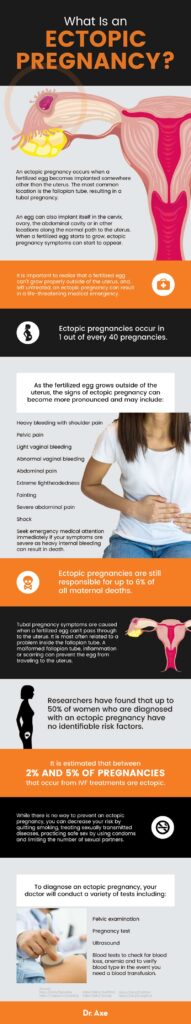
Are you aware of the potential risks and precautions associated with ectopic pregnancies? In this article, we will shed light on the complications that can arise from this condition. An ectopic pregnancy occurs when a fertilized egg implants outside of the uterus, usually in the fallopian tubes. While this can be a concerning situation, understanding the risks involved and taking necessary precautions can help ensure a healthy outcome. So, let’s explore the various complications that may arise and discover the measures you can take to minimize them.

1. Ruptured Ectopic Pregnancy
Ectopic pregnancy is a serious condition that occurs when a fertilized egg implants outside of the uterus, most commonly in the fallopian tubes. A ruptured ectopic pregnancy, also known as a tubal rupture, is a potentially life-threatening complication that requires immediate medical attention.
1.1 Symptoms of a Ruptured Ectopic Pregnancy
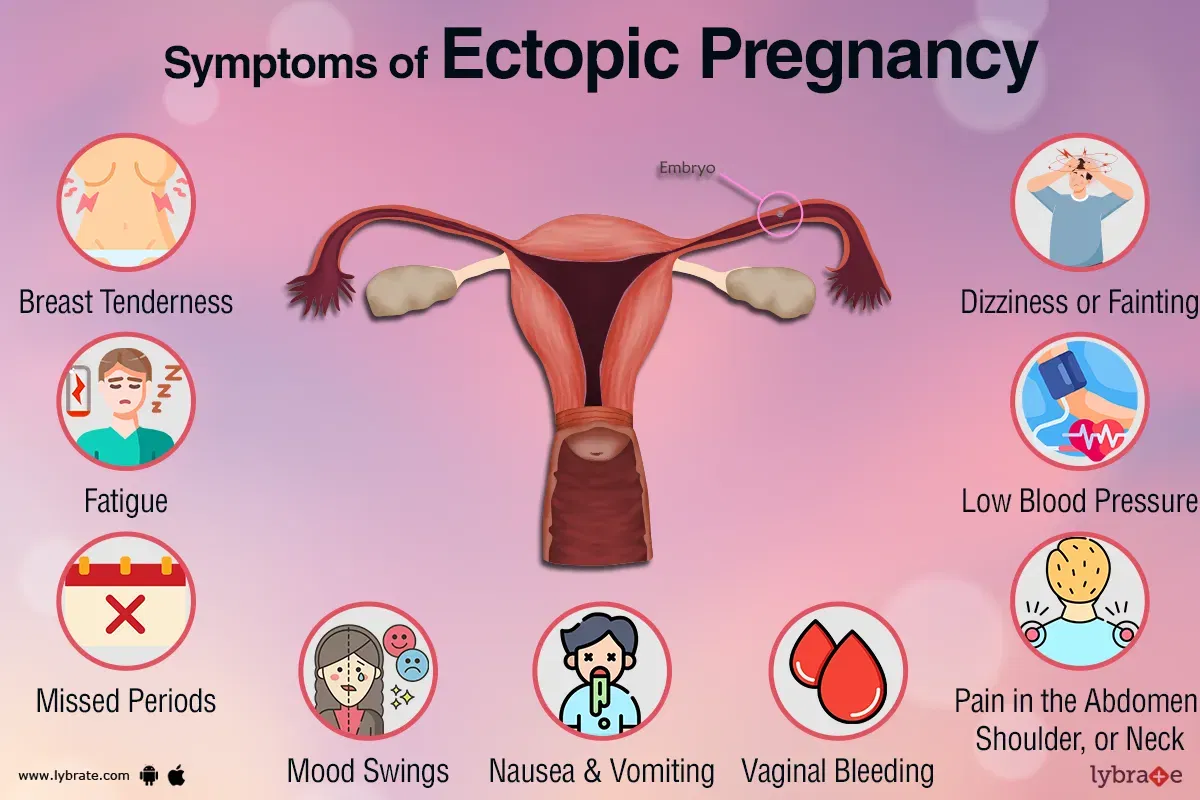
Recognizing the symptoms of a ruptured ectopic pregnancy is crucial for seeking prompt medical care. Some common symptoms include:
- Severe abdominal pain, often on one side
- Vaginal bleeding, which may be heavy or light
- Shoulder pain
- Dizziness or fainting
- Rectal pressure
- Intense cramping
If you experience any of these symptoms, it is essential to seek emergency medical help immediately.
