Hey there! Have you ever wondered about the ins and outs of juvenile diabetes? Well, wonder no further! In this article, we will explore the causes, symptoms, and treatment options for this unique form of diabetes. So, grab a cup of tea and get ready to dive into the world of juvenile diabetes!
Overview of Juvenile Diabetes
Juvenile diabetes, also known as type 1 diabetes, is a chronic condition that occurs when the pancreas produces little or no insulin. Insulin is a hormone that regulates the amount of sugar (glucose) in the blood. Without sufficient insulin, the glucose builds up in the bloodstream, leading to high blood sugar levels. Juvenile diabetes typically develops during childhood or adolescence, hence the name “juvenile” diabetes. It requires lifelong management and can significantly impact the daily life of those affected.
What is Juvenile Diabetes?
Juvenile diabetes, or type 1 diabetes, is an autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. Unlike type 2 diabetes, which is often associated with lifestyle factors like obesity and lack of physical activity, type 1 diabetes is not preventable or curable. Approximately 1.6 million Americans are living with type 1 diabetes, with around 40,000 cases diagnosed each year.
Causes of Juvenile Diabetes
While the exact cause of juvenile diabetes is still unknown, several factors are thought to contribute to its development. These include genetic factors, autoimmune response, and environmental triggers.
Genetic Factors
