As you walk into a hospital room, you are faced with the sight of an elderly patient lying in bed, seeking comfort and care. In this article, we will explore the essential nursing considerations that are crucial when providing care to aging patients. From identifying their specific healthcare needs to promoting active engagement in their own health, these key principles of nursing management will guide you in creating a nurturing and supportive environment for your elderly patients. So, let’s dive into the world of geriatric nursing and discover how you can make a significant difference in the lives of those who have contributed so much to society.

Physical Changes
As we age, our bodies undergo a variety of physical changes. These changes can affect various systems and organs, impacting our overall health and well-being. It is important for nurses to be aware of these changes in order to provide appropriate care and support to aging patients.
Vision changes
One of the most common age-related physical changes is a decline in vision. The lens of the eye becomes less flexible, making it harder to focus on close objects. This condition, known as presbyopia, can usually be corrected with reading glasses or bifocals. Additionally, older adults may develop conditions such as cataracts or age-related macular degeneration, which can further impact their vision. Nurses should be mindful of the need for frequent vision screenings and assistive devices such as magnifying glasses or large-print materials.
Hearing changes
Hearing loss is another common physical change that occurs with aging. Presbycusis, or age-related hearing loss, is typically gradual and affects the ability to hear high-frequency sounds. This can make it challenging for older adults to participate in conversations or hear important instructions from healthcare providers. Nurses should be patient and ensure clear communication, speaking slowly and directly facing the patient. The use of hearing aids and assistive listening devices may also be necessary.
Musculoskeletal changes
The musculoskeletal system undergoes several changes as we age. Bone density decreases, making older adults more prone to fractures or osteoporosis. Joint stiffness and reduced flexibility are also common, which can affect mobility and increase the risk of falls. Nurses should encourage regular exercise and physical therapy to help maintain muscle strength and joint flexibility. Additionally, providing assistive devices such as canes or walkers can assist with mobility and reduce the risk of accidents.
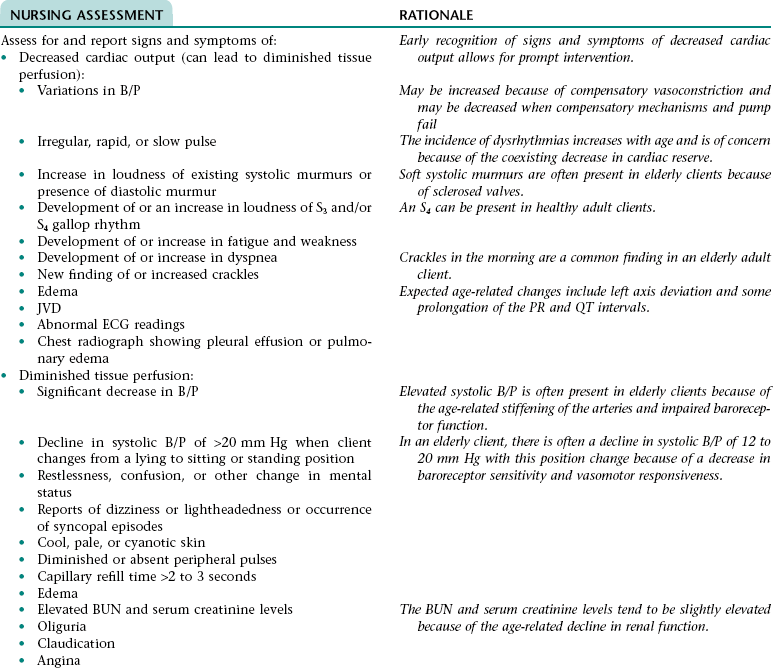
Cardiovascular changes
The cardiovascular system also undergoes changes as we age. The heart muscles may weaken, leading to a decrease in cardiac output and a slower resting heart rate. Blood vessels may become less elastic and more prone to hypertension or atherosclerosis. Nurses should closely monitor blood pressure and heart rate, as well as educate patients on the importance of a heart-healthy diet and regular exercise to maintain cardiovascular health.
Respiratory changes
The respiratory system undergoes changes that can affect breathing and lung function in older adults. Lung tissue becomes less elastic, and respiratory muscles may weaken, leading to a decrease in lung capacity. This can make it harder for older adults to breathe deeply or cough effectively, increasing the risk of respiratory infections. Nurses should promote practices such as deep breathing exercises and provide education on proper positioning and techniques for effective coughing to prevent complications such as pneumonia.
