You’re about to embark on a fascinating journey delving into the connection between gluten and a skin condition called Dermatitis Herpetiformis. Dermatitis Herpetiformis is a chronic, itchy rash marked by small blisters that can appear on various parts of the body. As you read on, you’ll explore how gluten, a protein found in certain grains, may trigger this autoimmune disorder, and uncover the potential implications for individuals with gluten sensitivity or Celiac disease. So, grab a cup of tea and get ready to uncover the mysteries behind this intriguing link.
Overview of Dermatitis Herpetiformis
Dermatitis Herpetiformis is a chronic skin condition characterized by intensely itchy blisters, bumps, or rash. It is a rare autoimmune disorder that occurs as a result of sensitivity to gluten, a protein found in wheat and other grains. The condition is often associated with celiac disease, another autoimmune disorder triggered by the consumption of gluten. Dermatitis Herpetiformis typically affects the skin, but it is connected to the body’s immune response to gluten.
Definition of Dermatitis Herpetiformis
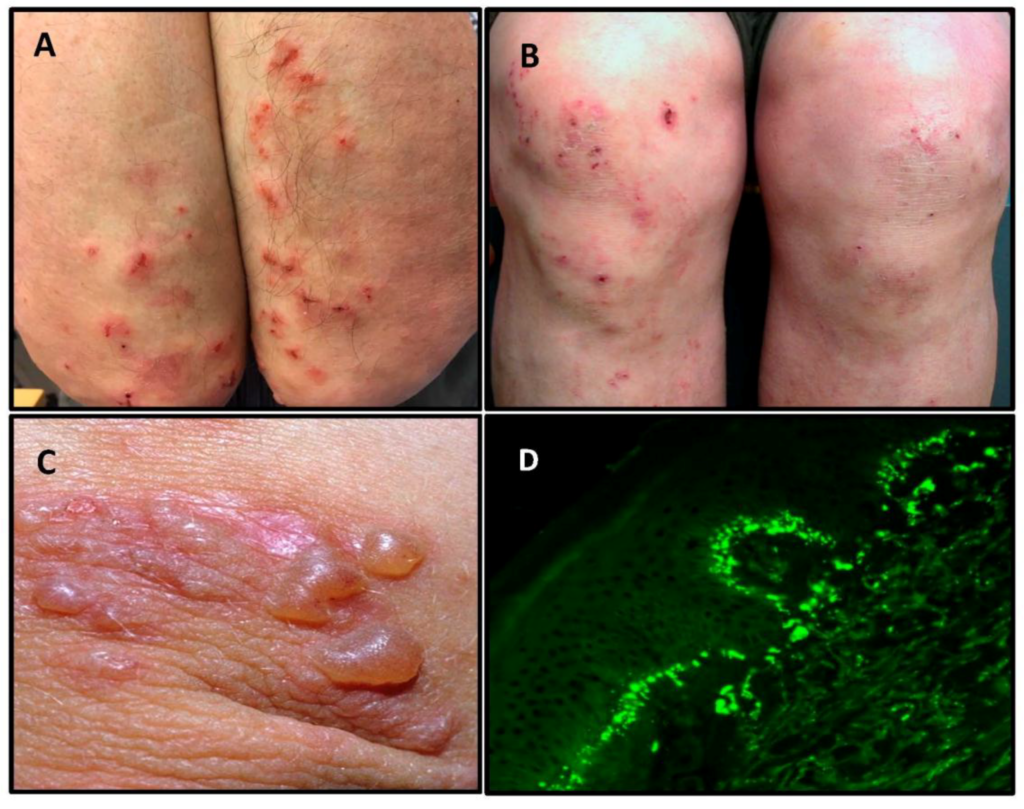
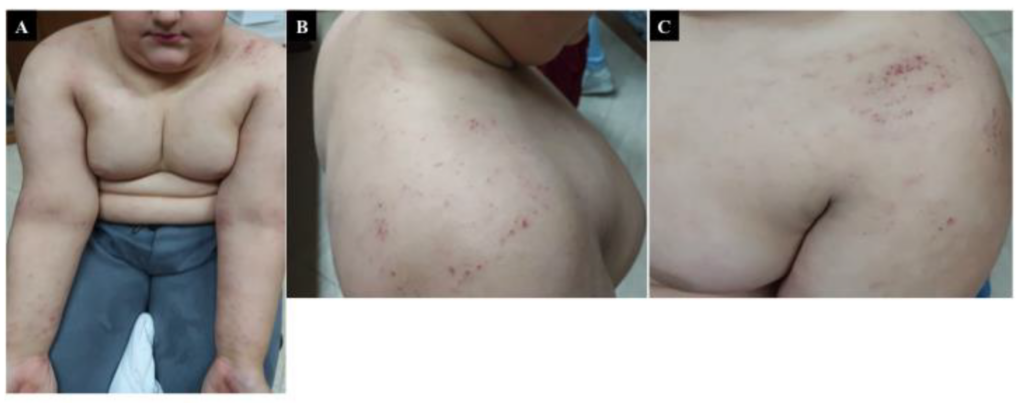
Dermatitis Herpetiformis, also known as Duhring’s disease, is a blistering skin condition that presents as a chronic rash. The name “dermatitis herpetiformis” was coined due to the initial belief that the condition was related to herpes, but this is not the case. The condition typically presents as small, red bumps or blisters that are extremely itchy and can cause significant discomfort. These lesions often appear symmetrically on the elbows, knees, buttocks, and scalp.
Symptoms of Dermatitis Herpetiformis
