Are you familiar with the itching, redness, and blisters that poison ivy can cause? If so, you’ll want to pay attention to these important nursing considerations for treating patients affected by this troublesome plant. From assessing the severity of the rash to providing relief through medication and education, nurses play a crucial role in managing the symptoms and preventing further complications. In this article, we’ll explore the key nursing considerations and best practices for dealing with poison ivy, ensuring that you have the knowledge and skills to effectively assist those affected by this irritating rash.
Patient Assessment
Identification of Poison Ivy Exposure
When assessing a patient for potential poison ivy exposure, it is crucial to gather information about their recent activities, such as hiking, gardening, or outdoor recreational activities. Ask if they have come into contact with any plants or foliage, especially poison ivy. Promptly identify and document any areas of skin that appear to have been in contact with poison ivy. These areas may show signs of redness, itching, and the development of blisters. Carefully examining the patient’s clothing and any tools or equipment they were using can also provide additional clues.
Assessment of symptoms and severity
Assess the patient’s symptoms related to poison ivy exposure, such as redness, itching, swelling, and the presence of blisters or rash. Observe the affected areas closely for signs of infection, such as increased redness, warmth, and pus. Evaluate the severity of the symptoms by considering the size and location of the rash, the intensity of the itching, and the overall impact on the patient’s daily activities. Assess any associated symptoms, including fever, general malaise, and joint pain, which could indicate a more severe reaction.
Evaluation of patient’s medical history
During the patient assessment, gather information about the patient’s medical history, including any known allergies or previous reactions to poison ivy. Inquire about existing medical conditions, such as asthma, because patients with certain conditions may be at higher risk for complications. Additionally, ask the patient about any current medications they are taking, as some medications may interact with treatment options for poison ivy. Understanding the patient’s medical history will help inform appropriate treatment and prevention strategies.
Symptom Management
Topical Treatment Options
When it comes to managing symptoms of poison ivy exposure, topical treatments play a crucial role. Recommend the application of calamine lotion or over-the-counter hydrocortisone creams to relieve itching and reduce inflammation. Emphasize the importance of gently washing the affected areas with mild soap and water before applying any topical treatments. Educate patients on proper technique and remind them to avoid scratching or picking at the affected areas to prevent further irritation and potential infection.
Oral Medications for Symptom Relief
In cases of severe itching or discomfort, oral medications may be necessary to provide relief. Common options include antihistamines, such as diphenhydramine, to help alleviate itching and promote sleep. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, can also be recommended to reduce inflammation and relieve pain. However, caution should be exercised when recommending or administering medications, particularly for vulnerable populations, and it is crucial to consider any potential interactions with the patient’s existing medications.
Non-pharmacological Interventions
Alongside topical and oral treatments, non-pharmacological interventions can help manage symptoms and provide relief. Encourage patients to apply cold compresses or take cool showers to soothe inflamed skin and reduce itching. Stress the importance of avoiding hot showers or baths, as the heat can worsen itching and potentially cause further skin irritation. Furthermore, instruct patients to wear loose-fitting, cotton clothing to minimize skin irritation and allow for better air circulation. Finally, advise patients to avoid activities that may cause excessive sweating, as sweat can exacerbate symptoms.