Genetics play a significant role in the development of juvenile diabetes. Individuals with certain gene variants have an increased risk of developing the condition. However, not all individuals with these genetic markers will develop diabetes, suggesting that other factors are involved.
Autoimmune Response
In individuals with juvenile diabetes, the immune system mistakenly targets and destroys the insulin-producing cells in the pancreas. The exact trigger for this autoimmune response is still unknown, but it is believed to involve a combination of genetic predisposition and environmental factors.
Environmental Factors
Certain environmental factors, such as viral infections or exposure to certain chemicals, may trigger the autoimmune response in individuals who are genetically susceptible. However, more research is needed to fully understand the specific environmental factors involved in the development of juvenile diabetes.
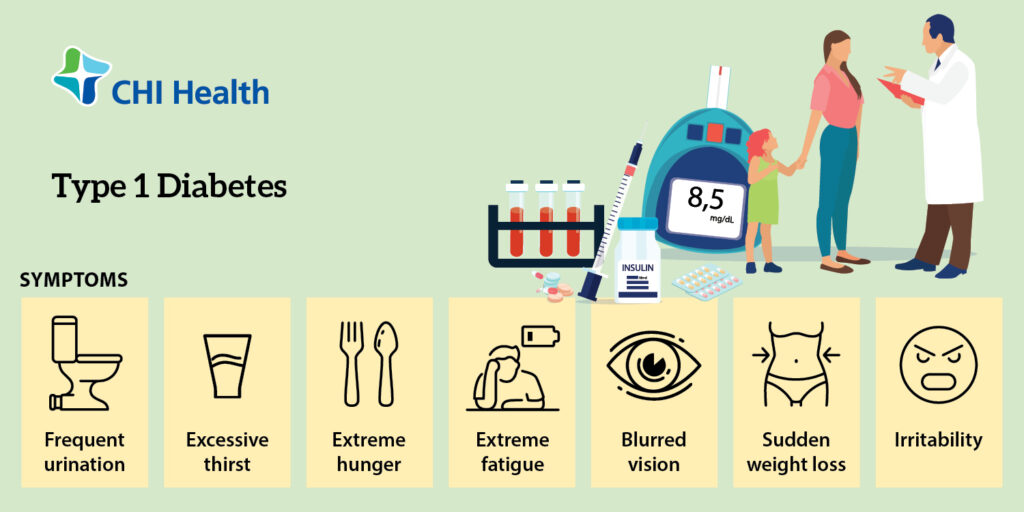
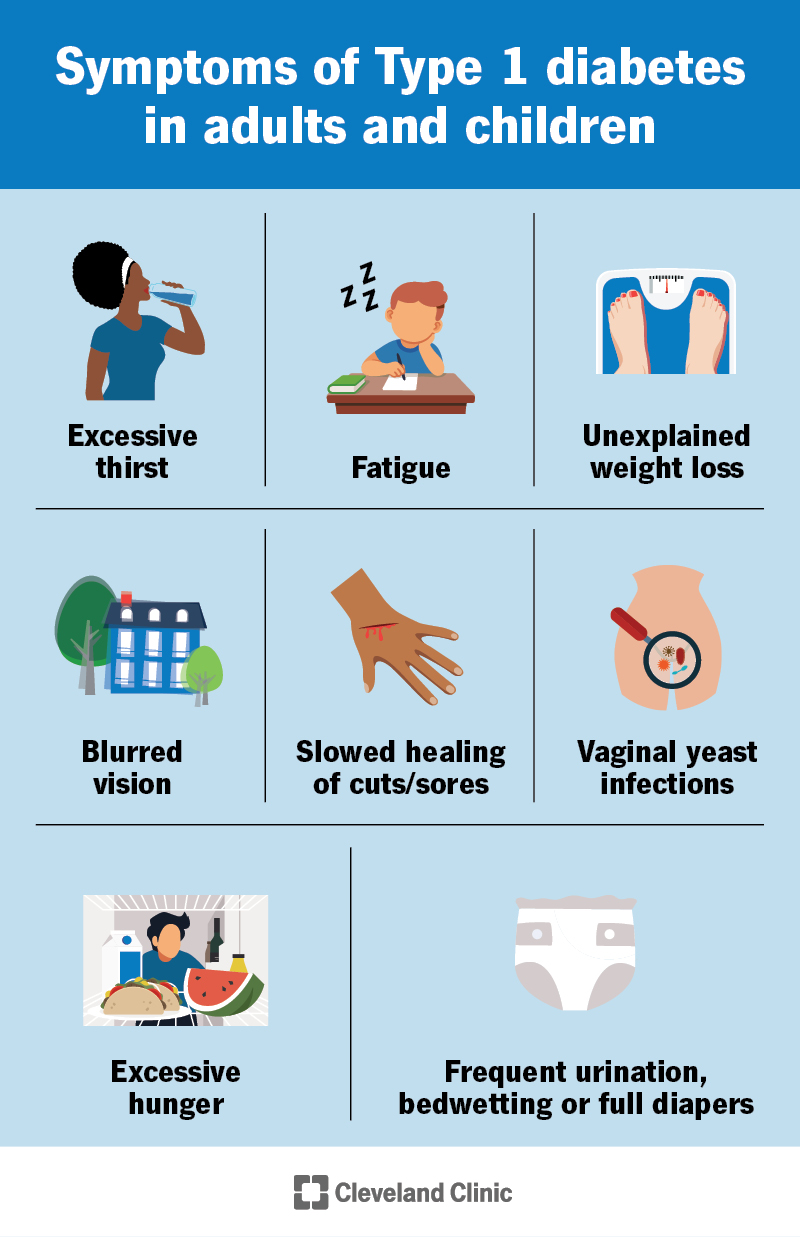
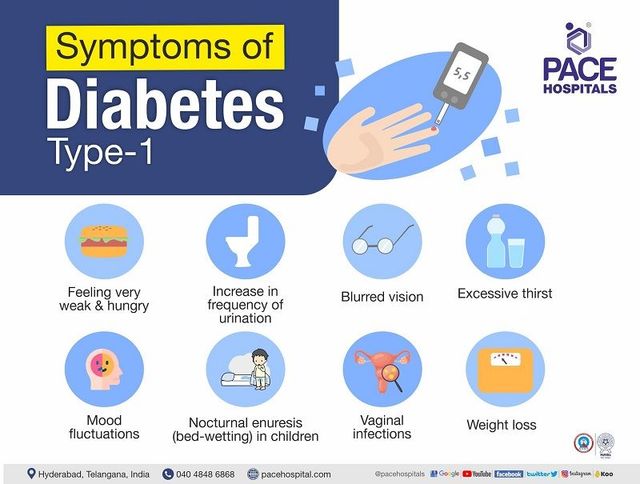
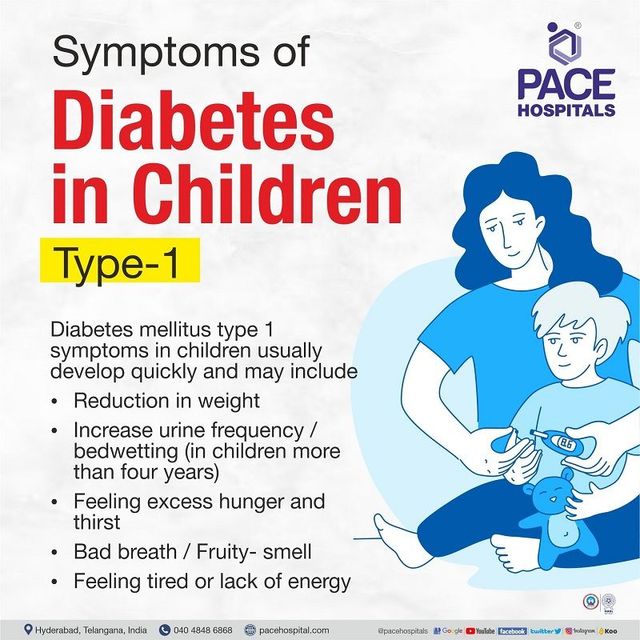
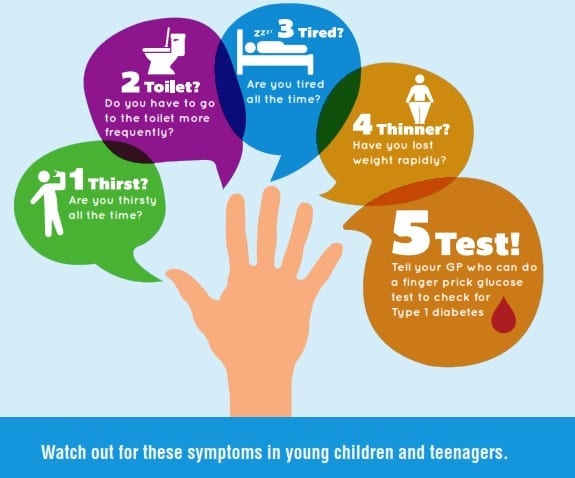
Symptoms of Juvenile Diabetes
Recognizing the symptoms of juvenile diabetes is crucial for early diagnosis and appropriate management. Here are some common symptoms to be aware of:
Increased Thirst and Frequent Urination
One of the early signs of juvenile diabetes is excessive thirst (polydipsia) and frequent urination (polyuria). This is due to the body’s attempt to eliminate excess glucose through urine.
