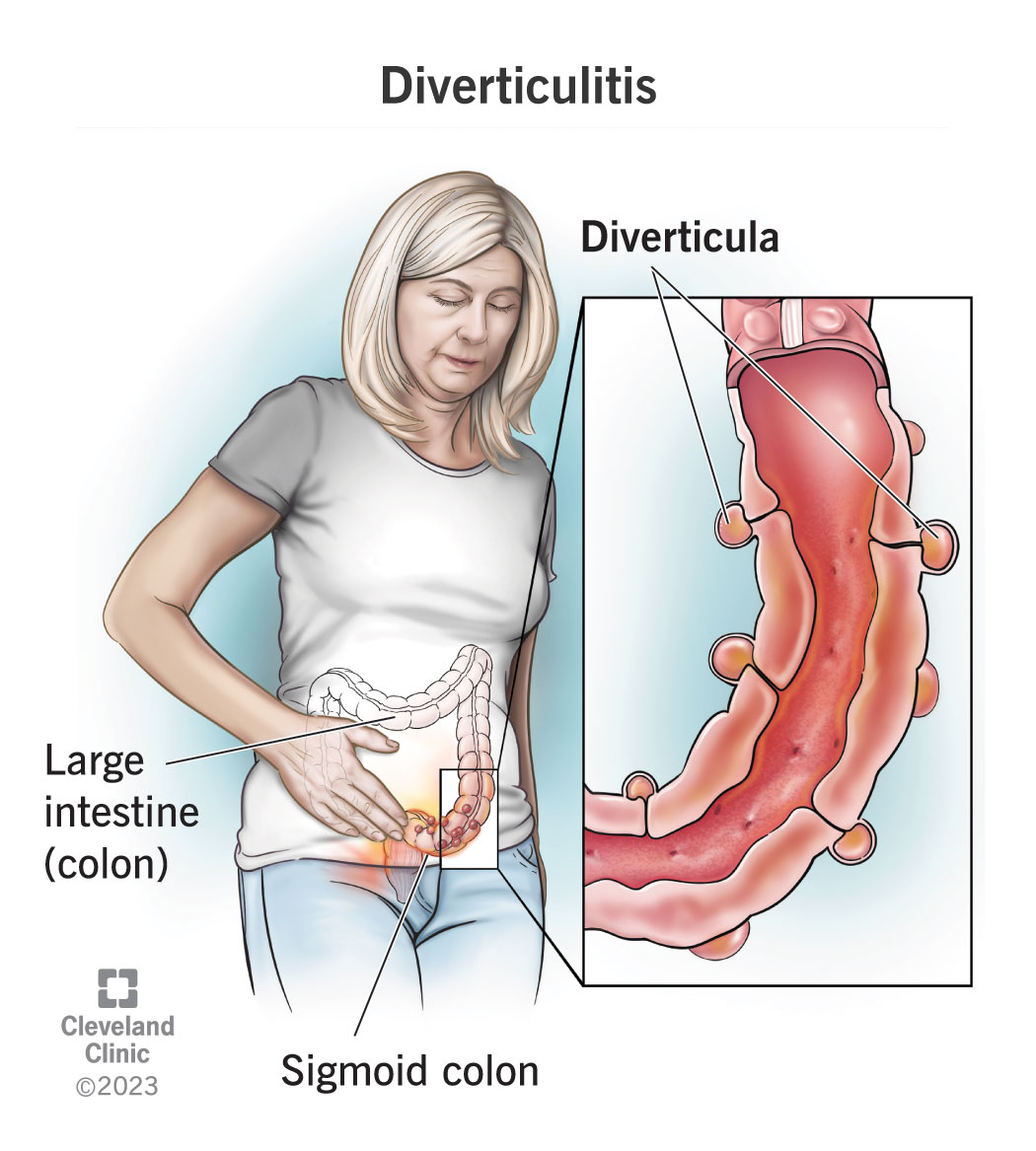
Are you or someone you know suffering from diverticulitis? Don’t worry, there is hope! In this article, we will explore the effective treatments available for diverticulitis, a condition characterized by inflamed pouches in the lining of the large intestine. From dietary changes to medication options, we will cover it all so you can find relief and regain control of your life. So sit back and read on to discover the best ways to manage and treat diverticulitis. Diverticulitis is a common condition that occurs when small, bulging pouches in the lining of the digestive system become inflamed or infected. While it can cause discomfort and complications, there are various types of diverticulitis and treatment options available to manage the condition effectively.