1.2 Emergency Treatment for Ruptured Ectopic Pregnancy
When a ruptured ectopic pregnancy is suspected, emergency medical treatment is necessary to prevent severe complications. The goals of emergency treatment include stopping internal bleeding, removing the ectopic pregnancy, and preserving fertility whenever possible.
Typically, surgery is the preferred method of treatment for a ruptured ectopic pregnancy. The type of surgery performed will depend on the severity of the rupture and the overall health of the individual. In some cases, emergency surgery may involve removing the affected fallopian tube.
1.3 Potential Complications of a Ruptured Ectopic Pregnancy
A ruptured ectopic pregnancy can lead to several potential complications. These may include:
- Hemorrhage: The rupture can cause significant internal bleeding, which may require blood transfusions.
- Shock: Severe bleeding can result in a state of shock, which requires immediate medical intervention.
- Infection: The rupture of the ectopic pregnancy may increase the risk of pelvic infection, requiring antibiotics.
- Scarring: The fallopian tube may become scarred as a result of the rupture, affecting future fertility.
If you have experienced a ruptured ectopic pregnancy, it is crucial to follow up with your healthcare provider to monitor for any potential complications and discuss future fertility options.
2. Recurrent Ectopic Pregnancy
While ectopic pregnancies are generally rare occurrences, some individuals may experience recurrent ectopic pregnancies. Understanding the causes and management of recurrent ectopic pregnancy is essential for those who have had multiple instances of this condition.
2.1 Causes of Recurrent Ectopic Pregnancy
Several factors may contribute to recurrent ectopic pregnancy, including:
- Previous tubal surgery: Prior surgical interventions, such as tubal ligation or tubal repair, may increase the risk of recurrent ectopic pregnancy.
- Pelvic inflammatory disease: Infections of the reproductive organs can lead to scarring and blockages in the fallopian tubes.
- Smoking: Tobacco use has been associated with an increased risk of ectopic pregnancy.
- Hormonal imbalances: Certain hormonal imbalances, such as those associated with polycystic ovary syndrome (PCOS), may increase the risk of ectopic pregnancy.
Understanding the underlying causes of recurrent ectopic pregnancy can help healthcare providers develop appropriate management and treatment plans.
2.2 Management and Treatment of Recurrent Ectopic Pregnancy
The management of recurrent ectopic pregnancy may involve a combination of medical and surgical interventions. Some common approaches include:
- Repeat surgery: If the recurrence is due to additional issues with the fallopian tubes, further surgical interventions may be necessary to remove or repair the affected tubes.
- Assisted reproductive techniques: In cases where both fallopian tubes are damaged or removed, in vitro fertilization (IVF) may be considered.
- Methotrexate therapy: Medications like methotrexate may be used to treat recurrent ectopic pregnancy, especially if the ectopic pregnancies are detected early and have not yet caused a rupture.
The appropriate management and treatment options for recurrent ectopic pregnancy will depend on individual factors, such as the location and severity of the ectopic pregnancies, overall health, and future fertility goals.
2.3 Prevention of Recurrent Ectopic Pregnancy
Preventing recurrent ectopic pregnancy involves addressing underlying causes and risk factors. Some preventive measures may include:
- Smoking cessation: Quitting smoking can significantly reduce the risk of ectopic pregnancy and its recurrence.
- Prompt treatment of infections: Timely treatment of pelvic inflammatory disease and other infections can help prevent scarring and damage to the fallopian tubes.
- Regular medical check-ups: Routine gynecological examinations and screenings can aid in the early detection and management of potential reproductive health issues.
- Consideration of contraception: For individuals who have experienced recurrent ectopic pregnancy, discussing different contraceptive methods with a healthcare provider is essential to reduce the risk of future ectopic pregnancies.
Implementing these preventive measures can help reduce the chances of recurrent ectopic pregnancy and improve overall reproductive health.
