Have you ever experienced that annoying itchiness, burning sensation, and redness between your toes or on the soles of your feet? If so, you might have fallen victim to a common fungal infection known as Athlete’s Foot. This pesky condition, occurring primarily in athletes (hence the name), can also affect anyone who spends long periods in damp environments, such as communal showers or swimming pools. This article will shed light on the causes and symptoms of Athlete’s Foot, providing you with valuable information to understand and tackle this itchy irritation head-on.
Causes of Athlete’s Foot
Fungal Infection
Athlete’s foot, also known as tinea pedis, is primarily caused by a fungal infection. The fungus responsible for this condition can be found in warm and moist environments such as public showers, locker rooms, and swimming pools. When your feet come into contact with these contaminated surfaces, the fungus can easily enter your skin, leading to the development of athlete’s foot.
Direct Contact
Direct contact with someone who already has athlete’s foot can also be a cause of this condition. Whether it’s through sharing towels, socks, or shoes, the infection can easily spread from one person to another. It’s important to be cautious and practice good hygiene, especially when it comes to sharing personal items with others.
Warm and Moist Environment
Athlete’s foot thrives in warm and moist environments, as these conditions provide the perfect breeding ground for the fungus. This is why places like public showers and swimming pools, where humidity levels are high, are common sources of infection. Additionally, wearing shoes that do not allow proper airflow can create a warm and moist environment inside your shoes, making you more susceptible to developing athlete’s foot.
Risk Factors
Wearing Tight Shoes
Wearing tight-fitting shoes, especially for extended periods, can increase your risk of developing athlete’s foot. Tight shoes can cause excessive sweating and a buildup of moisture, creating an ideal environment for the fungal infection to thrive. Opt for shoes that provide proper ventilation and allow your feet to breathe.
Walking Barefoot in Public Places
Walking barefoot in public places, such as locker rooms, gyms, and communal showers, puts you at a higher risk of coming into contact with the fungus that causes athlete’s foot. The floors in these areas can be hotbeds for fungal infections, so it’s best to wear protective footwear, such as flip-flops or shower shoes, to minimize the risk.
Poor Hygiene
Poor hygiene practices, such as not washing your feet regularly or not changing your socks and shoes frequently, can contribute to the development of athlete’s foot. Keeping your feet clean and dry is crucial in preventing the growth of the fungus. Make sure to wash your feet daily, dry them thoroughly, and change into clean socks and shoes regularly.
Sweating Profusely
Excessive sweating, particularly on your feet, can increase your susceptibility to athlete’s foot. Sweating creates a moist environment that promotes fungal growth. If you tend to sweat profusely, it’s essential to take extra precautions, such as using antifungal powder or wearing moisture-wicking socks to keep your feet dry.
Having a Weakened Immune System
Individuals with compromised immune systems, such as those with diabetes, HIV/AIDS, or undergoing immune-suppressing treatments, are more susceptible to developing athlete’s foot. A weakened immune system makes it harder for the body to fight off infections, including fungal infections like athlete’s foot. It’s crucial for individuals with weak immune systems to take extra care and preventive measures to minimize their risk.
Symptoms of Athlete’s Foot
Itching and Burning Sensation
One of the most common symptoms of athlete’s foot is persistent itching and a burning sensation on the affected area. The itching can be intense and may worsen over time if left untreated. This discomfort is often a result of the fungus irritating the skin.
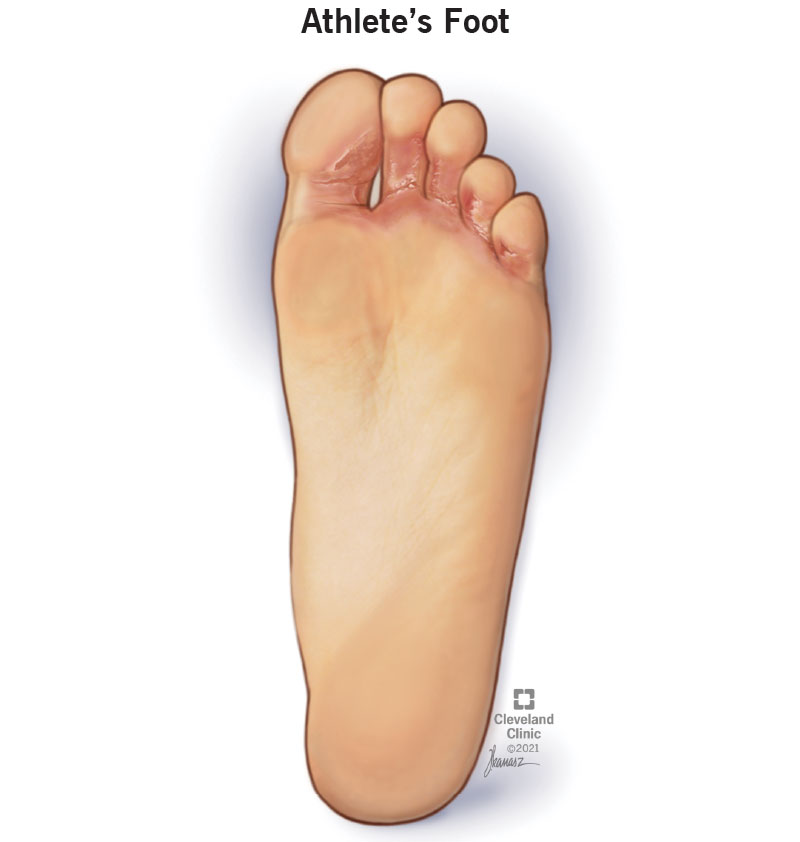
Redness and Peeling Skin
Athlete’s foot can cause redness and the skin to become dry and flaky, leading to peeling. The affected areas may appear scaly and may peel in small flakes. The redness and peeling skin are typically concentrated in between the toes, but it can also spread to other parts of the feet.