Types of Diverticulitis
-
Uncomplicated Diverticulitis: This is the most common type of diverticulitis and is characterized by mild symptoms such as abdominal pain, bloating, and changes in bowel movements. The pouches, known as diverticula, become inflamed but do not cause any serious complications.
-
Complicated Diverticulitis: In rare cases, diverticulitis can progress to become more severe and lead to complications such as abscesses, fistulas, perforations, obstructions, or even peritonitis. Complicated diverticulitis requires immediate medical attention and can result in emergency surgery.
Diagnostic Procedures
To accurately diagnose diverticulitis, healthcare professionals employ a variety of diagnostic procedures, including:
-
Physical Examination: During a physical examination, your doctor will assess your abdomen for tenderness, bloating, or any signs of infection. They may also check for a fever or increased heart rate, which can indicate infection.
-
Blood Tests: Blood tests are conducted to check for elevated white blood cell count, which could suggest an infection. Additionally, blood tests can help determine kidney and liver function, as well as assess your overall health status.
-
Imaging Tests: Imaging tests, such as a computed tomography (CT) scan, can provide detailed images of your intestines to identify any inflamed or infected diverticula. These scans are crucial in determining the severity and location of diverticulitis.
-
Colonoscopy: A colonoscopy may be recommended to rule out other conditions that mimic diverticulitis, such as colorectal cancer. During this procedure, a flexible tube with a camera is inserted into the rectum and large intestine to visualize the colon’s inner lining.

Conservative Treatments for Diverticulitis
For patients with uncomplicated diverticulitis or mild symptoms, conservative treatments may be sufficient to alleviate discomfort and promote healing. These treatments can include:
-
Antibiotics: When diverticulitis is accompanied by infection, antibiotics are often prescribed to combat the bacteria causing the inflammation. Depending on the severity of the infection, oral or intravenous antibiotics may be administered.
-
Pain Medication: Non-prescription pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage mild to moderate pain associated with diverticulitis. Prescription pain medication may be necessary for more severe cases.
-
Liquid Diet: In order to provide the intestine with an opportunity to rest and heal, a temporary shift to a liquid diet may be recommended. Clear liquids like broth, gelatin, and clear fruit juices are easily digested and put less strain on the intestines.
-
Rest and Lifestyle Changes: Getting plenty of rest is essential for allowing the body to recover from diverticulitis. Additionally, making long-term lifestyle changes such as increasing fiber intake, staying hydrated, and exercising regularly can help prevent future flare-ups.
Surgical Treatments for Diverticulitis
In cases of complicated diverticulitis or when conservative treatments fail to provide relief, surgical intervention may be necessary. The two main types of surgical treatments are:
-
Emergency Surgery: Emergency surgery is reserved for patients with severe complications such as abscesses, perforations, or peritonitis. The goal of emergency surgery is to remove the affected portion of the intestine and address any other complications.
-
Elective Surgery: Elective surgery is considered for patients who experience recurrent episodes of diverticulitis despite standard medical management or for those at a high risk of developing complications. It involves removing the affected portion of the colon to prevent future flare-ups.
Management of Acute Diverticulitis
When diverticulitis flares up, prompt management is essential to avoid potential complications. Acute diverticulitis can be managed through the following methods:
-
Clear Liquid Diet: In the initial stages of acute diverticulitis, a clear liquid diet is often recommended. This primarily includes fluids that are easy to digest, such as broth, tea, clear fruit juices, and gelatin. The goal is to give the intestines a chance to rest and recover.
-
Antibiotics: If the diverticulitis is accompanied by infection, antibiotics are prescribed to combat the bacterial infection and reduce inflammation. The specific antibiotic will depend on the severity and location of the infection.
-
Pain Medication: Pain medication, both over-the-counter and prescription, can help alleviate the discomfort associated with acute diverticulitis. It is important to follow the prescribed dosage and consult with a healthcare professional as necessary.
-
Hospitalization: In severe cases, hospitalization may be required to closely monitor the patient’s condition, administer intravenous antibiotics, manage pain, and ensure proper hydration. Hospitalization allows doctors to address any potential complications promptly.
