You’ve probably heard of diverticular disease, a common condition affecting the colon. In this article, we’ll explore some effective strategies for managing diverticular disease and improving your quality of life. From dietary changes to incorporating exercise into your routine, we’ll provide you with practical tips to help you take control of this condition. So let’s get started and learn how to effectively manage diverticular disease.

Overview of Diverticular Disease
Definition
Diverticular disease refers to a condition where small pouches, known as diverticula, form in the lining of your digestive system. These pouches can develop anywhere along the length of your colon, but they are most commonly found in the lower part of the large intestine. While many people with diverticula experience no symptoms or complications, some may develop diverticulitis – an infection or inflammation of the diverticula. It is important to understand the types, causes, and risk factors associated with diverticular disease, as well as its prevalence in order to prevent and manage the condition effectively.
Types of Diverticular Disease
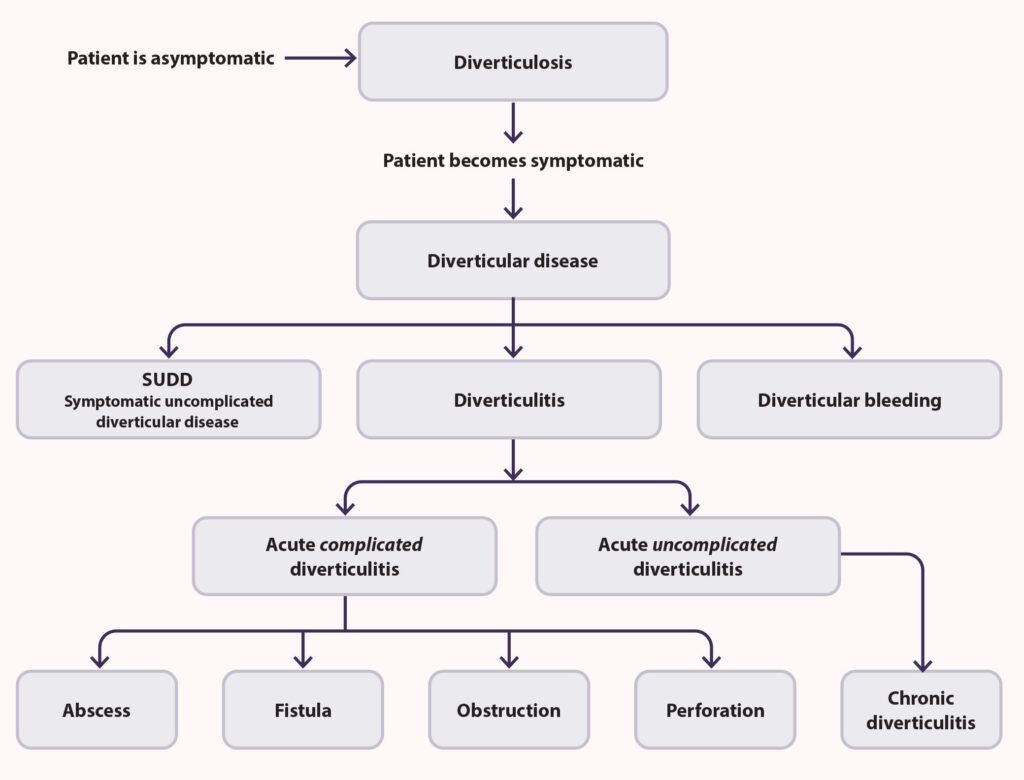
There are two main types of diverticular disease: diverticulosis and diverticulitis. Diverticulosis refers to the presence of small pouches or diverticula in the colon wall, whereas diverticulitis occurs when these pouches become inflamed or infected. While diverticulosis is usually asymptomatic, diverticulitis can cause severe abdominal pain and other complications. Understanding the difference between these two types is crucial for proper diagnosis and treatment.
