Living with Meniere’s Disease can be challenging, but with the right management techniques, it is possible to gain control over its symptoms. This article explores various strategies and lifestyle adjustments that can help you effectively manage Meniere’s Disease symptoms. From incorporating a low-sodium diet and practicing stress-reducing techniques to seeking medical support, this article provides valuable insights into finding relief and regaining control over your daily life. Find out how you can navigate the ups and downs of Meniere’s Disease with confidence and take charge of your well-being.

Understanding Meniere’s Disease
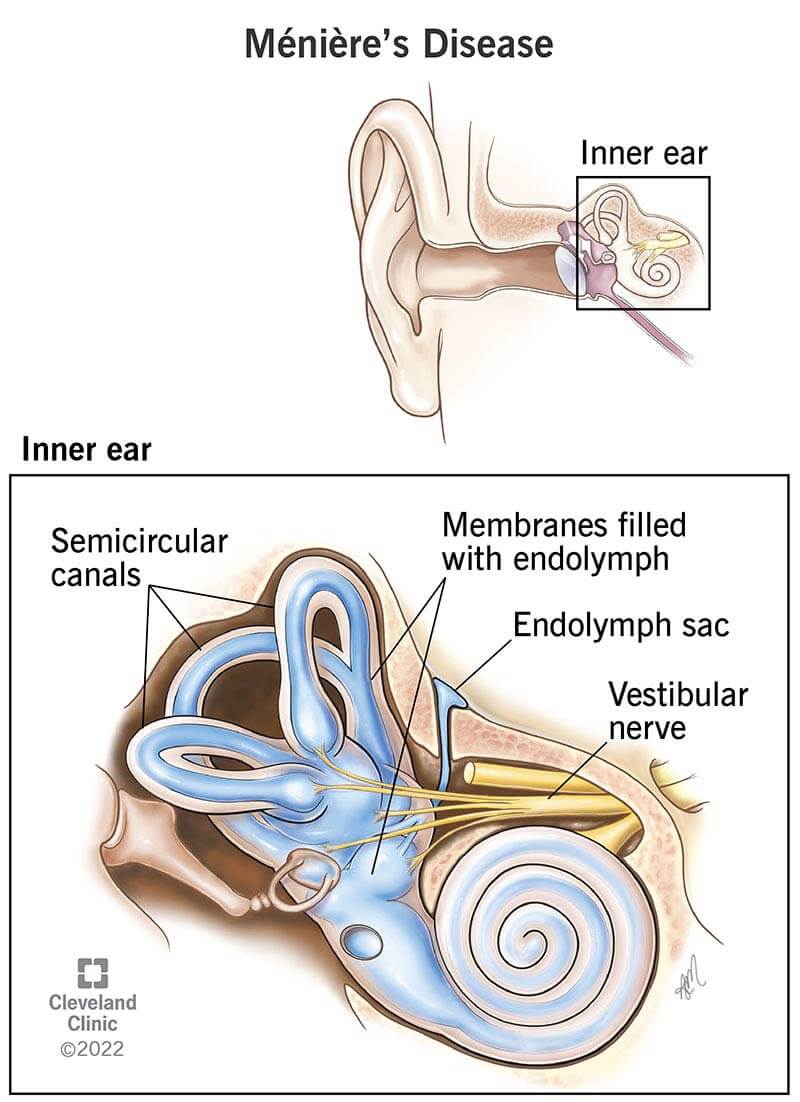
Meniere’s Disease is a chronic condition that affects the inner ear, causing episodes of vertigo, tinnitus (ringing in the ears), hearing loss, and a feeling of fullness or pressure in the affected ear. It is named after the French physician Prosper Ménière, who first described the condition in 1861. Meniere’s Disease is considered a relatively rare disorder, affecting approximately 615,000 individuals in the United States alone. While the exact cause of Meniere’s Disease remains unknown, there are several theories as to its origins.
What is Meniere’s Disease?
Meniere’s Disease is a disorder of the inner ear that can lead to a variety of symptoms, including vertigo, tinnitus, hearing loss, and a feeling of fullness or pressure in the ear. These symptoms can be debilitating and greatly affect one’s quality of life. Meniere’s Disease typically affects one ear, but can eventually progress to both ears over time. The severity and frequency of symptoms can vary from person to person, with some individuals experiencing frequent attacks, while others might have long periods without any symptoms.