Prevention Strategies
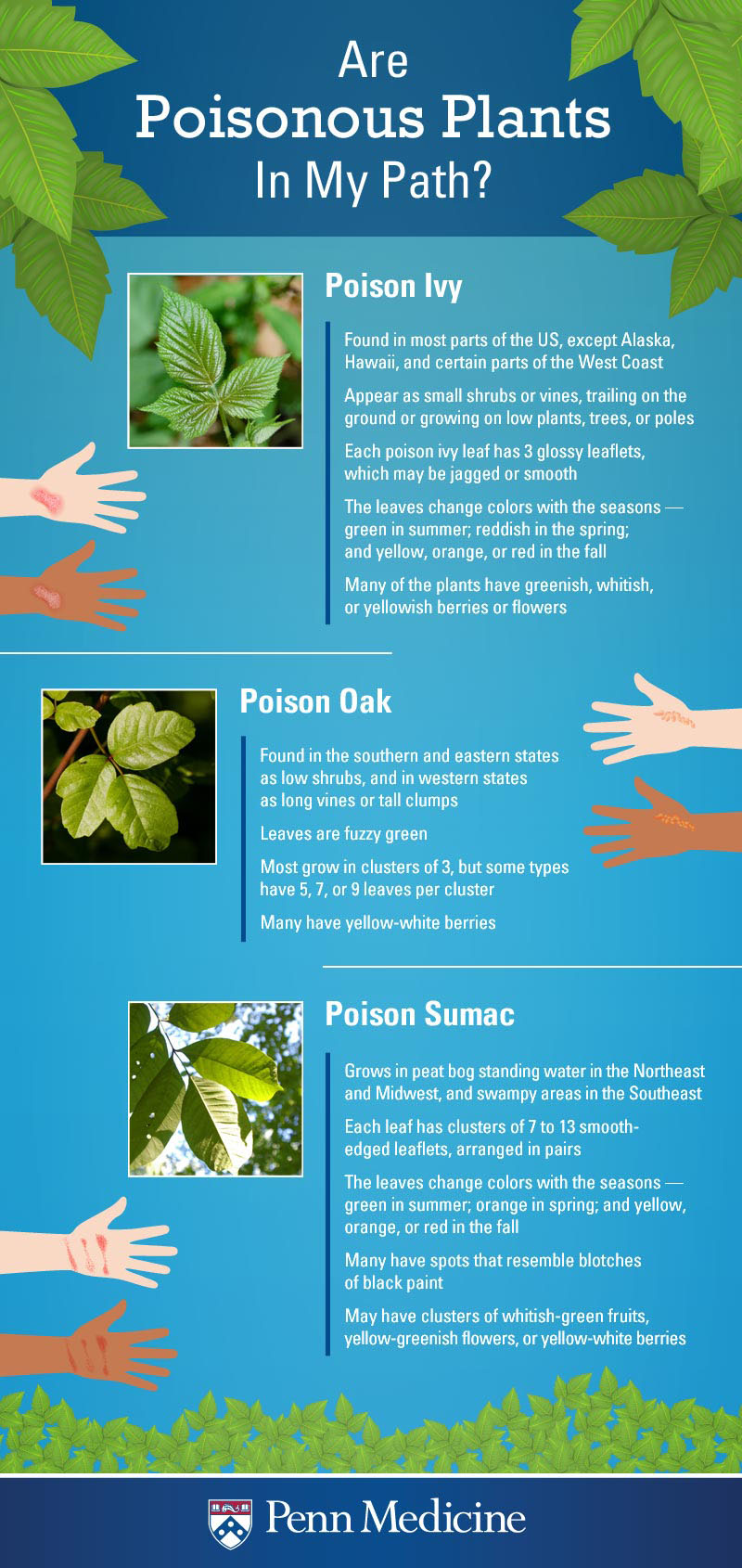
Education on Identifying Poison Ivy Plants
A vital aspect of preventing poison ivy exposure is educating patients on how to identify the plant accurately. Teach patients that poison ivy plants typically have three leaflets, resembling the shape of a mitten. The leaves may be shiny or dull, and their edges can be smooth or toothed. Emphasize the importance of avoiding any contact with plants that match these characteristics. Show pictures or provide visual aids to help patients recognize poison ivy in different settings, such as hiking trails or their own backyard.
Recommendations for Protective Clothing
To prevent direct contact with poison ivy, advise patients to wear long sleeves, long pants, and closed-toe shoes when engaging in outdoor activities. Suggest the use of gloves when gardening or handling plants. For added protection, recommend patients to tuck their pants into their socks or boots to further minimize the risk of contact with poison ivy. Proper clothing can act as a barrier between the skin and the plant, reducing the chances of exposure and subsequent symptoms.
Use of Barrier Creams and Washes
Barrier creams and washes can provide an extra layer of protection against poison ivy oils, which can cause a rash upon contact with the skin. Recommend the use of over-the-counter barrier creams containing ingredients such as bentoquatam, which create a protective barrier on the skin. Instruct patients to apply the cream in a thin layer before venturing outdoors. Additionally, advise patients to use specialized washes, such as those containing non-ionic surfactants, to remove any oils that may have come into contact with their skin.
Infection Prevention
Proper Wound Care
In cases where the patient’s skin has become blistered or broken as a result of poison ivy exposure, proper wound care is crucial to prevent infection. Instruct patients to clean the affected areas gently with mild soap and water. Advise them to avoid applying harsh chemicals or irritants to the open skin as it may worsen the symptoms and delay healing. Emphasize the importance of allowing the blisters to heal naturally and avoid popping them to prevent further damage and potential infection.