Unexplained Weight Loss
Despite increased hunger and calorie intake, individuals with juvenile diabetes may experience unexplained weight loss. This is because the body is unable to properly utilize glucose for energy and starts breaking down fat and muscle for fuel.
Extreme Hunger
Juvenile diabetes can also cause extreme hunger (polyphagia) as the body tries to compensate for the lack of energy from glucose. Individuals may feel constantly hungry, even after eating regular meals.
Fatigue and Weakness
The lack of glucose being absorbed by the body’s cells for energy can lead to persistent fatigue and weakness, even after adequate rest.
Blurred Vision
High levels of glucose in the bloodstream can affect the shape of the eye lens, resulting in blurred vision. This symptom may be temporary and improve with blood sugar control.
Slow-Healing Sores or Frequent Infections
Elevated blood sugar levels can impair the body’s ability to heal wounds and fight off infections. Individuals with juvenile diabetes may experience slow-healing sores or be more prone to infections, such as urinary tract infections or yeast infections.
Tingling or Numbness in Hands and Feet
Nerve damage, known as diabetic neuropathy, can occur in individuals with poorly controlled juvenile diabetes. This can cause a tingling or numb sensation in the hands and feet.
Irritability and Mood Swings
Fluctuations in blood sugar levels can affect mood and behavior. Individuals with juvenile diabetes may experience irritability, mood swings, and difficulty concentrating.
Diagnosing Juvenile Diabetes
If you or your child is experiencing symptoms of juvenile diabetes, it is important to seek medical attention for an accurate diagnosis. Here are common diagnostic methods:
Blood Tests to Measure Blood Glucose Levels
A blood test, typically a fasting plasma glucose test, is used to measure the level of glucose in the blood. If the results show consistently high blood sugar levels, further tests may be conducted to confirm the diagnosis.
Glycated Hemoglobin (A1C) Test
The A1C test provides an average of blood sugar levels over the past two to three months. It measures the percentage of hemoglobin that is coated with sugar. A higher A1C level indicates poorer blood sugar control and may suggest the presence of diabetes.
Types of Juvenile Diabetes
While type 1 diabetes is the most common form of juvenile diabetes, there are other types to be aware of:
Type 1 Diabetes
Type 1 diabetes is the primary form of juvenile diabetes and occurs when the immune system mistakenly destroys the insulin-producing cells in the pancreas. It requires lifelong insulin therapy for blood sugar management.
Type 2 Diabetes
Although less common in children and adolescents, type 2 diabetes can also develop during these stages. It is often associated with lifestyle factors such as obesity, lack of physical activity, and poor dietary choices. Type 2 diabetes may be managed with a combination of lifestyle changes, oral medications, and insulin therapy.
Other Rare Forms of Juvenile Diabetes
There are several other rare forms of juvenile diabetes, including maturity-onset diabetes of the young (MODY) and neonatal diabetes. These forms have distinct genetic and clinical characteristics, but they are relatively uncommon compared to type 1 and type 2 diabetes.
Treatment Options for Juvenile Diabetes
Effective management of juvenile diabetes involves comprehensive treatment strategies. Here are some common treatment options:
Insulin Therapy
Individuals with juvenile diabetes require insulin therapy to regulate their blood sugar levels. Insulin can be administered through injections or an insulin pump. The dosage and frequency of insulin administration are determined based on individual needs.