Cracked or Blistered Skin
In severe cases, athlete’s foot can lead to cracked or blistered skin. The constant itching and irritation can cause the skin to break, leaving painful cracks or blisters. This can increase the risk of secondary infections.
Dryness and Scaling
Dryness and scaling are common symptoms of athlete’s foot. The affected skin may appear dry and rough, with visible scaly patches or areas of flaking. The dryness and scaling are often accompanied by persistent itching.
Foul Odor
Another telltale symptom of athlete’s foot is a foul odor coming from the infected area. The excessive moisture and bacterial growth caused by the fungal infection can produce an unpleasant smell. It’s important to address the underlying fungal infection to alleviate the odor.
Diagnosis
Physical Examination
To diagnose athlete’s foot, a healthcare professional will typically perform a physical examination of the affected area. They will inspect your feet for any visible signs of infection such as redness, peeling skin, or blisters. They may also ask about your symptoms and medical history to rule out other possible causes.
Laboratory Testing
In some cases, a healthcare professional may order laboratory tests to confirm the diagnosis of athlete’s foot. These tests may involve taking a skin scraping or a sample of the affected area for microscopic examination or culturing. These tests can identify the specific fungus causing the infection and help guide the most appropriate treatment approach.
Treatment Options
Topical Antifungal Medications
For mild to moderate cases of athlete’s foot, topical antifungal medications are usually the first line of treatment. These medications, available as creams, lotions, or sprays, contain antifungal agents that effectively kill the fungus and relieve symptoms. It’s important to follow the instructions provided by your healthcare professional and continue using the medication for the recommended duration to ensure complete eradication of the infection.
Oral Antifungal Medications
In more severe or persistent cases, oral antifungal medications may be prescribed. These medications are taken by mouth and work to eliminate the fungus from the inside out. Oral antifungal medications are generally reserved for cases that do not respond well to topical treatments or when the infection has spread beyond the feet.
Home Remedies
Several home remedies can help alleviate the symptoms of athlete’s foot and promote healing. Tea tree oil, known for its antifungal properties, can be applied topically to the affected area. Apple cider vinegar soaks, using a diluted solution, can help rebalance the skin’s pH and inhibit fungal growth. Baking soda paste can be soothing and help relieve itchiness. Garlic, when crushed and applied to the affected area, may also help combat the infection due to its antifungal properties. However, it’s important to note that home remedies should not replace medical treatments, especially in severe cases.
Preventive Measures
Preventive measures are essential in reducing the risk of athlete’s foot recurrence. Good hygiene practices, such as washing your feet daily with soap and water, drying them thoroughly (especially between the toes), and changing into clean socks and shoes regularly, can help prevent the growth of fungus. Additionally, wearing breathable shoes and socks, avoiding walking barefoot in public places, and using antifungal powder or spray can significantly lower your risk of developing athlete’s foot.
Complications
Cellulitis
If left untreated or improperly managed, athlete’s foot can lead to complications such as cellulitis. Cellulitis is a bacterial skin infection that occurs when bacteria enter the cracked or broken skin caused by the fungal infection. The affected area may become swollen, red, warm to the touch, and painful. Prompt medical attention is necessary to treat cellulitis and prevent the infection from spreading.
Bacterial Infections
Secondary bacterial infections can occur when the skin is compromised by the underlying fungal infection. These bacterial infections can cause additional symptoms such as increased pain, pus-filled blisters, and fever. It’s important to address the fungal infection promptly to minimize the risk of bacterial complications.
