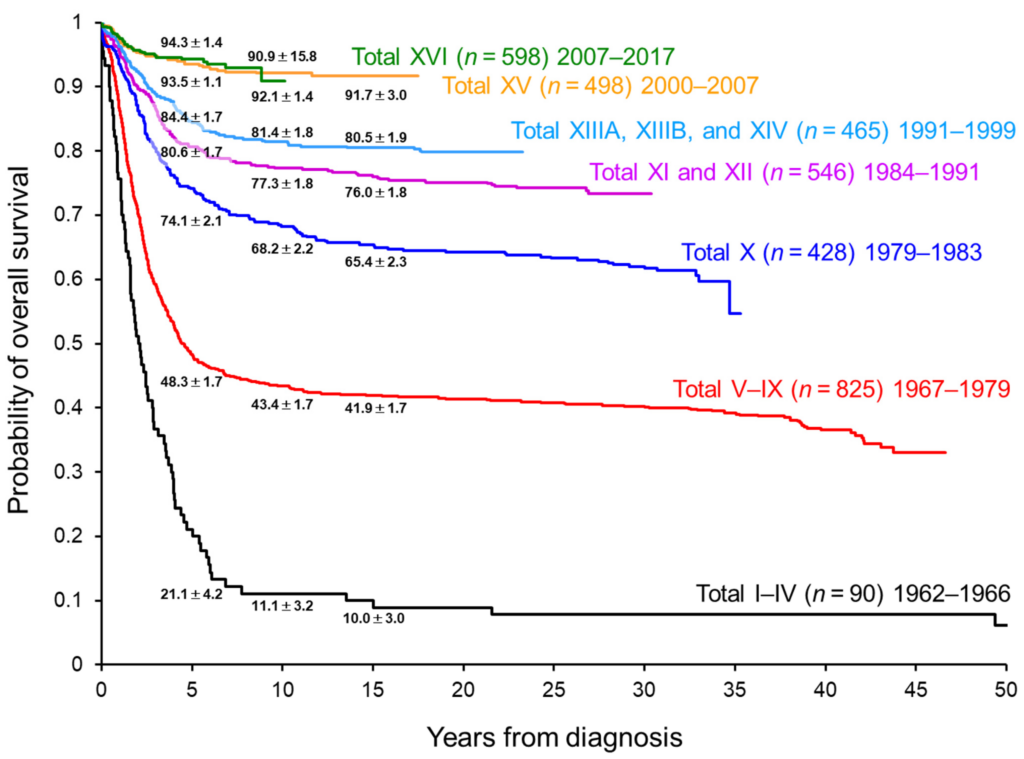
In this article, we will explore the incredible advancements being made in the field of research for children diagnosed with Acute Lymphoblastic Leukemia (ALL). As medical science continues to progress, new and innovative treatments are being developed that are improving outcomes and providing hope for these young patients and their families. From targeted therapies to immunotherapies, the focus on finding effective and compassionate treatments for ALL is giving children a fighting chance against this devastating disease. Let’s delve into the exciting developments and breakthroughs that are changing the lives of children battling Acute Lymphoblastic Leukemia.
Understanding Acute Lymphoblastic Leukemia (ALL)
Definition and Background
Acute Lymphoblastic Leukemia (ALL) is a type of cancer that affects the white blood cells, specifically the lymphocytes. It is the most common type of cancer in children, but it can also occur in adults. ALL occurs when the bone marrow produces too many immature lymphocytes, crowding out healthy blood cells. The underlying cause of ALL is still unknown, but it is believed to be a combination of genetic and environmental factors.
Epidemiology and Risk Factors
ALL is most commonly diagnosed in children between the ages of 2 and 5, with a slight male predominance. However, it can occur at any age. There are several risk factors associated with the development of ALL, including exposure to high levels of radiation or certain chemicals, such as benzene. Genetic factors also play a role, as certain genetic disorders, such as Down syndrome, are associated with an increased risk of ALL. Additionally, a family history of leukemia or a sibling with ALL can increase the risk of developing the disease.
Diagnostic Tools and Techniques
Clinical Presentation and Symptoms
The clinical presentation of ALL can vary, but common symptoms include fatigue, pale skin, frequent infections, easy bruising or bleeding, bone or joint pain, swollen lymph nodes, and weight loss. These symptoms are often non-specific and can be attributed to other conditions, making diagnosis challenging.
Laboratory Tests
Laboratory tests are used to confirm the diagnosis of ALL. Complete blood count (CBC) can reveal a low red blood cell count (anemia), low platelet count (thrombocytopenia), and abnormal white blood cell count. Blood smears can be examined under a microscope to look for abnormal lymphocytes. Additional tests, such as flow cytometry and immunophenotyping, are used to further characterize the leukemia cells and establish a definitive diagnosis.