The primary symptom of dermatitis herpetiformis is intense itching. The itching is often described as a stinging or burning sensation and can become extremely bothersome. Along with the itching, small red bumps or blisters may appear on the skin. These lesions are typically grouped together and can be very uncomfortable. Scratching the affected areas can lead to the formation of crusts and scabs, which can further irritate the skin. In some cases, the skin may become discolored or develop areas of hyperpigmentation.
Prevalence and Incidence of Dermatitis Herpetiformis
Dermatitis Herpetiformis is a relatively rare condition, with an estimated prevalence of 10 to 39 cases per 100,000 individuals. It is more commonly diagnosed in adults, with a peak onset occurring between the ages of 30 and 40, although it can affect individuals of any age. The condition is more prevalent in individuals of Northern European descent, particularly those of Scandinavian or Celtic ancestry. Dermatitis Herpetiformis is believed to affect males slightly more often than females, but the difference is not significant.

Causes of Dermatitis Herpetiformis
Role of Gluten in Dermatitis Herpetiformis
The primary cause of dermatitis herpetiformis is the consumption of gluten. Gluten is a protein found in wheat, rye, and barley, and it triggers an immune response in individuals with dermatitis herpetiformis. When gluten is ingested, the body produces antibodies that attack the skin, leading to the development of the characteristic rash and blisters. It is important to note that not all individuals with dermatitis herpetiformis have celiac disease, although a strong association between the two conditions exists.