Causes of Meniere’s Disease
The exact cause of Meniere’s Disease remains unknown, although there are several theories as to what may contribute to its development. One common theory suggests that Meniere’s Disease is caused by an accumulation of fluid within the inner ear, known as endolymphatic hydrops. This excess fluid can disrupt the normal balance and pressure within the ear, leading to the symptoms associated with Meniere’s Disease. Other potential causes include genetic factors, autoimmune reactions, viral infections, and abnormal blood vessel constriction.
Symptoms of Meniere’s Disease
Meniere’s Disease is characterized by a cluster of symptoms that can vary in severity and duration. The most common symptoms include:
-
Vertigo: A spinning sensation that can last for several minutes to hours. During an episode of vertigo, individuals may experience dizziness, a loss of balance, and difficulty walking.
-
Tinnitus: A persistent ringing, buzzing, or roaring sound in the affected ear. Tinnitus can range from mild to severe and can be particularly bothersome during periods of quiet or at night.
-
Hearing Loss: Individuals with Meniere’s Disease may experience fluctuating hearing loss in the affected ear. This can range from mild to profound and may come and go during episodes of vertigo.
-
Ear Fullness: Many individuals with Meniere’s Disease report a feeling of pressure or fullness in the affected ear. This sensation can be uncomfortable and may contribute to difficulties with hearing and balance.
If you are experiencing these symptoms, it is important to consult with a healthcare professional for a proper diagnosis.

Diagnosing Meniere’s Disease
While there is no specific test to definitively diagnose Meniere’s Disease, healthcare professionals use a combination of medical history, physical examination, and specialized tests to make a diagnosis. The diagnostic process typically involves ruling out other possible causes of the symptoms and identifying the characteristic pattern of Meniere’s Disease.
Medical History and Physical Examination
During the medical history portion of the diagnostic process, your healthcare professional will ask you questions about your symptoms, their frequency and duration, and any factors that may trigger or worsen them. They will also inquire about your medical history and any pre-existing conditions that may be relevant. A physical examination may also be performed to assess your balance, coordination, and the function of your ears.
Hearing and Balance Tests
Hearing tests, such as pure-tone audiometry and speech audiometry, are commonly used to assess the extent and nature of hearing loss in individuals suspected of having Meniere’s Disease. Balance tests, such as the Dix-Hallpike maneuver and electronystagmography (ENG), may also be conducted to evaluate the function of your inner ear and vestibular system.
Tests to Differentiate Meniere’s Disease from Other Conditions
In some cases, additional tests may be required to differentiate Meniere’s Disease from other conditions that present with similar symptoms. These tests may include magnetic resonance imaging (MRI) to rule out tumors or other abnormalities, blood tests to check for underlying autoimmune conditions or infections, and electrocochleography to assess the electrical activity in the inner ear.
Managing Meniere’s Disease
Although there is currently no cure for Meniere’s Disease, there are various treatment options available to help manage the symptoms and improve quality of life. The goal of treatment is to reduce the frequency and severity of attacks, alleviate symptoms, and prevent long-term hearing loss. The treatment approach may vary depending on the individual and the specific symptoms experienced.
Lifestyle Changes
Making certain lifestyle changes can play a crucial role in managing Meniere’s Disease. Stress management techniques, such as relaxation exercises and mindfulness, can help reduce the impact of stress on symptoms. Improving sleep habits, such as establishing a regular sleep schedule and creating a calming sleep environment, can also contribute to symptom management. Additionally, avoiding triggering factors, such as loud noises, bright lights, and sudden head movements, can help minimize the occurrence of episodes.
Dietary Modifications
Dietary modifications may be recommended for individuals with Meniere’s Disease, as certain foods and substances can potentially trigger or worsen symptoms. Reducing sodium intake is often advised, as excessive salt consumption can lead to increased fluid retention in the body, potentially exacerbating symptoms. Limiting caffeine and alcohol consumption is also recommended, as they can have a stimulant effect and worsen symptoms. Identifying and avoiding trigger foods, such as high-sugar or processed foods, can also be beneficial.
Medications
Medications can be prescribed to manage the symptoms associated with Meniere’s Disease. Diuretics, commonly known as water pills, may be prescribed to reduce fluid retention and help regulate the fluid balance within the inner ear. Anti-vertigo medications, such as antihistamines or anticholinergics, can alleviate vertigo symptoms. Anti-nausea medications may also be prescribed to control nausea and vomiting during episodes of vertigo. In certain cases, steroids or antibiotics may be used for their anti-inflammatory or antimicrobial properties.
