In the world of medical science, diagnosing brain stem death is a critical process that requires meticulous assessment. Understanding the key factors involved in recognizing this condition is paramount in ensuring accurate diagnosis and appropriate medical interventions. From the cessation of brainstem reflexes to the absence of respiratory efforts, these telltale signs play a crucial role in determining the irreversibility of brain function loss. This article will shed light on the essential elements that physicians consider when diagnosing brain stem death, providing valuable insights into this complex medical phenomenon.
Key Factors in Diagnosing Brain Stem Death
Brain stem death is a critical medical condition in which there is irreversible loss of all brainstem functions. Diagnosing brain stem death requires a comprehensive evaluation, which involves the assessment of various clinical factors and the use of specialized diagnostic techniques. In this article, we will explore the key factors involved in diagnosing brain stem death and their importance in reaching an accurate diagnosis.
Clinical History and Examination
The clinical history and examination of the patient are crucial in diagnosing brain stem death. The patient’s medical history provides valuable information about the underlying conditions that may have contributed to the current state. Additionally, a detailed neurological examination helps the medical team assess the level of consciousness and the presence of brainstem reflexes. This examination provides vital clues regarding the functioning of the brainstem and aids in the diagnosis of brain stem death.
Neuroimaging
Neuroimaging techniques, such as computed tomography (CT) scan and magnetic resonance imaging (MRI), play a crucial role in diagnosing brain stem death. These imaging modalities help determine the underlying etiology of the loss of brainstem function. They also aid in excluding potentially reversible causes of the condition. The findings from neuroimaging studies further complement the clinical evaluation and enhance the accuracy of the diagnosis.
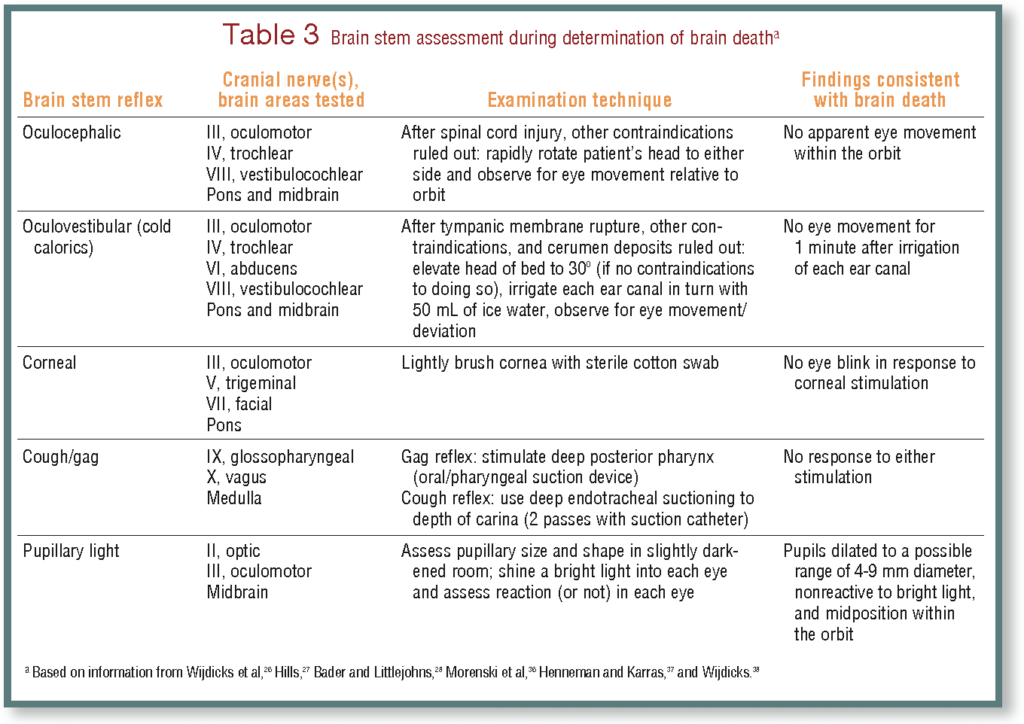
Brainstem Reflexes
A critical aspect of diagnosing brain stem death is assessing the presence of brainstem reflexes. These reflexes include the pupillary reflex, oculovestibular reflex, corneal reflex, gag reflex, cough reflex, swallowing reflex, and apnea reflex. The absence of these reflexes is indicative of brainstem dysfunction and supports the diagnosis of brain stem death. The evaluation of brainstem reflexes is a crucial component of the diagnostic process.
Electroencephalogram (EEG)
The electroencephalogram (EEG) is a valuable tool in diagnosing brain stem death. It involves monitoring the electrical activity of the brain and helps determine the presence or absence of cerebral cortex activity. In brain stem death, there is no detectable cerebral cortex activity on the EEG, further confirming the irreversible loss of brain function. The EEG serves as supportive evidence in the diagnosis of brain stem death.

