Managing Diabetes During Pregnancy
Pregnancy is a unique and transformative journey, but it can often pose significant challenges, especially if you are managing diabetes. It’s essential to understand how to navigate this beautiful yet complex phase of your life when you have a condition that requires careful management. In this guide, you’ll discover practical strategies and insights for managing diabetes during pregnancy, ensuring the health of both you and your baby.
Understanding Diabetes and Pregnancy
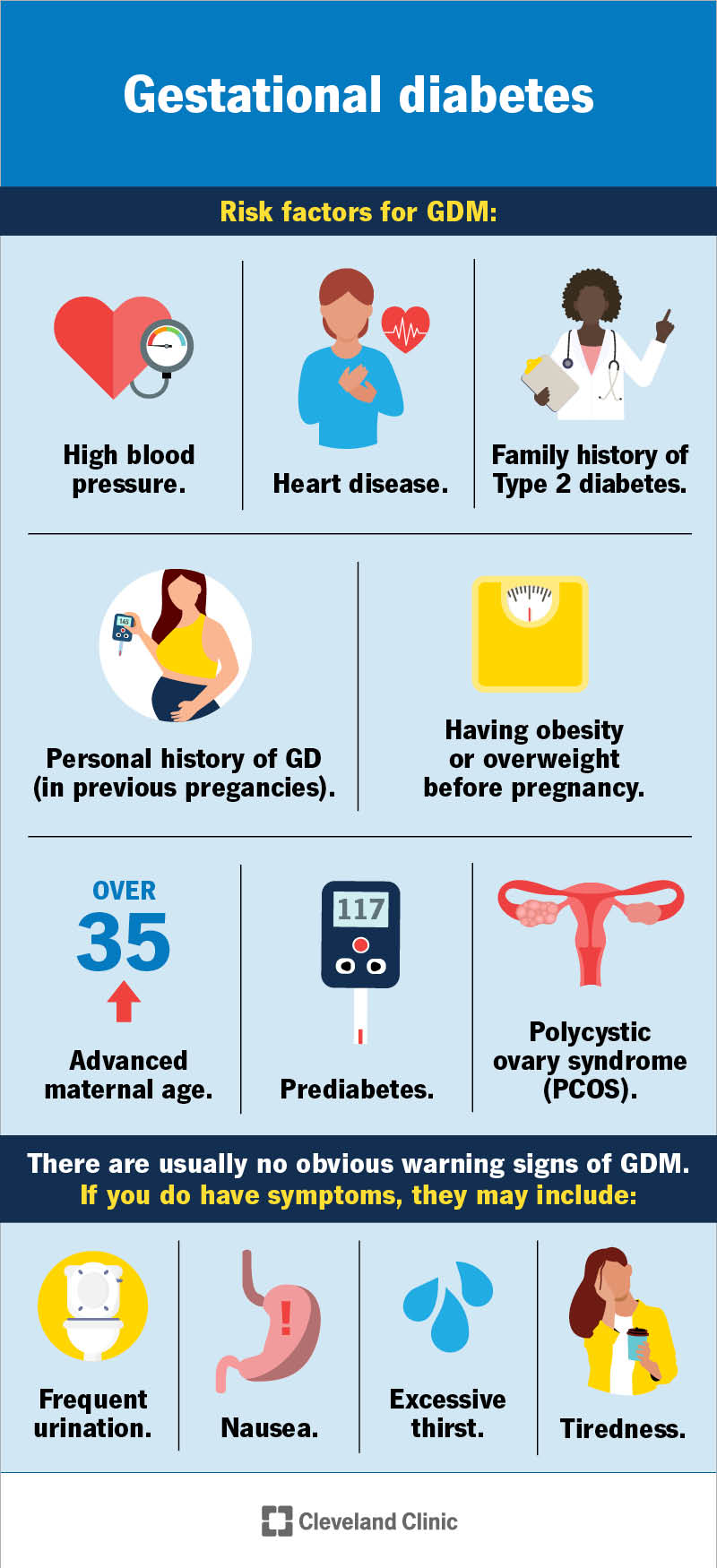
To begin, let’s clarify what diabetes is and how it might affect pregnancy. Diabetes is a condition characterized by high blood sugar levels, which can arise from insufficient insulin production or the body’s inability to respond to insulin effectively. There are several types of diabetes, with the most common being Type 1, Type 2, and Gestational Diabetes.