Toenail Fungus
Athlete’s foot can spread to the toenails, leading to fungal nail infections. This condition, also known as onychomycosis, can cause the toenails to become thick, discolored, and brittle. Treating both the athlete’s foot and toenail fungus simultaneously is crucial to prevent the spread of infection and promote overall healing.

When to See a Doctor
Persistent Infection
If your athlete’s foot symptoms persist despite using over-the-counter antifungal treatments, it’s important to seek medical attention. A healthcare professional can assess the severity of the infection and prescribe stronger antifungal medications if necessary.
Spread to Other Body Parts
If the infection spreads beyond the feet and affects other body parts, such as the hands or groin, it’s crucial to see a doctor. These areas are susceptible to fungal infections as well, and appropriate treatment is necessary to prevent further spread.
Diabetes or Weakened Immune System
Individuals with diabetes or a weakened immune system should consult a healthcare professional if they suspect they have athlete’s foot. These conditions can make it more challenging to manage the infection effectively, and prompt medical attention is essential to prevent complications.
Prevention Tips
Keep Feet Clean and Dry
Maintaining good foot hygiene is crucial in preventing athlete’s foot. Wash your feet daily with soap and water, paying special attention to the spaces between your toes. After washing, dry your feet thoroughly, especially between the toes, as moisture can encourage fungal growth.
Wear Breathable Shoes and Socks
Choosing shoes that allow proper ventilation and opting for moisture-wicking socks can help keep your feet dry. Avoid wearing tight shoes or those made of synthetic materials that can trap moisture and contribute to the growth of fungus.
Avoid Walking Barefoot in Public Places
To minimize the risk of coming into contact with the fungus that causes athlete’s foot, avoid walking barefoot in public places such as locker rooms, gyms, and communal showers. Wear protective footwear like flip-flops or shower shoes.
Use Antifungal Powder or Spray
Using antifungal powder or spray on your feet can help create a hostile environment for the fungus. These products can help absorb moisture and inhibit fungal growth. Apply them to your feet, focusing on the spaces between your toes, before putting on socks and shoes.
Change Shoes and Socks Regularly
Regularly changing your shoes and socks can help prevent the buildup of moisture and increase ventilation for your feet. Alternate between different pairs of shoes to allow them time to dry thoroughly between uses.

Natural Remedies
Tea Tree Oil
Tea tree oil is a natural remedy that is known for its antifungal properties. Dilute tea tree oil with a carrier oil, such as coconut oil, and apply it to the affected areas of your feet. Make sure to test a small area first for any adverse reactions and discontinue use if you experience any irritation.
Apple Cider Vinegar Soak
An apple cider vinegar soak can help rebalance the pH of your skin and inhibit fungal growth. Mix equal parts of apple cider vinegar and water in a basin or tub, and soak your feet for 15-20 minutes. Pat your feet dry thoroughly afterward.
Baking Soda Paste
Baking soda can help soothe itchiness and promote dryness. Mix baking soda with water to create a paste and apply it to the affected areas of your feet. Leave it on for 10-15 minutes before rinsing it off.
Garlic
Garlic is believed to have antifungal properties. Crush a few cloves of garlic and apply the paste to the affected areas of your feet. Leave it on for 30 minutes before rinsing it off. If you experience any irritation, discontinue use.
Conclusion
Athlete’s foot, although common, can be bothersome and uncomfortable. The causes of this condition include fungal infections, direct contact with infected individuals or surfaces, and warm and moist environments. Various risk factors, such as tight shoes, poor hygiene, excessive sweating, and a weakened immune system, can increase the likelihood of developing athlete’s foot.
Recognizing the symptoms of athlete’s foot, including itching, burning, redness, peeling skin, cracked skin, and foul odor, is essential for early intervention and treatment. Proper diagnosis often involves a physical examination and, in some cases, laboratory testing.
Treatment options range from topical antifungal medications, oral antifungal medications, to home remedies. Preventive measures, such as maintaining good foot hygiene, wearing breathable shoes and socks, and avoiding walking barefoot in public places, can significantly reduce the risk of athlete’s foot recurrence.
While natural remedies may provide some relief and promote healing, it’s essential to consult a healthcare professional, particularly in severe or persistent cases. Complications of athlete’s foot, such as cellulitis, bacterial infections, and toenail fungus, can occur if left untreated.
If your symptoms persist, spread to other body parts, or you have an underlying condition like diabetes or a weakened immune system, seeking medical attention is crucial. Remember, prevention is key, and adopting simple preventive measures can help you keep your feet healthy and free from athlete’s foot.