Blood Sugar Monitoring
Regular monitoring of blood sugar levels is essential for maintaining optimal control. This is typically done using a blood glucose meter to measure the level of glucose in a small blood sample.
Healthy Eating and Meal Planning
A balanced and nutritious diet is crucial for individuals with juvenile diabetes. This includes monitoring carbohydrate intake, choosing foods with a low glycemic index, and balancing meals with protein and healthy fats.
Physical Activity and Exercise
Regular physical activity and exercise are important for overall health and blood sugar management. Consultation with healthcare professionals is recommended to develop an appropriate exercise plan that considers blood sugar fluctuations and insulin adjustments.
Education and Support
Education and support play a vital role in managing juvenile diabetes. It is important for individuals and their families to learn about the condition, insulin administration, blood sugar monitoring, and lifestyle modifications. Support groups and diabetes educators can provide valuable guidance and emotional support.
Preventing Complications
Effective management and prevention of complications are key priorities for individuals with juvenile diabetes. Here are some important preventive measures:
Blood Sugar Control
Maintaining stable blood sugar levels within the target range can help reduce the risk of complications. Regular monitoring, medication adherence, and lifestyle modifications are essential for achieving optimal blood sugar control.
Regular Check-ups
Regular check-ups with healthcare professionals, including endocrinologists and diabetes educators, are crucial for monitoring overall health and identifying any potential complications at an early stage.
Healthy Lifestyle Choices
Adopting a healthy lifestyle, including a balanced diet, regular physical activity, and sufficient sleep, can contribute to better overall health and improved blood sugar control.
Stress Management
Stress can impact blood sugar levels and overall well-being. It is important to develop effective stress management strategies, such as practicing relaxation techniques, engaging in hobbies, and seeking support when needed.
Managing Juvenile Diabetes in School
Proper management of juvenile diabetes is crucial during school hours. Here are some key considerations:
Creating an Individualized Healthcare Plan (IHP)
Working with school staff, parents, and healthcare professionals, an Individualized Healthcare Plan (IHP) should be developed to address the specific needs of the student with diabetes. This plan outlines appropriate medical care, blood sugar monitoring, insulin administration, and emergency procedures.
Communication with School Staff
Open communication between parents, healthcare providers, and school staff is essential. Teachers, coaches, and school nurses should be aware of the student’s condition, symptoms, treatment plan, and emergency contacts.
Managing Blood Sugar Throughout the School Day
Regular blood sugar monitoring, insulin administration, and meal/snack planning should be incorporated into the student’s daily routine. It is crucial to ensure snacks or glucose tablets are readily available in case of low blood sugar episodes.
Psychological Impact of Juvenile Diabetes
Living with juvenile diabetes can have a significant psychological impact. Here are some important aspects to consider:
Adjustment and Emotional Support
Adapting to the challenges of living with juvenile diabetes can be overwhelming. Emotional support from healthcare providers, family, and friends can help individuals and their families cope with the diagnosis and manage the emotional impact.
Managing Stress and Anxiety
The management of juvenile diabetes can be stressful, and chronic stress can impact blood sugar control. Practicing stress-reduction techniques, such as mindfulness, exercise, and seeking professional help when needed, can support overall well-being.
Coping with the Demands of Diabetes Management
Living with juvenile diabetes may require frequent blood sugar testing, insulin administration, meal planning, and lifestyle modifications. Developing effective coping strategies and finding a balance between diabetes management and daily life activities is crucial.
Research and Future Developments
Ongoing research and advancements in technology offer hope for improved management and potential cures for juvenile diabetes. Some areas of research include:
Advancements in Insulin Therapy
Researchers are continually developing new types of insulin and insulin delivery systems to enhance treatment options and improve blood sugar control.
Artificial Pancreas
The development of artificial pancreas systems, which continuously monitors blood sugar levels and automatically regulates insulin delivery, may revolutionize diabetes management and reduce the burden on individuals with juvenile diabetes.
Tissue Engineering and Transplantation
Scientists are exploring regenerative medicine approaches such as tissue engineering and transplantation to restore or replace the insulin-producing cells lost in juvenile diabetes. These promising developments may provide potential long-term solutions and even a cure for the condition.
In conclusion, juvenile diabetes, or type 1 diabetes, is a chronic condition that requires lifelong management. While the exact cause is still unknown, genetic factors, autoimmune response, and environmental triggers are thought to contribute to its development. Early recognition of symptoms, accurate diagnosis, and comprehensive treatment strategies, including insulin therapy and lifestyle modifications, are essential for optimal diabetes management. It is important to prioritize preventive measures, regular check-ups, and psychological support to minimize complications and support the well-being of individuals living with juvenile diabetes. Ongoing research offers hope for advancements in treatment options and potential cures, bringing optimism for the future of those affected by this condition.