Genetic Factors in Dermatitis Herpetiformis
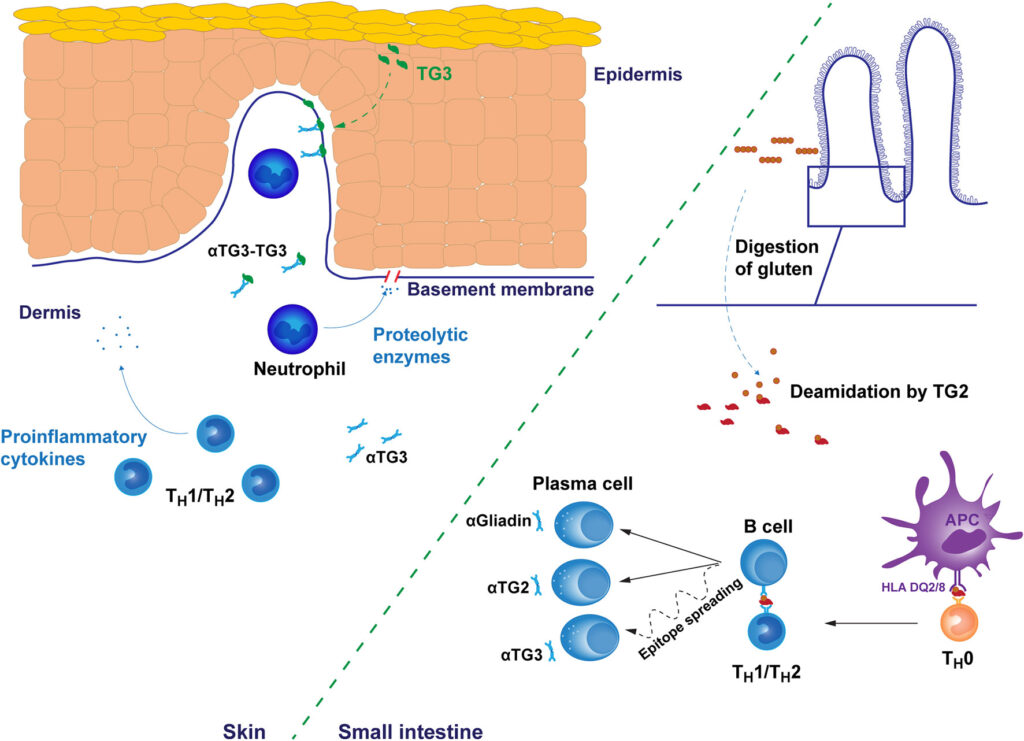
There is evidence to suggest that genetic factors play a role in the development of dermatitis herpetiformis. Certain variations of specific genes, such as HLA-DQ2 and HLA-DQ8, have been associated with an increased risk of both dermatitis herpetiformis and celiac disease. These genes are involved in the immune response and may influence the body’s reaction to gluten. However, it is important to note that not all individuals with these genetic variations will develop dermatitis herpetiformis, indicating that there are likely other factors at play.
Pathophysiology of Dermatitis Herpetiformis
Autoimmune Basis of Dermatitis Herpetiformis
Dermatitis Herpetiformis is an autoimmune disorder, meaning that the immune system mistakenly attacks healthy tissue. In the case of dermatitis herpetiformis, the immune system mistakenly targets the skin when exposed to gluten. This immune response leads to the development of inflammation and the characteristic rash and blisters. The exact mechanism behind this autoimmune response is not fully understood, but it is believed to involve a complex interplay between genetic predisposition and environmental factors such as gluten consumption.
Immune Response to Gluten in Dermatitis Herpetiformis
In individuals with dermatitis herpetiformis, gluten triggers an immune response in the small intestine. This immune response leads to the production of antibodies, specifically immunoglobulin A (IgA) antibodies. These IgA antibodies then migrate to the skin, where they bind to proteins called transglutaminases. The interaction between the antibodies and transglutaminases causes inflammation in the skin, resulting in the characteristic rash and blisters. It is important to note that the immune response in dermatitis herpetiformis is specific to the skin, while in celiac disease, it primarily affects the intestines.

Diagnosis of Dermatitis Herpetiformis
Clinical Examination and Symptoms
Diagnosing dermatitis herpetiformis often begins with a thorough clinical examination and evaluation of symptoms. A dermatologist will carefully assess the characteristic rash and blisters, paying close attention to the location and appearance of the lesions. The intensely itchy nature of the rash is often a key indicator of dermatitis herpetiformis, particularly when it is accompanied by a history of gluten sensitivity or celiac disease. However, a clinical examination alone is not enough to confirm the diagnosis.