Imaging and Biopsy
Imaging techniques, such as X-rays, ultrasounds, and computed tomography (CT) scans, are used to detect the extent of the disease and identify any abnormalities in the bones, organs, or lymph nodes. In some cases, a bone marrow biopsy may be necessary to determine the percentage of leukemia cells in the bone marrow and to assess the response to treatment.
Advancements in Treatment Approaches
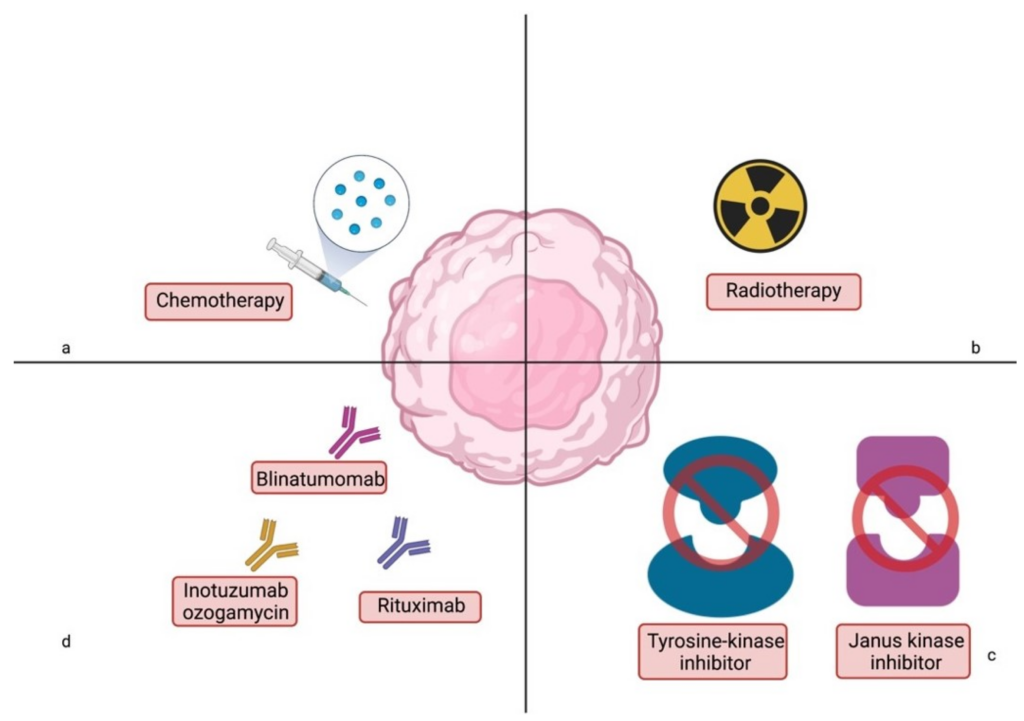
Chemotherapy
Chemotherapy is the mainstay of treatment for ALL. It involves the use of powerful drugs to kill cancer cells and prevent their growth. Chemotherapy is typically given in cycles, with periods of treatment followed by periods of rest to allow the body to recover. The specific combinations of drugs and the duration of treatment vary depending on the patient’s risk factors and response to therapy.
Targeted Therapy
Targeted therapy is a newer approach to treating ALL. It involves the use of drugs that specifically target cancer cells while sparing the healthy cells. These drugs work by interfering with specific molecules or pathways that are essential for cancer cell growth and survival. By targeting these specific abnormalities, targeted therapy can be more effective and cause fewer side effects than traditional chemotherapy.
Immunotherapy
Immunotherapy is another innovative treatment approach for ALL. It harnesses the power of the immune system to fight cancer cells. One type of immunotherapy involves the use of antibodies that recognize and bind to specific proteins on the surface of cancer cells, marking them for destruction by the immune system. Another type of immunotherapy involves the use of chimeric antigen receptor (CAR) T-cell therapy, where a patient’s own immune cells are modified to express a receptor that recognizes and kills cancer cells.
Stem Cell Transplantation
Stem cell transplantation, also known as a bone marrow transplant, is a potentially curative treatment option for patients with high-risk or relapsed ALL. It involves replacing the patient’s damaged bone marrow with healthy stem cells from a donor. The transplanted stem cells can develop into healthy blood cells and help rebuild the immune system. However, stem cell transplantation carries significant risks and requires careful matching of the donor and recipient.