Non-Drug Therapies
Non-drug therapies can be effective in managing Meniere’s Disease symptoms and improving quality of life. Vestibular rehabilitation, a form of physical therapy, can help retrain the brain to compensate for vestibular dysfunction and improve balance and coordination. Cognitive-behavioral therapy (CBT) can help individuals develop coping strategies to manage anxiety or depression associated with Meniere’s Disease. Hearing aids can be beneficial for individuals with hearing loss, while ear pressure regulating devices can help alleviate symptoms of ear fullness.
Coping Strategies for Meniere’s Disease
Living with Meniere’s Disease can be challenging, both physically and emotionally. However, there are coping strategies that can help individuals navigate their journey with the condition.
Building a Support Network
One of the most important coping strategies is building a support network. Reach out to friends, family, and support groups to share your experiences and seek emotional support. Connecting with others who are going through similar challenges can provide validation, encouragement, and helpful tips for managing symptoms.
Educating Yourself and Others
Knowledge is empowering. Take the time to educate yourself about Meniere’s Disease, its symptoms, and treatment options. This will help you better understand your condition and communicate effectively with your healthcare team. It’s also essential to educate your loved ones and those around you about Meniere’s Disease, as it will enable them to support you better and be more understanding of your needs.
Managing Anxiety or Depression
Dealing with a chronic condition such as Meniere’s Disease can lead to feelings of anxiety or depression. It is important to prioritize your mental well-being and seek professional help if needed. Cognitive-behavioral therapy (CBT) and other therapeutic techniques can assist in managing these emotions and building resilience.
Surgical Options for Meniere’s Disease
In some cases, when medical management fails to provide relief, surgical interventions may be considered. These procedures are typically reserved for individuals with severe and debilitating symptoms that significantly affect their quality of life.
Endolymphatic Sac Decompression
Endolymphatic sac decompression is a surgical procedure aimed at improving fluid drainage and normalizing inner ear pressure. During the procedure, a small portion of the bone is removed to create an additional pathway for the fluid to drain out of the inner ear. This can potentially reduce the frequency and severity of vertigo episodes.
Vestibular Nerve Section
Vestibular nerve section involves cutting or blocking the vestibular nerve, which helps transmit signals from the inner ear to the brain. This procedure is typically performed when other treatment options have failed to provide relief. By interrupting the signals from the affected ear, vertigo symptoms can be alleviated, although this procedure may result in mild imbalance or dizziness.
Labyrinthectomy
Labyrinthectomy is a procedure that involves removing the entire inner ear structures responsible for balance and hearing. This procedure is typically reserved for severe cases of Meniere’s Disease with profound hearing loss and debilitating vertigo. After the procedure, individuals lose all hearing in the affected ear but experience relief from vertigo symptoms.
Cochlear Implant
For individuals who have severe hearing loss as a result of Meniere’s Disease, a cochlear implant may be an option. A cochlear implant is an electronic device that bypasses the damaged parts of the inner ear and directly stimulates the auditory nerve, allowing individuals to perceive sound.

Tips for Living with Meniere’s Disease
While managing Meniere’s Disease can be a lifelong journey, there are practical tips and strategies that can help individuals better cope with the condition and improve their overall well-being.
Maintaining Regular Check-ups
Regular check-ups with your healthcare professional are essential for monitoring your condition and making any necessary adjustments to your treatment plan. These appointments also provide an opportunity to discuss any concerns or changes in symptoms.
Keeping a Symptom Diary
Keeping a symptom diary can be immensely helpful in tracking patterns and identifying triggers or factors that worsen your symptoms. Documenting details such as the date, time, duration, and severity of symptoms, as well as any potential triggers, can provide valuable information for you and your healthcare team.
Adapting Your Home and Work Environment
Making simple modifications to your home and work environment can help minimize the impact of Meniere’s Disease on your daily life. For example, reducing clutter to prevent tripping hazards, using handrails in staircases, and installing grab bars in the bathroom can improve safety and reduce the risk of falls during vertigo episodes.
Planning for Emergencies
Preparing for emergencies is essential, especially for individuals with Meniere’s Disease. Keep a list of emergency contacts, including your healthcare professional’s contact information, readily available. It may also be helpful to inform your family, friends, or coworkers about your condition and provide them with information on how to assist you during an episode.
In conclusion, Meniere’s Disease is a complex condition that can significantly impact an individual’s life. However, with proper management strategies, support, and medical interventions, individuals with Meniere’s Disease can lead fulfilling lives. By understanding the nature of the disease, implementing lifestyle changes, following treatment plans, and seeking support, it is possible to effectively manage symptoms and minimize their impact. Remember, you are not alone, and there are resources available to help you on your journey with Meniere’s Disease.