3. Fertility Issues
Ectopic pregnancy can have various impacts on fertility. It is important to understand these effects and explore fertility enhancement techniques for individuals who may want to conceive in the future.
3.1 Impact of Ectopic Pregnancy on Fertility
While ectopic pregnancy itself does not cause infertility, it may significantly affect future fertility. The potential impacts on fertility include:
- Damaged fallopian tubes: Ectopic pregnancy can cause scarring and damage to the fallopian tubes, making it difficult for the egg to travel from the ovary to the uterus.
- Reduced egg quality: The inflammation and trauma associated with ectopic pregnancy can potentially impact the quality of the remaining eggs and reduce the chances of successful conception.
- Risk of recurrent ectopic pregnancy: Individuals who have had an ectopic pregnancy have an increased risk of experiencing it again in future pregnancies.
Understanding the effects of ectopic pregnancy on fertility is essential in order to make informed decisions regarding future conception plans.
3.2 Assisted Reproduction Techniques for Fertility Enhancement
For individuals experiencing fertility issues after an ectopic pregnancy, assisted reproduction techniques may offer potential solutions. Depending on individual circumstances and the extent of the fertility issues, options may include:
- In vitro fertilization (IVF): IVF involves the fertilization of eggs in a laboratory setting and the subsequent transfer of embryos to the uterus.
- Gamete intrafallopian transfer (GIFT): GIFT involves placing eggs and sperm directly into the fallopian tubes to allow for natural fertilization.
- Intrauterine insemination (IUI): IUI involves placing prepared sperm directly into the uterus during ovulation to increase the chances of fertilization.
Assisted reproduction techniques can help individuals with fertility issues after ectopic pregnancy achieve their desired pregnancy outcomes.
4. Psychological Effects of Ectopic Pregnancy
Experiencing an ectopic pregnancy can have significant emotional and psychological impacts on individuals. It is essential to recognize these effects and seek appropriate support and professional help when needed.
4.1 Emotional and Psychological Impact on Individuals
Ectopic pregnancy can be a traumatic experience, causing a range of emotions and psychological effects. Some common emotional responses may include:
- Grief and sadness: The loss of a pregnancy can result in deep feelings of grief and sadness.
- Guilt and self-blame: Some individuals may feel guilty or blame themselves for the ectopic pregnancy, even though it is beyond their control.
- Anxiety and fear: Those who have experienced an ectopic pregnancy may feel anxious and afraid about the potential risks and complications of future pregnancies.
It is important to acknowledge and address these emotions, as they can significantly impact mental well-being and overall quality of life.
4.2 Seeking Support and Professional Help
Seeking support from loved ones and professional help can be instrumental in coping with the psychological effects of ectopic pregnancy. Consider the following options:
- Support groups: Joining support groups or online communities can provide a space to connect with individuals who have experienced similar situations, offering understanding and encouragement.
- Counseling or therapy: Speaking with a mental health professional can help individuals process their emotions, develop coping strategies, and work through feelings of grief, guilt, and anxiety.
- Open communication: Sharing your experiences and emotions with trusted friends, family members, or your partner can provide a source of support.
Remember, seeking support is not a sign of weakness but rather a strength in navigating the emotional journey of healing after ectopic pregnancy.

5. Blood Loss and Anemia
Excessive bleeding is a significant concern in ectopic pregnancy and can lead to the development of anemia. Understanding the risks and management of blood loss is crucial for individuals who have experienced or are at risk of ectopic pregnancy.
5.1 Excessive Bleeding and Risk of Anemia
Ectopic pregnancy can cause internal bleeding if the fallopian tube ruptures or if there is bleeding within the abdominal cavity. Excessive bleeding poses a risk of developing anemia, a condition characterized by a decrease in the number of red blood cells or hemoglobin.
Anemia can lead to symptoms such as fatigue, weakness, shortness of breath, dizziness, and pale skin. It is important to monitor blood loss and address anemia promptly to prevent further complications.
5.2 Management of Blood Loss during Ectopic Pregnancy
Managing and preventing excessive blood loss during ectopic pregnancy requires prompt medical intervention. The following measures may be taken:
- Blood transfusions: If blood loss is significant, a blood transfusion may be necessary to restore red blood cell count and prevent anemia.
- Intravenous fluids: Administering intravenous fluids can help maintain blood pressure and support circulation.