Risk Stratification and Personalized Medicine
Patient Risk Stratification
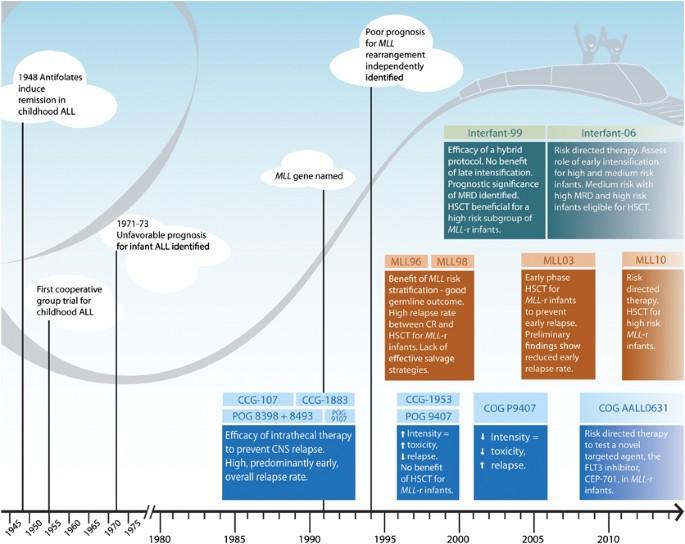
Risk stratification is an important step in determining the most appropriate treatment approach for each patient. Patients with ALL are classified into different risk groups based on various factors, such as age, white blood cell count at diagnosis, presence of specific genetic abnormalities, and response to initial treatment. This stratification helps to guide treatment decisions and optimize outcomes.
Molecular Subtyping
Molecular subtyping is a technique that allows for the classification of ALL based on the specific genetic abnormalities present in the leukemia cells. This information provides valuable insights into the biology of the disease and can help predict the response to certain treatments. Molecular subtyping can also identify potential targets for novel therapies and guide the development of personalized treatment approaches.
Genomic Profiling
Genomic profiling involves the analysis of a patient’s entire genome to identify genetic mutations or abnormalities that may be driving the development and progression of ALL. This comprehensive approach provides a more complete picture of the genetic landscape of the disease and can uncover potential therapeutic targets. Genomic profiling is an evolving field that holds great promise for improving the diagnosis and treatment of ALL.
Minimal Residual Disease Monitoring
Importance of Minimal Residual Disease (MRD) Assessment
Minimal Residual Disease (MRD) refers to the presence of small amounts of leukemia cells that remain undetectable after initial treatment. MRD assessment is a powerful prognostic tool that helps to predict the risk of relapse and guide treatment decisions. In patients who achieve MRD negativity, the risk of relapse is significantly reduced, while persistent MRD positivity indicates a higher risk of relapse and may warrant more aggressive therapy.
Methods for MRD Monitoring
There are several methods available for MRD monitoring, including flow cytometry, polymerase chain reaction (PCR), and next-generation sequencing (NGS). Flow cytometry is often used for quick and reliable detection of MRD in the bone marrow or peripheral blood. PCR and NGS are more sensitive techniques that can detect very low levels of residual disease. These methods enable clinicians to closely monitor the response to treatment and adjust therapy accordingly.
Supportive Care and Management of Side Effects
Prevention and Treatment of Infections
Patients with ALL are at an increased risk of infections due to the suppression of the immune system by chemotherapy. Therefore, it is important to take proactive measures to prevent infections, such as maintaining good hygiene, avoiding contact with sick individuals, and receiving appropriate vaccinations. In the event of an infection, prompt treatment with antibiotics or antifungal agents may be necessary to prevent complications.
Supportive Measures for Hematopoietic Toxicity
Chemotherapy can cause hematopoietic toxicity, resulting in low blood cell counts. Supportive measures, such as red blood cell and platelet transfusions, growth factors to stimulate white blood cell production, and the use of colony-stimulating factors, can help manage these side effects and minimize the impact on the patient’s well-being.
Management of Central Nervous System (CNS) Involvement
ALL has a predilection for spreading to the central nervous system (CNS). Prophylactic therapy, such as intrathecal chemotherapy, is often administered to prevent CNS relapse. In cases where there is already CNS involvement, radiation therapy or higher doses of intrathecal chemotherapy may be required to eradicate the disease.
Psychosocial Support for Patients and Families
The diagnosis and treatment of ALL can have a significant emotional and psychosocial impact on patients and their families. It is important to provide comprehensive support, including access to counseling services, support groups, and educational resources. Psychosocial support can help patients and families cope with the challenges of diagnosis, treatment, and survivorship.
Relapse and Salvage Therapy
Factors Affecting Risk of Relapse
Several factors can influence the risk of relapse in patients with ALL, including the initial response to treatment, the presence of specific genetic abnormalities, and the presence of MRD. Patients who achieve complete remission with minimal residual disease negativity have a lower risk of relapse, while those with persistent MRD positivity or certain high-risk genetic abnormalities have a higher risk of relapse.