Techniques for Preventing Secondary Infections
Secondary infections are a concern when dealing with open wounds caused by poison ivy. Educate patients on proper techniques for preventing secondary infections, such as keeping the affected areas clean and dry. Instruct them to avoid scratching or picking at the blisters to minimize the risk of introducing bacteria. Encourage patients not to share towels or clothing with others to prevent the spread of potential pathogens. If signs of infection, such as increased redness, swelling, or pus, occur, advise patients to seek medical attention promptly.
Importance of Hand Hygiene
Stress the significance of proper hand hygiene to prevent the spread of poison ivy oils to other parts of the body and potential contamination of objects or surfaces. Emphasize the importance of washing hands thoroughly with soap and water, especially after coming into contact with poison ivy plants or any items that may have been exposed to the oils. Encourage patients to carry hand sanitizer with them for situations where handwashing is not readily available. By practicing good hand hygiene, patients can minimize the risk of further exposure and subsequent symptoms.

Special Considerations for Vulnerable Populations
Pediatric Patients
When dealing with pediatric patients, it is essential to exercise additional caution and tailored care. Children may have a harder time avoiding poison ivy or recognizing the plant’s distinguishing characteristics, so education should be provided in an age-appropriate manner. Avoid using scare tactics but emphasize the importance of listening to caregivers and following prevention methods. When choosing treatment options, consult a pediatrician to ensure the safety and effectiveness of specific medications for younger patients.
Pregnant or Nursing Women
Pregnant or nursing women should be advised to take extra precautions to protect themselves from poison ivy exposure. Educate them about the potential risks to both themselves and their unborn or nursing babies. Emphasize the importance of using protective clothing, barrier creams, and frequent handwashing. When considering treatment options, consult with their obstetrician or primary healthcare provider to ensure the safety and appropriateness of recommended medications during pregnancy or lactation.
Elderly Individuals
Elderly individuals may be more susceptible to severe reactions from poison ivy exposure due to weakened immune systems. Assess their overall health status and closely monitor for potential complications. Educate them on prevention strategies and provide clear instructions on proper wound care and symptom management. Additionally, ensure they have a good support system in place and consider involving family members or caregivers in their care to assist with adherence to prevention methods and treatment regimens.
Complications and Emergency Situations
Identifying severe allergic reactions
Be vigilant in assessing patients for signs of severe allergic reactions, also known as anaphylaxis, as these can be life-threatening. Symptoms may include difficulty breathing, swelling of the face, lips, tongue, or throat, rapid heartbeat, dizziness, or loss of consciousness. If a patient exhibits any of these symptoms, immediately initiate emergency medical assistance and ensure a swift transfer to a healthcare facility for further evaluation and treatment.
Recognition of secondary infections
Secondary infections may occur as a result of scratching or breaking the skin due to intense itching caused by poison ivy exposure. Watch for signs of infection, such as increased redness, warmth, swelling, pain, or the presence of pus. Advise patients to seek medical attention promptly if any of these symptoms occur, as they may require antibiotic treatment to prevent further complications. Proper education regarding wound care and infection prevention techniques can help reduce the risk of secondary infections.
Management of anaphylactic shock
If a patient experiences anaphylactic shock due to severe allergic reactions, prompt and appropriate management is crucial. Ensure the patient’s airway remains open and unobstructed, assist with any necessary breathing or administer CPR if required. If available, administer epinephrine immediately according to established protocols and seek emergency medical help without delay. Continuous monitoring and supportive care should be provided until the patient is stabilized and transferred to a medical facility for further management and evaluation.

Patient Education
Teaching patients about poison ivy
Educating patients about poison ivy is essential for their understanding of how to prevent exposure and manage any symptoms effectively. Explain the appearance and characteristics of poison ivy plants, emphasizing the importance of avoiding direct contact. Describe the common symptoms of poison ivy exposure to help patients recognize and start appropriate management promptly. Answer any questions and provide informational pamphlets or resources to reinforce the information given and support their learning.
Guidance on avoiding future exposure
Patients should be provided with comprehensive guidance on how to avoid future exposure to poison ivy. Reinforce the importance of recognizing and avoiding contact with the plant, especially in outdoor environments. Encourage patients to routinely inspect their surroundings and promptly remove any poison ivy plants they may encounter on their property. Furthermore, advise patients to consider alternative activities or locations that are free of poison ivy, reducing the risk of exposure altogether.