Causes and Risk Factors
The exact cause of diverticular disease is not fully understood, but several factors are believed to contribute to its development. A primary cause is thought to be a diet low in fiber, which can lead to constipation and increased pressure in the colon, resulting in the formation of diverticula. Other risk factors include age (particularly over the age of 40), obesity, lack of exercise, smoking, and certain medications. By identifying these causes and risk factors, individuals can take proactive steps to prevent the onset of diverticular disease.
Prevalence
Diverticular disease is a common condition, especially in Western countries. In fact, it affects approximately 5-10% of people under the age of 50, and nearly 50% of individuals over the age of 60. The prevalence of diverticular disease increases with age, making it an important health concern for older adults. By understanding the scope of the condition’s prevalence, healthcare professionals and individuals alike can allocate appropriate resources and prioritize prevention and management strategies.
Symptoms of Diverticular Disease
Abdominal Pain
One of the most common symptoms of diverticular disease is abdominal pain. The pain typically occurs in the lower left side of the abdomen and can range from mild discomfort to severe and debilitating. It may come and go or persist for extended periods. The exact cause of this pain is not fully understood, but it may be related to the inflammation or infection of diverticula. If you experience persistent or severe abdominal pain, it is important to seek medical attention for proper diagnosis and treatment.
Bloating and Gas
Diverticular disease can also cause bloating and excessive gas production. This can result from the altered movement of digested food through the colon, leading to fermentation and the release of gases. Bloating and gas can cause discomfort and may contribute to abdominal distension. Managing these symptoms often involves dietary modifications and ensuring adequate fluid intake.
Change in Bowel Habits
Diverticular disease can disrupt your normal bowel habits. You may experience changes in stool consistency, frequency, or urgency. Some individuals may develop constipation, while others may experience diarrhea. These changes can be attributed to the presence of diverticula and inflammation of the colon. Monitoring your bowel habits and discussing any changes with your healthcare provider can help determine appropriate management strategies.
Rectal Bleeding