Cognitive Changes
In addition to the physical changes that occur with aging, there are also significant cognitive changes that can impact an individual’s mental abilities and functioning. Nurses must be aware of these changes in order to provide appropriate support and care to aging patients.
Memory decline
One of the most common cognitive changes associated with aging is memory decline. Older adults may experience difficulty recalling recent events or forgetfulness when it comes to tasks or appointments. Nurses should be patient and understanding, providing reminders and written instructions when necessary. It is important to differentiate normal age-related memory decline from more serious memory disorders, such as dementia, which require further assessment and intervention.
Decreased problem-solving abilities
As we age, our ability to solve complex problems or make decisions may decline. This can affect an individual’s ability to manage daily tasks or make informed choices about their healthcare. Nurses should provide support by breaking tasks into smaller steps and offering guidance when needed. Ensuring that older adults have access to appropriate resources and support systems, such as family members or caregivers, can also help compensate for decreased problem-solving abilities.
Confusion and delirium
Confusion and delirium are common cognitive changes seen in older adults, particularly during hospitalization or acute illness. Delirium is characterized by a sudden and fluctuating change in mental status, often due to an underlying medical condition or medication side effects. Nurses should carefully assess for signs of confusion or delirium and work closely with the healthcare team to identify and address the underlying cause. Providing a calm and familiar environment, as well as involving family members in the care plan, can help reduce confusion and delirium.
Dementia
Dementia is a progressive cognitive decline that affects memory, thinking, and behavior. It is not a normal part of aging but becomes more common as individuals get older. Nurses should be knowledgeable about the different types of dementia, such as Alzheimer’s disease, and be skilled in providing person-centered care to individuals with dementia. This includes creating a safe and supportive environment, promoting meaningful activities, and managing challenging behaviors with empathy and patience.
Depression and anxiety
Mental health concerns such as depression and anxiety are common in older adults. The aging process, loss of loved ones, and physical health problems can contribute to feelings of sadness and worry. Nurses should be alert to signs of depression and anxiety, such as changes in appetite or sleep patterns, social withdrawal, or increased agitation. They should provide emotional support, education on coping strategies, and facilitate referrals to mental health professionals when needed.

Medication Management
As individuals age, they often require multiple medications to address various health conditions. Nurses play a crucial role in medication management for aging patients, ensuring that medications are appropriate, safe, and effective.
Polypharmacy
Polypharmacy refers to the use of multiple medications, often prescribed by different healthcare providers, to manage an individual’s health conditions. While medications can be beneficial, polypharmacy increases the risk of adverse drug reactions, medication interactions, and medication non-adherence. Nurses should conduct thorough medication reconciliation and work closely with the healthcare team to simplify medication regimens and eliminate unnecessary medications.
Adverse drug reactions
Older adults are more susceptible to adverse drug reactions due to age-related changes in pharmacokinetics and pharmacodynamics. Nurses must closely monitor for signs and symptoms of adverse drug reactions, such as changes in vital signs, unusual bleeding, or cognitive impairment. Prompt reporting and collaboration with prescribers are essential to ensure timely intervention and prevent further complications.
Medication adherence
Medication adherence can be challenging for aging patients, particularly those with complex medication regimens or cognitive decline. Nurses should provide education and support to help older adults understand their medications, including purpose, dosage, and potential side effects. Simplifying medication regimens through the use of pill organizers or reminder systems can also improve adherence.
Potential drug interactions
Drug interactions occur when two or more medications interact in a way that alters their intended effects or causes adverse reactions. Older adults are at higher risk of drug interactions due to the use of multiple medications. Nurses should review medication profiles regularly and be knowledgeable about potential drug interactions. Interprofessional collaboration among healthcare providers is crucial to identify and manage drug interactions effectively.
Age-related changes in pharmacokinetics and pharmacodynamics
Pharmacokinetics refers to how medications are absorbed, distributed, metabolized, and excreted in the body. Aging can cause changes in these processes, resulting in altered medication response and increased risk of adverse effects. Pharmacodynamics, on the other hand, refers to how medications interact with receptors to produce a therapeutic effect. Age-related changes can also affect the way medications work in the body. Nurses should be aware of these age-related changes and adjust medication doses or frequencies as necessary to ensure optimal therapeutic outcomes and minimize adverse effects.