The Impact of Diabetes on Pregnancy
If you’re managing diabetes while expecting, it’s crucial to understand its implications. High blood sugar levels during pregnancy can lead to complications, such as the increased risk of miscarriage, preterm birth, and birth defects. Additionally, babies born to mothers with diabetes are at a higher risk for conditions like jaundice, low blood sugar, and obesity later in life.
Your Health Comes First
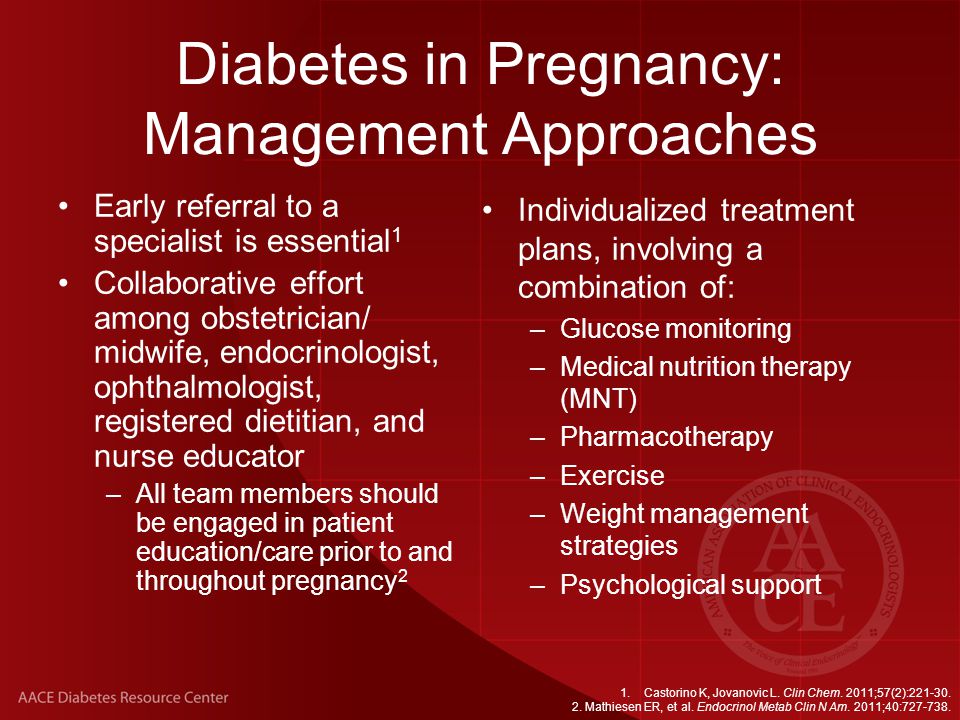
Throughout your pregnancy, prioritizing your health is not only vital for you but also for the well-being of your baby. It’s important to maintain good blood sugar control to minimize the risks associated with high glucose levels. This often requires working closely with your healthcare providers, including your obstetrician and diabetes care team.