Recognition of early symptoms
Teach patients how to recognize the early symptoms of poison ivy exposure, such as redness, itching, and the formation of blisters or rash. Instruct them to monitor any areas of skin that have come into contact with poison ivy closely. Prompt recognition of these symptoms allows for early intervention and prevents the progression of the condition. Encourage patients to seek medical advice promptly if symptoms persist, worsen, or if signs of infection or severe allergic reactions develop.
Psychosocial Support
Addressing patient anxiety and distress
Poison ivy exposure can cause significant anxiety and distress due to intense itching, discomfort, and possible cosmetic concerns. Offer empathy, actively listen to their concerns, and reinforce that poison ivy reactions are common and treatable. Educate patients on symptom management strategies to alleviate discomfort and provide reassurance regarding the self-limiting nature of the condition. Additionally, encourage patients to express their concerns openly and offer additional resources or counseling services if needed.
Counseling on coping mechanisms
When patients experience the discomfort and frustration associated with poison ivy exposure, it is essential to provide them with coping mechanisms. Encourage patients to engage in activities that can divert their attention from the itching, such as reading, watching movies, or participating in hobbies. Use distraction techniques, such as deep breathing exercises or meditation, to help patients manage their anxiety. Recommend the use of over-the-counter products like anti-itch creams or cold compresses for temporary relief.
Referral for specialized mental health support
In certain cases, patients may require additional mental health support to manage the psychological impact of poison ivy exposure. If patients exhibit signs of severe distress, anxiety disorders, or depression, it is crucial to refer them to specialized mental health professionals for further evaluation and treatment. Collaborate with the patient’s healthcare provider to ensure comprehensive care and address any underlying psychological issues that may arise from the experience.

Collaboration with Other Healthcare Professionals
Communication with physicians
Close collaboration with physicians is essential when managing patients with poison ivy exposure. Provide detailed assessments and updates on the patient’s symptoms, severity, and treatment response to inform the physician’s decision-making process. Seek guidance regarding medication management, particularly in complex cases or when dealing with vulnerable populations. Effective communication ensures continuity of care and promotes patient safety and well-being.
Coordination with dermatologists
In complex or severe cases of poison ivy exposure, consultation with a dermatologist may be warranted. Dermatologists can offer specialized expertise in managing skin conditions and provide advanced treatment options if necessary. Collaborate with the dermatologist to develop a holistic care plan and ensure optimal outcomes for the patient. Regularly communicate updates and progress to maintain continuity of care and facilitate the patient’s recovery.
Consultation with pharmacists
Pharmacists play a crucial role in patient care when it comes to medication management and potential interactions. Consult with pharmacists to ensure appropriate prescribing, dosing, and administration of medications used to manage symptoms or prevent potential complications. Utilize their expertise to identify any potential drug-drug interactions or contraindications, particularly in patients who are taking multiple medications concurrently. Regular communication and collaboration with pharmacists promote patient safety and optimize treatment outcomes.
Follow-up and Continuity of Care
Monitoring patient progress
After initiating treatment and providing education, regularly monitor the patient’s progress and update their medical record accordingly. Assess the improvement of symptoms, evaluate the effectiveness of the prevention strategies implemented, and ensure any potential complications are promptly addressed. Document changes in the patient’s condition, including any adverse reactions or treatment modifications, to ensure continuity of care and accurate patient management.
Scheduling further medical evaluations
In cases where the patient’s symptoms persist or worsen despite initial treatment, it may be necessary to schedule further medical evaluations. Consult the patient’s primary healthcare provider or dermatologist to determine the most appropriate next steps. They may recommend additional tests or refer the patient to a specialist for further evaluation or treatment. Timely follow-up appointments ensure the ongoing assessment of the patient’s condition and the adaptation of treatment strategies if needed.
Documentation and reporting
Accurate and detailed documentation is essential in every step of patient care. Record the patient’s medical history, assessment findings, treatment plans, and patient education provided. Document any changes in symptoms, medication adjustments, and follow-up appointments, ensuring continuity of care between different healthcare providers. Allergy alert bracelets or other relevant documentation should be recommended to alert future healthcare professionals about the patient’s specific reaction to poison ivy.