Skin Biopsy and Histopathology
To confirm the diagnosis of dermatitis herpetiformis, a skin biopsy is typically performed. During a biopsy, a small sample of skin is taken from an active lesion and examined under a microscope. The histopathology of dermatitis herpetiformis shows specific changes, including an accumulation of neutrophils (a type of white blood cell) beneath the skin’s surface. These neutrophils form small clusters called microabscesses. The presence of these microabscesses, along with other histopathological findings, is highly characteristic of dermatitis herpetiformis.
Blood Tests for Dermatitis Herpetiformis
In addition to a skin biopsy, blood tests can aid in the diagnosis of dermatitis herpetiformis. The presence of specific antibodies, such as IgA antibodies and transglutaminase antibodies, can help support the diagnosis. These antibodies are often elevated in individuals with dermatitis herpetiformis, particularly when there is concomitant gluten sensitivity or celiac disease. Blood tests can also be helpful in ruling out other skin conditions that may present with similar symptoms.
Treatment of Dermatitis Herpetiformis
Gluten-Free Diet as the Primary Treatment
The most effective treatment for dermatitis herpetiformis is a strict lifelong adherence to a gluten-free diet. By eliminating all sources of gluten from the diet, individuals with dermatitis herpetiformis can effectively manage the condition and prevent symptom flare-ups. This requires careful reading of food labels and avoiding not only obvious sources of gluten but also hidden sources, such as certain processed foods, sauces, and seasonings. It is also important to avoid cross-contamination, as even small amounts of gluten can trigger a reaction.
Medications for Dermatitis Herpetiformis
In some cases, medications may be prescribed to help manage the symptoms of dermatitis herpetiformis. Dapsone, an oral medication, is commonly used to reduce itching and inflammation. It works by suppressing the immune response and reducing the formation of antibodies. However, dapsone may have potential side effects, such as anemia and liver toxicity, so regular monitoring and close supervision by a healthcare professional are necessary. Other medications, such as sulfapyridine or certain antibiotics, may be used as alternatives or in combination with dapsone.
Management of Itching and Skin Lesions
In addition to a gluten-free diet and medications, there are several measures individuals with dermatitis herpetiformis can take to manage itching and promote healing of the skin. Applying topical creams or ointments can help soothe the skin and alleviate discomfort. Cool compresses or baths can also provide temporary relief from itching. It is important to avoid scratching or picking at the lesions, as this can lead to further irritation and potential infection. Keeping the skin clean and dry, wearing loose-fitting clothing, and avoiding irritating substances can also help manage symptoms.
Relationship Between Dermatitis Herpetiformis and Celiac Disease
Prevalence of Dermatitis Herpetiformis in Celiac Disease
Dermatitis herpetiformis is strongly associated with celiac disease, with up to 25% of individuals with celiac disease also developing dermatitis herpetiformis. The two conditions share a common trigger, gluten, and are thought to be related autoimmune disorders. However, not all individuals with dermatitis herpetiformis have celiac disease, and not all individuals with celiac disease have dermatitis herpetiformis. It is important for individuals with either condition to be aware of the potential comorbidity and seek appropriate medical care.
Similarities and Differences
Dermatitis herpetiformis and celiac disease are both autoimmune disorders with a shared immune response to gluten. However, there are distinct differences between the two conditions. While dermatitis herpetiformis primarily affects the skin, celiac disease primarily affects the small intestine. The symptoms of celiac disease are more varied and can include gastrointestinal distress, malabsorption, and nutrient deficiencies. In contrast, the symptoms of dermatitis herpetiformis are predominantly skin-related, with intense itching and the development of skin lesions. Despite these differences, the management of both conditions involves strict adherence to a gluten-free diet.
Potential Complications of Dermatitis Herpetiformis
Intestinal Damage and Nutritional Deficiencies
Untreated or poorly managed dermatitis herpetiformis can lead to long-term complications, particularly in individuals with undiagnosed celiac disease. The immune response triggered by gluten can damage the lining of the small intestine, leading to malabsorption of nutrients. This malabsorption can result in various nutritional deficiencies, including iron deficiency anemia, vitamin deficiencies, and calcium malabsorption. It is crucial for individuals with dermatitis herpetiformis to be screened for celiac disease and receive appropriate treatment to prevent these complications.