Planning Your Pregnancy
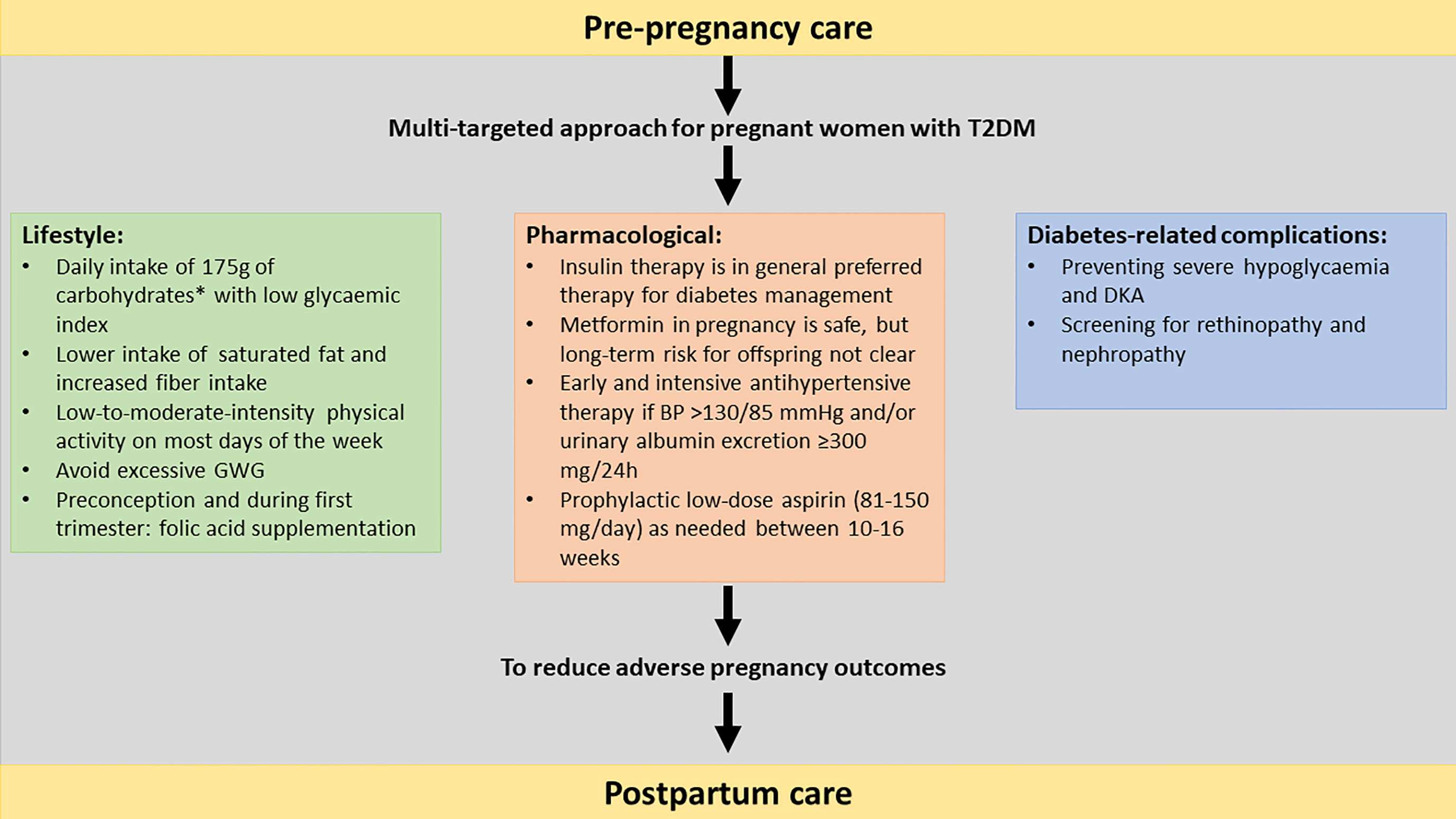
Before you embark on your pregnancy journey, planning is crucial. If you’re living with diabetes, consider taking the time to strategize with your healthcare provider. They can help you understand the importance of achieving optimal blood glucose levels before conceiving. This proactive approach can significantly reduce the risk of complications for you and your baby.