Occasionally, diverticular disease may cause rectal bleeding. This can manifest as bright red blood in your stool or on the toilet paper. Rectal bleeding can be alarming, and it is essential to seek medical attention to determine the cause and ensure proper management. While diverticular bleeding is typically mild and self-limiting, in some cases, it may require more intensive treatment or monitoring.
Diagnosis of Diverticular Disease
Medical History and Physical Examination
To diagnose diverticular disease, your healthcare provider will begin by taking a detailed medical history and performing a physical examination. They will inquire about your symptoms, family history, and any risk factors that may contribute to the development of the condition. Additionally, they may palpate your abdomen to assess for tenderness or signs of infection. A comprehensive evaluation of your medical history and physical examination can provide valuable insights for further diagnostic testing.
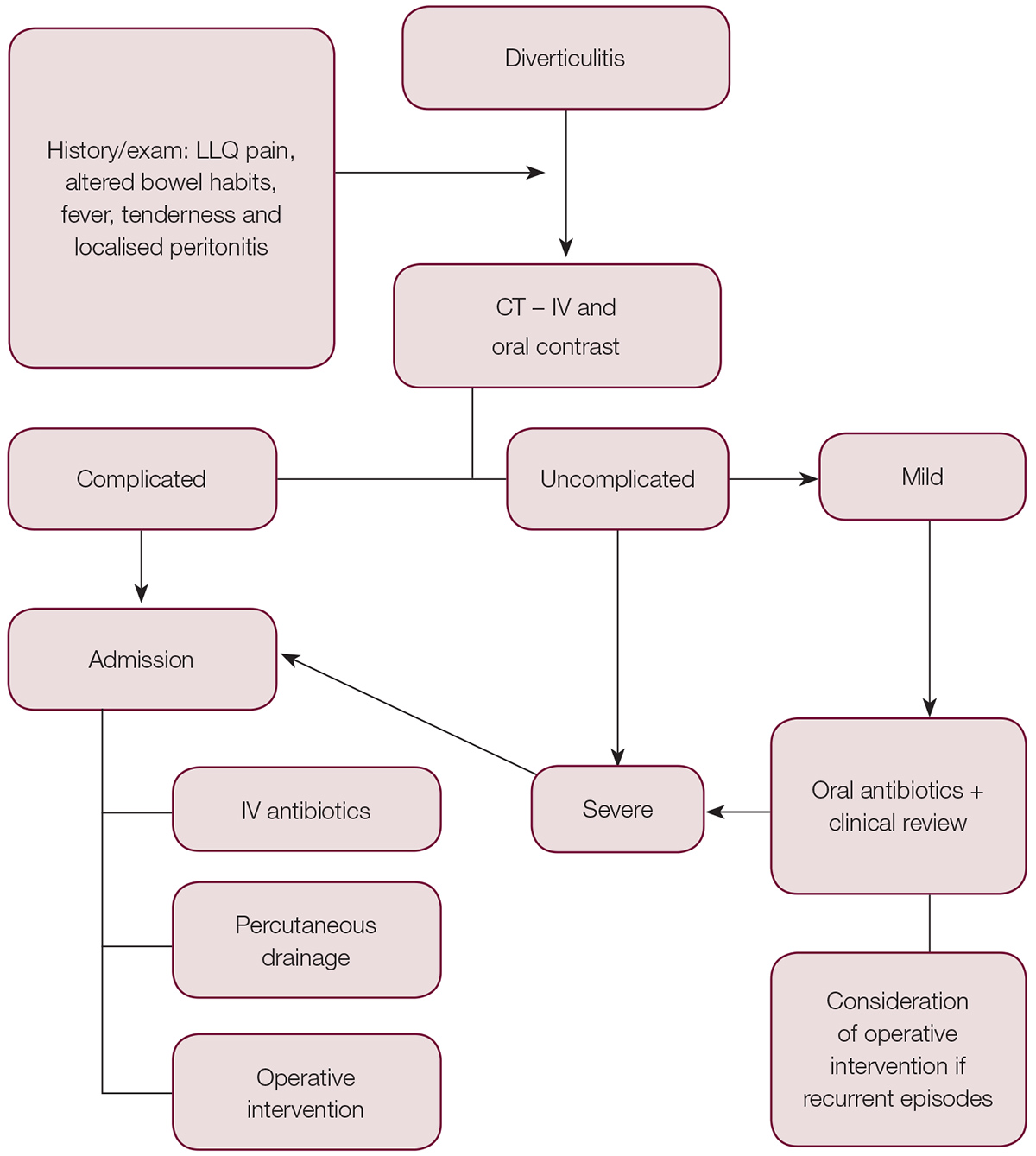
Imaging Tests
Imaging tests play a crucial role in the diagnosis of diverticular disease. Two commonly used imaging techniques are a computerized tomography (CT) scan and an abdominal ultrasound. A CT scan provides detailed cross-sectional images of your abdomen, allowing your healthcare provider to identify any diverticula, signs of inflammation, or complications such as abscesses. An abdominal ultrasound uses high-frequency soundwaves to create images of your abdomen, providing information about the structure and condition of your organs. These imaging tests are important tools in confirming the presence of diverticular disease and assessing its severity.
Colonoscopy
In some cases, a colonoscopy may be performed to visualize the colon and confirm the presence of diverticular disease. During a colonoscopy, a flexible tube with a camera at the tip is inserted into the rectum and guided through the colon. This procedure allows for a detailed examination of the colon wall and can help identify diverticula, signs of inflammation, or any other abnormalities. A colonoscopy is particularly useful in ruling out other conditions and guiding treatment decisions.
Laboratory Tests
Laboratory tests may be conducted to support the diagnosis of diverticular disease and assess its severity. Blood tests, such as a complete blood count (CBC), can help detect signs of infection or inflammation. Additional tests, such as stool analysis or a fecal occult blood test, may be ordered to assess for the presence of blood in the stool or any other abnormalities. These laboratory tests can provide valuable information to assist with the diagnosis and management of diverticular disease.
Treatment Options for Diverticular Disease
Dietary Changes and Fiber Intake
(…)