Evoked Potentials
Evoked potentials are another important diagnostic tool utilized in the assessment of brain stem death. These include somatosensory evoked potentials (SSEPs), brainstem auditory evoked potentials (BAEPs), and visual evoked potentials (VEPs). The absence or significant impairment of evoked potentials indicates dysfunction of the brainstem and supports the diagnosis of brain stem death. Evoked potentials provide objective measurements and contribute to the comprehensive evaluation of the patient.
Apnea Testing
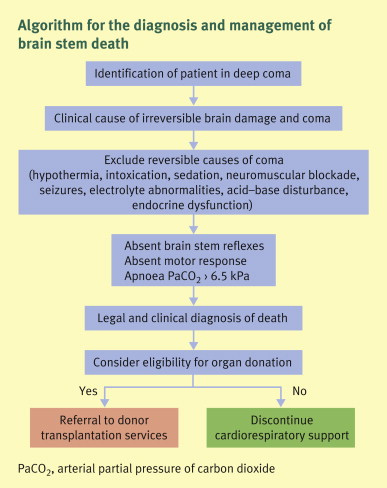
Apnea testing involves inducing controlled hypoventilation and monitoring arterial blood gases to assess the patient’s respiratory response. In brain stem death, there is an absent respiratory response, leading to an increase in carbon dioxide levels and a decrease in oxygen levels. The demonstration of absent respiratory response during apnea testing further strengthens the diagnosis of brain stem death.

Confirmation of Irreversible Cessation of Brain Function
To confirm the diagnosis of brain stem death, repeated clinical examinations and tests are conducted over an appropriate observation period. Consistent findings, such as the absence of brainstem reflexes, absence of cerebral cortex activity on EEG, and impaired evoked potentials, help confirm the irreversible cessation of brain function. The confirmation of irreversible brain function loss is crucial in the accurate diagnosis of brain stem death.
Exclusion of Confounding Factors
Properly conducted clinical and laboratory evaluations are essential in excluding confounding factors that may mimic brain stem death. Intoxication, hypothermia, heavy sedation, and neuromuscular blockade are among the factors that can cause coma and mimic the signs of brain stem death. A thorough evaluation helps rule out these confounding factors and ensures an accurate diagnosis of brain stem death.

Documentation and Legal Considerations
Documentation of the diagnostic process and the findings is of utmost importance in diagnosing brain stem death. This ensures proper record-keeping and helps with any legal considerations that may arise. The accurate and detailed documentation provides transparency and accountability in the evaluation of brain stem death cases.
Multidisciplinary Approach
Diagnosing brain stem death necessitates a multidisciplinary approach. Multiple medical specialists, including neurologists, neurosurgeons, intensivists, radiologists, and organ transplant coordinators, collaborate to evaluate the patient thoroughly. The expertise from various specialties ensures a comprehensive assessment and minimizes the possibility of errors in the diagnosis of brain stem death.
In conclusion, diagnosing brain stem death requires a systematic evaluation involving various key factors. The clinical history and examination, neuroimaging studies, assessment of brainstem reflexes, EEG, evoked potentials, apnea testing, confirmation of irreversible cessation of brain function, exclusion of confounding factors, documentation, and a multidisciplinary approach all contribute to an accurate diagnosis. Understanding these key factors is essential for medical professionals involved in the diagnosis of brain stem death and can have a significant impact on patient management and potential organ transplantation considerations.