Preconception Counseling
Preconception counseling is an excellent opportunity to discuss your diabetes management while planning for pregnancy. Your healthcare provider will typically assess your overall health, discuss your diabetes management plan, and suggest necessary adjustments to align with your pregnancy goals. This might include reviewing your current medications, dietary habits, and exercise routines.
Setting Realistic Goals
Setting realistic and achievable goals with your medical team can help empower you throughout your pregnancy. Whether it’s aiming for target blood glucose levels or managing a healthy weight, focus on progress rather than perfection. Remember, pregnancy is a shared journey; it’s perfectly normal to have questions and concerns along the way.
Monitoring Your Blood Sugar Levels
Once you’re pregnant, regular monitoring of your blood sugar levels becomes even more critical. This will not only allow you to keep track of your health but also enable you to make timely adjustments to your diabetes management plan.
Frequency of Monitoring
You might find that the frequency of blood sugar checks increases during pregnancy. While individual needs vary, many healthcare providers recommend checking your levels several times a day, including before and after meals. This will give you a comprehensive view of how your body is responding to different foods and activities.
Understanding Your Target Ranges
Each person may have different target ranges for blood sugar levels during pregnancy based on individual health concerns. Generally, the American Diabetes Association suggests the following target ranges:
- Fasting: Less than 95 mg/dL
- 1 hour after meals: Less than 140 mg/dL
- 2 hours after meals: Less than 120 mg/dL
Consulting with your healthcare team is essential to ensure your targets are tailored to your specific situation.
Meal Planning and Nutrition
Eating well is one of the most effective ways to manage your diabetes during pregnancy. Proper nutrition will not only help regulate your blood sugar levels but also provide your growing baby with essential nutrients.
Choosing Balanced Meals
When meal planning, focus on creating balanced meals that include a mix of carbohydrates, protein, and healthy fats. Carbohydrates should be high in fiber and low in refined sugars. This might include whole grains, fruits, and vegetables. Pairing carbohydrates with protein can also help stabilize your blood sugar levels.
Portion Control
Portion control can play a crucial role in managing blood sugar levels. It’s natural to feel hungrier during pregnancy, but being mindful of portion sizes can help you avoid spikes in your blood glucose. Working with a nutritionist to develop a meal plan that suits your taste while adhering to diabetic guidelines can be incredibly beneficial.
Hydration Matters
Don’t forget about hydration! Drinking plenty of water is vital for both your health and your baby’s development. Staying hydrated helps your body regulate blood sugar levels more efficiently. Aim for at least eight glasses of water a day, and always listen to your body.

Physical Activity During Pregnancy
Keeping active is important, but when you’re managing diabetes, it’s vital to approach physical activity thoughtfully. Exercise can help control blood sugar levels, boost your mood, and even improve your overall well-being during your pregnancy.
Consult Your Healthcare Provider
Before beginning or modifying your exercise routine, consult your healthcare provider. They can guide you on what forms of exercise are safe and beneficial based on your specific medical history and current health status.
Types of Safe Exercises
Generally, moderate exercises like walking, swimming, and prenatal yoga can be ideal for pregnant individuals with diabetes. These activities can help you maintain a healthy weight, regulate blood sugar levels, and prepare your body for labor.
Listen to Your Body
Throughout your pregnancy, it’s essential to listen to your body. If you experience shortness of breath, dizziness, or discomfort while exercising, immediately slow down or stop. Your comfort and safety are paramount, so always prioritize your well-being.
Insulin and Medications
If you’re on insulin or other medications for diabetes, adjustments may be necessary during pregnancy. Insulin needs often change as your body and hormones fluctuate throughout this time.
Timing and Dosage Adjustments
Working with your healthcare provider to determine the right timing and dosage for your medications is crucial. You may need to monitor your blood sugar levels more frequently to understand how your body is responding and to make adjustments accordingly.
Possible Medication Changes
Some medications for diabetes may not be safe during pregnancy. Discuss any necessary changes with your healthcare provider, who will recommend safe alternatives that will protect both your health and your baby’s.