Fall Prevention
Falls are a significant concern for older adults and can lead to serious injuries or complications. Nurses play a key role in fall prevention and should implement strategies to identify fall risks and minimize hazards.
Fall risk assessment
Nurses should conduct a comprehensive fall risk assessment for aging patients, including evaluating factors such as medication use, mobility limitations, cognitive impairment, and environmental hazards. Falls risk assessment tools can aid in identifying individuals at high risk for falls. Based on the assessment, nurses can develop personalized care plans to address individual needs and reduce fall risk.
Environmental modifications
Creating a safe environment is essential in fall prevention. Nurses should assess the patient’s home or care setting for potential hazards such as loose rugs, uneven surfaces, or inadequate lighting. Modifying the environment by removing obstacles, installing handrails, or adding grab bars in bathrooms can greatly reduce the risk of falls.
Assistive devices
Assistive devices, such as canes, walkers, or bedside commodes, can provide support and stability for older adults with mobility issues. Nurses should assess the patient’s needs and capabilities and recommend appropriate assistive devices. Training on proper use and maintenance of these devices is also important.
Exercise and physical therapy
Regular exercise and physical therapy can help improve strength, balance, and coordination, reducing the risk of falls. Nurses should encourage aging patients to participate in appropriate exercise programs and refer them to physical therapy when necessary. Exercise routines should be tailored to the individual’s abilities and preferences.
Education on fall prevention
Nurses should educate aging patients and their families about fall prevention strategies. This includes teaching proper body mechanics, safe transferring techniques, and the importance of wearing appropriate footwear. Providing information on the use of assistive devices, such as walkers or canes, and reinforcing the need for regular exercise can also help prevent falls.

Nutrition and Hydration
Nutrition and hydration are essential components of healthy aging. Nurses should assess the nutritional status of aging patients and provide support to ensure adequate intake of nutrients and fluids.
Malnutrition and dehydration risk
Older adults are at increased risk of malnutrition and dehydration due to various factors, including decreased appetite, difficulty chewing or swallowing, and medication side effects. Nurses should monitor weight changes, signs of malnutrition (such as muscle wasting or poor wound healing), and signs of dehydration (such as dry mouth or decreased urine output). Nutritional and fluid intake should be assessed, and appropriate interventions, such as modified textures or increased fluid intake, should be implemented.
Weight management
Maintaining a healthy weight is important for overall health and well-being in older adults. Nurses should assess weight and body mass index (BMI) regularly and provide education on healthy eating habits and portion control. For individuals who are underweight or overweight, nurses should work closely with registered dietitians to develop personalized weight management plans.
Dietary considerations
Certain dietary considerations become more important as we age. Adequate intake of calcium and vitamin D is crucial for bone health and can help prevent osteoporosis. Nurses should assess dietary intake and educate aging patients on foods rich in these nutrients or recommend appropriate supplements when necessary. Special dietary considerations for conditions such as diabetes or kidney disease should also be addressed.
Supplemental nutrition
In some cases, older adults may require supplemental nutrition to meet their dietary needs. Nurses should assess nutritional intake and collaborate with registered dietitians to determine the need for oral nutritional supplements or enteral nutrition. Monitoring of nutritional status and regular reassessment are essential to ensure optimal outcomes.
Hydration strategies
Proper hydration is important for maintaining overall health and preventing complications such as urinary tract infections or constipation. Nurses should encourage aging patients to drink an adequate amount of fluids throughout the day and provide education on the signs and symptoms of dehydration. Offering fluids at regular intervals, providing assistance with drinking if necessary, and monitoring urine output can help ensure proper hydration.
Pain Management
Pain is a common concern among aging patients and can significantly impact their quality of life. Nurses play a crucial role in assessing and managing pain in older adults.
Assessment and screening
Nurses should conduct thorough pain assessments in aging patients, including evaluating the location, intensity, and quality of pain. Various pain assessment tools, such as numeric rating scales or verbal descriptors, can assist in quantifying pain. Additionally, nurses should consider the impact of pain on physical and psychosocial functioning to develop a comprehensive pain management plan.
Non-pharmacological approaches
Non-pharmacological interventions should be considered as part of a multimodal approach to pain management. Nurses can utilize techniques such as heat or cold therapy, massage, relaxation techniques, or cognitive-behavioral strategies to help alleviate pain. Providing a calming environment, distraction, or music therapy can also be beneficial.