- Surgical intervention: Surgery is often required to stop the bleeding and remove the ectopic pregnancy, preventing further blood loss.
It is crucial to prioritize medical care and closely monitor blood loss to prevent complications like anemia and ensure a safe recovery.
6. Adhesions and Scarring
Adhesions and scarring can occur as a result of the inflammation and trauma associated with ectopic pregnancy. Understanding the consequences of adhesions and scarring and exploring management options is important for individuals affected by this condition.
6.1 Consequences of Adhesions and Scarring
Adhesions are bands of scar tissue that form between nearby organs or tissues, causing them to stick together. Adhesions can lead to various complications, including:
- Chronic pelvic pain: Adhesions in the pelvic region can cause ongoing pain and discomfort.
- Bowel and bladder problems: Adhesions can result in blocked or twisted intestines, leading to bowel obstruction or urinary problems.
- Fertility issues: Scarring and adhesions in the fallopian tubes can hinder the passage of eggs, impairing fertility.
Understanding the potential consequences of adhesions and scarring is essential for making informed decisions about management and treatment.
6.2 Management and Treatment Options for Adhesions
The management and treatment of adhesions depend on their severity and the impact on an individual’s health and fertility. Some options may include:
- Laparoscopic surgery: Minimally invasive procedures can be performed to remove or reduce adhesions, improving fertility and alleviating pain.
- Physical therapy: Techniques such as pelvic floor physical therapy can help manage pain and improve mobility in individuals with pelvic adhesions.
- Assisted reproduction techniques: In cases where the fallopian tubes are severely damaged, assisted reproduction techniques like IVF can bypass the need for fallopian tube function.
It is important to consult with a healthcare provider to determine the most appropriate management and treatment options based on individual circumstances and symptoms.

7. Ectopic Pregnancy in Fallopian Tube Stump
While rare, ectopic pregnancy can occur in the fallopian tube stump after a previous tubal surgery, such as a tubal ligation or tubal removal. Understanding the causes, risk factors, and treatment options is crucial for individuals who have undergone tubal surgery and may be at risk.
7.1 Causes and Risk Factors
Ectopic pregnancy in the fallopian tube stump can occur due to various factors, including:
- Incomplete tubal ligation or removal: If the tubal surgery was not performed correctly and a portion of the fallopian tube remains functional, ectopic pregnancy can occur in the residual fallopian tube.
- Tubal recanalization: Over time, the fallopian tube may spontaneously reconnect or recanalize, allowing for the passage of sperm and the implantation of a fertilized egg.
Individuals who have had tubal surgery, especially if it was performed many years ago, may be at a higher risk of ectopic pregnancy occurring in the fallopian tube stump.
7.2 Detection and Treatment Options
Detecting ectopic pregnancy in the fallopian tube stump can be challenging, as it may present symptoms similar to other types of ectopic pregnancies. Early diagnosis is critical for preventing complications. Some treatment options may include:
- Surgical removal: Surgical intervention is usually required to remove the ectopic pregnancy and the affected fallopian tube stump.
- Methotrexate therapy: In some cases, medications like methotrexate may be considered as an alternative to surgery, especially if the ectopic pregnancy is detected early and the tube stump is otherwise healthy.
It is important for individuals who have had tubal surgery to discuss the potential risks and monitoring strategies with their healthcare provider to ensure the early detection and appropriate treatment of ectopic pregnancy in the fallopian tube stump.
8. Ectopic Pregnancy in Cervix or Ovary
Although rare, ectopic pregnancies can occur in uncommon locations such as the cervix or ovary. Understanding the presentation, diagnosis, and treatment approaches for ectopic pregnancies in these locations is crucial for healthcare providers and individuals affected by this condition.
8.1 Uncommon Locations of Ectopic Pregnancy
Ectopic pregnancies in the cervix or ovary are considered unusual and pose unique challenges for detection and management. These uncommon locations may present with symptoms similar to those of more typical ectopic pregnancies but require specific diagnostic approaches.
Ectopic pregnancies in the cervix occur when the fertilized egg implants in the lower part of the uterus, in or near the cervix. Ectopic pregnancies in the ovary, often referred to as ovarian pregnancies, occur when the fertilized egg implants in or on the ovary.
8.2 Diagnosis and Treatment Approaches
It can be challenging to diagnose ectopic pregnancies in the cervix or ovary due to their rarity and atypical presentations. Some diagnostic methods that may be used include:
- Transvaginal ultrasound: This imaging technique can help visualize the location of the gestational sac and determine if it is in the cervix or ovary.