Risk of Lymphoma and Other Cancers
Another potential complication of dermatitis herpetiformis is an increased risk of developing certain types of cancer, particularly lymphoma. Studies have shown that individuals with dermatitis herpetiformis have a higher prevalence of lymphoma compared to the general population. It is important to note that the overall risk of developing lymphoma is still relatively low, but individuals with dermatitis herpetiformis should be aware of this association. Regular monitoring by a healthcare professional is essential to detect any early signs of lymphoma or other cancers.
Living with Dermatitis Herpetiformis
Adhering to a Strict Gluten-Free Diet
Living with dermatitis herpetiformis requires a lifelong commitment to a strict gluten-free diet. This involves actively avoiding foods and products that contain gluten, which can be challenging, particularly when eating out or traveling. However, with careful planning and education, it is possible to lead a healthy and fulfilling life while managing the condition. It is important to stay informed about gluten-free food options and to seek support from healthcare professionals, dietitians, and support groups that specialize in gluten-related disorders.
Importance of Regular Follow-up
Regular follow-up appointments with a dermatologist or healthcare professional are crucial for individuals with dermatitis herpetiformis. These appointments allow for the monitoring of the skin condition and the assessment of treatment effectiveness. Additionally, regular check-ups can help identify any potential complications or changes in symptoms that may require further evaluation. Close communication with healthcare professionals ensures that any necessary adjustments to treatment or management strategies can be made promptly.
Support Groups and Resources
Living with dermatitis herpetiformis can be challenging, both physically and emotionally. Seeking support from others who are going through a similar experience can provide comfort, knowledge, and encouragement. Support groups, both in-person and online, can offer a safe space to share experiences, ask questions, and access valuable resources. Additionally, there are numerous educational materials, websites, and books available that provide information on living with dermatitis herpetiformis and managing a gluten-free lifestyle.
Future Research and Outlook
Advancements in Understanding the Disease
As research into autoimmune disorders expands, there is an increasing focus on dermatitis herpetiformis and its connection to celiac disease. Scientists continue to investigate the underlying mechanisms of the condition, including the role of specific genes and the immune response to gluten. Advancements in understanding the disease will contribute to improved diagnostic tools, more targeted treatments, and a better understanding of the long-term outcomes for individuals with dermatitis herpetiformis.
Potential Therapeutic Targets
Exploring potential therapeutic targets for dermatitis herpetiformis is a growing area of interest. Scientists are investigating medications and interventions that specifically target the immune response and minimize inflammation. These advancements may offer alternative treatment options for individuals who may not respond well to or tolerate existing therapies. Additionally, research is ongoing to develop medications that could potentially block the immune response triggered by gluten, providing a more direct way to manage the condition.
Improving Quality of Life for Patients
With increasing awareness and understanding of dermatitis herpetiformis, there is a growing emphasis on improving the quality of life for individuals living with the condition. This includes efforts to support individuals in adhering to a gluten-free lifestyle, providing access to resources and support groups, and promoting mental well-being. As research progresses, new strategies and interventions will continue to emerge, further enhancing the overall management and quality of life for patients with dermatitis herpetiformis.
Conclusion
Dermatitis Herpetiformis is a chronic autoimmune skin condition characterized by intensely itchy blisters, bumps, or rash. It is closely related to gluten sensitivity and celiac disease, with gluten triggering an immune response that leads to inflammation in the skin. While a strict gluten-free diet is the primary treatment for dermatitis herpetiformis, medications and other management strategies can also be utilized to alleviate symptoms. Regular follow-up with healthcare professionals and participation in support groups can help individuals effectively manage the condition and improve their quality of life. Ongoing research is contributing to a better understanding of dermatitis herpetiformis, which will lead to advancements in diagnosis, treatment, and the overall care of individuals with this condition.