Long-term Management and Prevention
To prevent future episodes of diverticulitis and promote overall digestive health, the following long-term management strategies are recommended:
-
High-Fiber Diet: Consuming a diet high in fiber can help regulate bowel movements and prevent constipation, one of the risk factors for diverticulitis. Incorporating foods such as fruits, vegetables, whole grains, and legumes ensures an adequate fiber intake.
-
Lifestyle Changes: Making lifestyle changes, such as quitting smoking and limiting alcohol consumption, can help reduce the risk of diverticulitis. Smoking and excessive alcohol intake are associated with an increased risk of developing the condition.
-
Regular Exercise: Engaging in regular physical activity, such as brisk walking or cycling, helps promote healthy digestion and prevent constipation. Exercise also contributes to overall well-being and can aid in weight management.

Complications and Their Treatments
Diverticulitis can lead to various complications, each requiring appropriate treatment:
-
Abscess: In some cases, diverticulitis can lead to the formation of an abscess, which is a pocket of infected fluid. Treatment often involves draining the abscess through a procedure called percutaneous drainage, along with the use of antibiotics.
-
Fistula: A fistula occurs when an abnormal connection forms between the colon and another organ or the skin. Surgical intervention is typically required to close the fistula and prevent further complications.
-
Perforation: If a diverticulum ruptures and causes a perforation, emergency surgery is necessary to repair the perforation and remove the affected part of the colon. Intravenous antibiotics are administered to prevent infection.
-
Obstruction: A severe case of diverticulitis can lead to a blockage or obstruction of the intestine. To relieve the obstruction, surgery may be required to remove the affected portion of the colon or to create a temporary colostomy.
-
Peritonitis: Peritonitis occurs when the infection from diverticulitis spreads throughout the abdominal cavity. Immediate surgical intervention is required to treat the infection and remove the infected tissues.
Nutritional Considerations
Maintaining a balanced diet is crucial for managing diverticulitis and supporting overall health:
-
Balanced Diet: In addition to consuming a high-fiber diet, it is important to maintain a well-balanced diet that includes all necessary nutrients. A variety of fruits, vegetables, lean proteins, whole grains, and dairy products should be incorporated into daily meals.
-
Supplements: In some cases, individuals with diverticulitis may benefit from the supplementation of certain nutrients. These supplements can include fiber supplements or probiotics to support healthy digestion.

Alternative and Complementary Treatments
While traditional medical treatments are typically the primary approach for diverticulitis, some alternative and complementary treatments are thought to provide additional relief:
-
Probiotics: Probiotics are beneficial bacteria that can help restore the natural balance of gut flora. Some studies suggest that specific strains of probiotics may reduce symptoms and prevent recurrent episodes of diverticulitis.
-
Herbal Remedies: Certain herbal remedies, such as aloe vera and chamomile, are believed to have anti-inflammatory properties that may help alleviate symptoms of diverticulitis. However, it is essential to consult with a healthcare professional before using herbal remedies.
-
Acupuncture: Acupuncture, an ancient Chinese practice, involves inserting thin needles into specific points on the body to promote healing and alleviate pain. It is believed that acupuncture may help reduce inflammation and provide pain relief in cases of diverticulitis.
Psychological Support for Diverticulitis
Dealing with a chronic condition like diverticulitis can take a toll on one’s mental health. Seeking psychological support can be beneficial for coping with the challenges associated with the condition:
-
Counseling: Counseling or therapy sessions can provide individuals with a safe space to discuss their emotions, fears, and frustrations related to diverticulitis. A mental health professional can offer guidance and support to navigate the emotional aspects of living with the condition.
-
Support Groups: Joining a support group for individuals with diverticulitis allows you to connect with others who understand your experiences. Sharing experiences, strategies, and coping mechanisms in a supportive group setting can help reduce feelings of isolation.
In conclusion, understanding the different types of diverticulitis, diagnostic procedures, treatment options, and long-term management recommendations can empower individuals to effectively manage the condition. By working closely with healthcare professionals, making lifestyle changes, and seeking appropriate treatments, individuals diagnosed with diverticulitis can experience relief from symptoms and reduce the risk of complications. Remember, early diagnosis and timely intervention are key to preventing further complications and promoting overall well-being.