- Blood tests: Measuring the levels of pregnancy hormones, such as human chorionic gonadotropin (hCG), can provide additional information to support the diagnosis.
The treatment approach for ectopic pregnancies in the cervix or ovary will depend on the location, size, and overall health of the individual. Options may include surgical removal or, in some cases, medications like methotrexate.
Individuals with ectopic pregnancies in these uncommon locations require specialized medical care to ensure appropriate diagnosis, management, and treatment.
9. Future Pregnancy Concerns
After experiencing an ectopic pregnancy, individuals may have concerns about the chances of future ectopic pregnancies and the precautions that should be taken during subsequent pregnancies. Understanding the risks and necessary medical monitoring and care is important for those planning to conceive in the future.
9.1 Chances of Future Ectopic Pregnancies
Having an ectopic pregnancy in the past increases the risk of future ectopic pregnancies. The exact risk varies depending on individual factors, such as the cause of the initial ectopic pregnancy, the presence of remaining fallopian tubes, and overall reproductive health.
It is crucial to discuss the potential risk of subsequent ectopic pregnancies with healthcare providers to develop appropriate monitoring and care plans.
9.2 Precautions for Future Pregnancies
For individuals planning future pregnancies after experiencing an ectopic pregnancy, several precautions can be taken to optimize safety and minimize the risk of recurrence. These may include:
- Early prenatal care: Seeking early and regular prenatal care allows healthcare providers to closely monitor the pregnancy and detect any potential issues promptly.
- Close monitoring of hCG levels: Regular blood tests to monitor hCG levels can help confirm the viability and location of the pregnancy.
- Ultrasound examinations: Ultrasounds can provide visual confirmation of the pregnancy and allow healthcare providers to assess its location and progression.
- Consultation with a specialist: In some cases, referral to a fertility specialist or high-risk pregnancy specialist may be necessary to ensure specialized care and monitoring.
It is important to discuss these precautions and any additional recommendations with a healthcare provider to tailor a personalized plan for future pregnancies.
9.3 Medical Monitoring and Care during Future Pregnancies
During future pregnancies, individuals who have had an ectopic pregnancy may require additional medical monitoring and care. Regular check-ups, blood tests, and ultrasounds may be recommended to ensure the pregnancy’s progress and detect any signs of complications.
Working closely with healthcare providers and adhering to the recommended monitoring schedule can help ensure the best possible outcomes for future pregnancies.
10. Medical and Surgical Treatments
The treatment of ectopic pregnancy may involve both medical and surgical interventions. Understanding the available options and their implications is essential for individuals who require treatment for ectopic pregnancy.
10.1 Medications for Ectopic Pregnancy
In some cases, ectopic pregnancies can be treated with medication instead of surgery. Methotrexate is a common medication used to treat ectopic pregnancy. It works by stopping the growth of the pregnancy and gradually dissolving the tissue.
Medication therapy is typically an option for individuals who have an unruptured ectopic pregnancy with low levels of hCG, and the pregnancy is not located near blood vessels. It is important to closely follow the prescribed medication regimen and undergo regular monitoring to ensure the effectiveness of the treatment.
10.2 Surgical Procedures for Ectopic Pregnancy
Surgery is often required to remove an ectopic pregnancy, especially if it has already ruptured or poses a risk to the individual’s health. The surgical procedures commonly used for ectopic pregnancy are:
- Laparoscopy: A minimally invasive surgery performed through small incisions, allowing the surgeon to remove the ectopic pregnancy and, if necessary, repair any damage to the fallopian tubes.
- Laparotomy: A traditional surgical approach that involves a larger abdominal incision. Laparotomy is usually reserved for cases where the ectopic pregnancy is larger or more complex, or if there are concerns about internal bleeding.
The choice of surgical procedure will depend on factors such as the severity of the ectopic pregnancy, the presence of a rupture, and the surgeon’s expertise.
It is important to consult with a healthcare provider to determine the most appropriate treatment approach based on individual circumstances, overall health, and fertility goals.
In conclusion, ectopic pregnancy is a complex and challenging condition that requires immediate medical attention. Understanding the symptoms, potential complications, and available treatment options is crucial for those affected by ectopic pregnancy. By staying informed, seeking support, and working closely with healthcare providers, individuals can navigate the physical and emotional impacts of ectopic pregnancy while optimizing their future reproductive health.