Managing Stress and Mental Health
It’s completely natural to feel anxious or overwhelmed at times while managing diabetes during pregnancy. Your mental health is just as important as your physical health, so take the time to address any concerns you may have.
Finding Support
Consider reaching out to support groups or engaging with fellow expectant mothers who may also have diabetes. Sharing experiences and advice can provide relief and help you feel less isolated in your journey. Additionally, don’t hesitate to talk to your healthcare provider about your feelings. They can offer resources and strategies to help you cope.
Mindfulness and Relaxation Techniques
Incorporating mindfulness and relaxation techniques into your daily routine can also be beneficial. Practicing yoga, meditation, or simple deep-breathing exercises can help reduce stress and promote a sense of calm during your pregnancy.
Regular Check-Ups and Monitoring
Routine prenatal check-ups are more important than ever when you have diabetes. During these visits, your healthcare provider will monitor your overall health, your baby’s growth and development, and your blood sugar levels.
Keeping Track of Appointments
Keeping a record of your appointments and any changes to your health can be helpful. This will enable both you and your healthcare provider to make informed decisions about your diabetes management during pregnancy. Never hesitate to voice any concerns or symptoms you may experience; these discussions are vital for your overall care.
Gestational Diabetes Screening
If you haven’t already been diagnosed with gestational diabetes, your healthcare provider will likely recommend screening between the 24th and 28th weeks of pregnancy. Regular testing will help identify any issues early on, allowing for timely interventions.

Preparing for Labor and Delivery
As your due date approaches, it’s time to think about your labor and delivery plan. Discuss your diabetes management plan with your healthcare provider well in advance to ensure everything goes smoothly on the big day.
Crafting a Birth Plan
A well-thought-out birth plan should include how you want to manage your diabetes during labor and delivery. Discuss any medications, diet, and monitoring you wish to have during this critical time. Having a plan not only eases your worries but also empowers your healthcare team to meet your specific needs.
Postpartum Care for Diabetes
After giving birth, postpartum care is equally important. Your diabetes management may change, and it’s crucial to follow up with your healthcare provider for any necessary adjustments. Keep in mind that gestational diabetes typically resolves itself after delivery, but it is essential to follow up regularly to monitor your health.
Staying Informed and Engaged
Being informed and proactive is vital in managing diabetes during pregnancy. Knowledge empowers you to make better decisions regarding your health and your baby’s well-being.
Educational Resources
Consider enrolling in educational programs focused on diabetes management and pregnancy. This can be an excellent way to gain valuable insights and connect with healthcare professionals who specialize in your needs.
Engaging With Your Healthcare Team
Maintaining open communication with your healthcare team is essential. Remember, they are your partners in this journey, and keeping them informed about your progress, concerns, or changes in your condition can make a significant difference in your care.
Celebrating Your Journey
Managing diabetes during pregnancy can be challenging, but it’s also filled with joy and anticipation. As you progress through this journey, take the time to celebrate the small victories. Whether it’s reaching a target blood sugar level, enjoying a healthy meal, or simply feeling your baby kick, these moments are worth cherishing.
Building a Supportive Network
Surround yourself with supportive friends and family who understand your journey—those who can celebrate your wins and encourage you through any difficulties. Building a supportive network is invaluable for navigating the complexities of pregnancy with diabetes.
Embracing Self-Care
Self-care plays an essential role in your well-being. Don’t forget to take time for yourself, whether that’s indulging in a favorite hobby, taking a warm bath, or simply resting. Nurturing your own mental and emotional health is just as important as managing diabetes.
Managing diabetes during pregnancy may feel overwhelming, but with the right knowledge, support, and care, you can navigate this journey successfully. Be patient with yourself, stay informed, and remember that your health and your baby’s health are worth the effort.
If you found this article helpful, please clap, leave a comment with your thoughts, and subscribe to my Medium newsletter for regular updates and more insightful content!