Treatment Strategies for Relapsed ALL
Treatment strategies for relapsed ALL depend on several factors, including the patient’s age, initial risk group, time to relapse, and previous treatment exposures. Options may include intensifying chemotherapy, targeted therapies, immunotherapy, stem cell transplantation, or participation in clinical trials. The goal of salvage therapy is to achieve another remission and possibly proceed to curative treatment.
Novel Therapies for Salvage Treatment
With advancements in research, novel therapies are being developed for the treatment of relapsed ALL. These therapies include targeted agents that specifically inhibit the signaling pathways involved in cancer growth, immunotherapies that enhance the immune system’s ability to recognize and eliminate cancer cells, and gene therapies that modify a patient’s own immune cells to kill leukemia cells more effectively.
Long-Term Follow-Up and Survivorship
Monitoring for Late Effects
Survivors of ALL require long-term follow-up care to monitor for potential late effects of treatment. These can include cardiovascular problems, secondary cancers, infertility, neurocognitive impairment, and endocrine dysfunction. Regular screenings and surveillance are essential to identify and manage these late effects early, improving the overall quality of life for survivors.
Quality of Life and Psychosocial Outcomes
Improving the quality of life for ALL survivors is a crucial aspect of long-term care. This involves addressing physical, psychosocial, and emotional needs, providing educational support, and ensuring smooth transitions into adulthood. By providing holistic care and support, healthcare professionals can help survivors flourish in their personal and professional lives.
Transition to adult care
The transition from pediatric to adult care can be challenging for ALL survivors as they navigate a new healthcare system and assume greater responsibility for their own healthcare. A structured transition program, involving multidisciplinary healthcare teams, can help facilitate the process and ensure continuity of care. Open communication and education are key components to empower survivors in managing their health.
Supporting Research Initiatives
National and International Collaborative Efforts
Acute Lymphoblastic Leukemia research relies heavily on national and international collaborative efforts. Collaboration allows researchers to pool resources, share data, and accelerate the development of new treatment strategies. Collaborative networks such as the Children’s Oncology Group (COG) and the International BFM Study Group are vital in conducting large-scale clinical trials and collecting comprehensive data to guide future research.
Funding and Grants for ALL Research
Research in the field of Acute Lymphoblastic Leukemia heavily relies on funding and grants. Organizations such as the National Cancer Institute (NCI), the Leukemia & Lymphoma Society (LLS), and various philanthropic foundations play a crucial role in providing financial support to researchers and institutions. These funds are essential for conducting clinical trials, advancing scientific discoveries, and improving outcomes for ALL patients.
Future Directions and Promising Research
Advancements in Genomic Medicine
Genomic medicine holds great promise for the future of Acute Lymphoblastic Leukemia research. By analyzing the entire genome of leukemia cells, researchers can identify new genetic abnormalities and pathways involved in disease progression. This knowledge will lead to the development of targeted therapies and personalized treatment approaches, ultimately improving outcomes for patients with ALL.
Precision Medicine Approaches
Precision medicine aims to tailor treatment based on the individual characteristics of each patient and their disease. This approach takes into account factors such as genetic mutations, molecular subtypes, and response to therapy. By utilizing precision medicine approaches, clinicians will be able to choose the most effective and least toxic treatments for each patient, maximizing therapeutic outcomes.
Immunotherapy Innovations
Immunotherapy continues to evolve and holds promise for the treatment of ALL. Ongoing research is focused on developing new immunotherapies, improving the durability of response, and minimizing side effects. Strategies such as combining immunotherapies with other treatment modalities and enhancing the persistence and function of immune cells show great potential in achieving long-term remissions and ultimately curing ALL.
Biology and Pathogenesis Studies
Understanding the biology and pathogenesis of Acute Lymphoblastic Leukemia is critical for the development of targeted therapies and effective treatment approaches. Researchers are investigating the underlying mechanisms that drive the development and progression of ALL, including genetic mutations, epigenetic modifications, and aberrant signaling pathways. By elucidating these processes, novel therapeutic targets can be identified and exploited.
Acute Lymphoblastic Leukemia is a complex disease that requires a multidisciplinary approach for diagnosis, treatment, and long-term management. With advancements in research and technology, there have been significant improvements in our understanding and treatment of ALL. Through ongoing collaborations, funding support, and innovative research, the future holds great promise for further advancements in the field, ultimately leading to improved outcomes and quality of life for patients with Acute Lymphoblastic Leukemia.
Watch This Video Below
Related Terms About Advancements in Research for Acute Lymphoblastic Leukemia in Children
Advances In Leukemia Research And Treatment, Recent Advances In The Treatment Of Acute Lymphoblastic Leukemia, What Is Advanced Leukemia