Medication options
Pharmacological interventions may be necessary for managing pain in aging patients. Nurses should collaborate with prescribers to evaluate the appropriateness of analgesic medications, taking into consideration the potential risks and benefits, drug interactions, and age-related changes in drug metabolism. Regular reassessment of pain levels and medication effectiveness is essential to ensure optimal pain control.
Evaluation and reassessment
Nurses should closely monitor the effectiveness of pain management strategies and regularly reassess pain levels. The individual’s response to interventions should be evaluated, and adjustments to the pain management plan should be made as needed. Ongoing communication and collaboration with the healthcare team, as well as open dialogue with the patient and their family, are crucial in achieving optimal pain control.
Collaboration with pain specialists
In some cases, pain management may require the expertise of pain specialists, such as pain medicine physicians or palliative care teams. Nurses should advocate for their patients and facilitate referrals to pain specialists when necessary. Collaboration and communication with pain specialists are important to ensure a coordinated and comprehensive approach to pain management.

Skin Care
Proper skin care is essential for aging patients to maintain skin integrity and prevent complications such as pressure ulcers or infections. Nurses should assess skin health and implement preventive measures to promote optimal skin care.
Skin integrity assessment
Nurses should regularly assess the skin of aging patients to identify any changes or signs of skin breakdown. Paying attention to areas prone to pressure or friction, such as bony prominences or skin folds, is important. Early identification of skin issues allows for timely intervention and preventive measures.
Pressure ulcer prevention
Pressure ulcers, also known as bedsores or pressure sores, are a common complication in older adults, particularly those with limited mobility or chronic medical conditions. Nurses should implement strategies to prevent pressure ulcers, such as frequent repositioning, the use of pressure-relieving devices (e.g., specialized mattresses or cushions), and regular skin inspections. Education on proper skincare techniques and the importance of nutrition and hydration is also critical.
Wound care management
If a wound or skin breakdown occurs, nurses should provide appropriate wound care management. This includes cleaning the wound, applying appropriate dressings, and ensuring proper hygiene. Nurses should assess wound healing progress regularly and collaborate with wound care specialists if necessary.
Moisture-associated dermatitis
Moisture-associated dermatitis, such as incontinence-associated dermatitis or fungal infections, is common in aging patients. Nurses should assess for signs of skin irritation or infection in areas that are frequently exposed to moisture. Implementing preventive measures, such as the use of moisture barriers or absorbent products, can help maintain skin integrity.
Skin hygiene practices
Proper skin hygiene is important to prevent skin infections and maintain overall skin health. Nurses should educate aging patients on appropriate skincare practices, including gentle cleansing techniques, adequate hydration, and the use of moisturizers or emollients. Avoiding harsh chemicals or irritants and promoting regular bathing or showering can also help maintain skin cleanliness and integrity.
End-of-Life Care
End-of-life care is an essential aspect of nursing practice for aging patients nearing the end of their lives. Nurses should approach end-of-life care with compassion and provide comprehensive support to patients and their families.
Advanced care planning
Advanced care planning involves discussions between healthcare providers, patients, and their families to identify goals of care and preferences for end-of-life treatment. Nurses should facilitate these conversations and ensure that aging patients have the opportunity to express their wishes and make informed decisions about their care. Advance directive documents, such as living wills or healthcare proxies, should be reviewed and updated as needed.
Palliative and hospice care
Palliative and hospice care focus on providing comfort, managing symptoms, and improving quality of life for patients with serious illness or nearing the end of life. Nurses should collaborate with palliative and hospice care teams to develop individualized care plans that address physical, emotional, and psychosocial needs. Regular assessments and adjustments to the care plan are necessary to ensure optimal symptom management and support.
Symptom management
Symptom management is a critical aspect of end-of-life care for aging patients. Nurses should be knowledgeable about common end-of-life symptoms, such as pain, dyspnea, nausea, or anxiety, and implement appropriate interventions for relief. This may involve medication administration, non-pharmacological approaches, or referral to specialized palliative care teams or pain specialists.
Psychosocial support
End-of-life care encompasses not only physical needs but also emotional and psychosocial support. Nurses should provide compassionate and empathetic care, addressing the emotional needs of aging patients and their families. Active listening, therapeutic communication, and facilitating support groups or counseling services can help individuals cope with grief, loss, and other psychosocial challenges.
Ethical considerations
Ethical considerations are important in end-of-life care. Nurses should respect the autonomy and dignity of aging patients, ensuring that their wishes and values are honored. This may involve discussing ethical dilemmas or complex decisions with the healthcare team, advocating for patient rights, or seeking guidance from ethics committees or spiritual advisors. Open communication and collaboration among healthcare providers, patients, and families are essential in navigating these sensitive situations.
Communication and Advocacy
Effective communication and advocacy are essential for providing high-quality care to aging patients. Nurses should establish open and trusting relationships, involve patients and their families in decision-making, and advocate for their needs and preferences.
Effective communication strategies
Nurses should employ effective communication strategies when interacting with aging patients. This includes active listening, using clear and simple language, and allowing sufficient time for the patient to express their concerns or ask questions. Encouraging open dialogue, practicing empathy, and providing education on health conditions or treatment options can help enhance communication and promote patient-centered care.
Patient and family involvement
Involving patients and their families in healthcare decisions is crucial, particularly for aging patients who may have complex healthcare needs. Nurses should actively engage patients and families in care planning, ensuring that their perspectives, values, and goals are considered. Providing education, resources, and support to facilitate shared decision-making can help empower patients and their families to actively participate in their care.
Healthcare decision-making
As aging patients face healthcare decisions, nurses should support their autonomy and facilitate informed decision-making. This may involve explaining the benefits and risks of various treatment options, discussing prognosis, or providing access to additional resources or second opinions. Nurses should ensure that patients have the necessary information to make decisions that align with their values and preferences.
Respecting autonomy and dignity
Respecting the autonomy and dignity of aging patients is a fundamental aspect of nursing care. Nurses should uphold the rights of patients to make decisions about their own bodies and healthcare, even if their choices differ from that of the healthcare team. Respecting personal boundaries, privacy, and cultural or religious beliefs is crucial in maintaining the dignity of the individual.
Ensuring patient rights
Nurses should advocate for the rights of aging patients, ensuring that they receive safe, ethical, and quality care. This may involve addressing issues such as informed consent, privacy, or access to healthcare services. Nurses should be knowledgeable about patient rights, healthcare policies, and legal frameworks to effectively advocate for their patients’ needs and well-being.
Geriatric Syndromes
Geriatric syndromes are a group of conditions that are common in aging individuals and are characterized by a combination of medical, functional, and psychosocial issues. Nurses should be knowledgeable about these syndromes and provide appropriate care and support to aging patients.
Frailty syndrome
Frailty syndrome refers to a state of increased vulnerability and decreased resilience in aging individuals. It is characterized by physical and cognitive decline, fatigue, and increased susceptibility to adverse health outcomes. Nurses should assess for signs of frailty, such as decreased strength or functional decline, and implement appropriate interventions. This may include exercise programs, fall prevention strategies, nutrition support, and coordination of care with other healthcare providers.
Urinary incontinence
Urinary incontinence is a common geriatric syndrome characterized by the loss of bladder control. It can have a significant impact on an individual’s quality of life and increase the risk of falls, skin breakdown, or social isolation. Nurses should conduct thorough assessments to determine the type and cause of urinary incontinence and develop individualized management plans. This may involve lifestyle modifications, pelvic floor exercises, assistive devices, or referral to specialists for further evaluation and treatment.
Delirium
Delirium is a sudden and fluctuating change in mental status, often seen in older adults during hospitalization or acute illness. It is typically caused by an underlying medical condition, medication side effects, or environmental factors. Nurses should assess for signs of delirium, such as confusion or disorientation, and work closely with the healthcare team to identify and address the underlying cause. Providing a calm and familiar environment, maintaining a regular routine, and involving family members or familiar caregivers can help reduce delirium.
Geriatric depression
Depression is a common mental health concern among aging individuals, often characterized by persistent sadness, loss of interest or pleasure, or changes in appetite or sleep patterns. Nurses should assess for signs of depression and collaborate with mental health professionals to provide appropriate support and treatment. This may involve counseling, medication management, or referral to support groups or community resources.
Functional decline
Functional decline refers to a decrease in an individual’s ability to perform daily activities or maintain independence. It can be caused by various factors, including physical or cognitive decline, chronic conditions, or psychosocial issues. Nurses should assess functional abilities and provide appropriate interventions to maintain or improve independence. This may include physical therapy, occupational therapy, assistive devices, or modifications to the home environment. Regular reassessment and collaboration with the healthcare team are important to address changing needs and promote continued independence.