In this article, we will explore the important nursing considerations and care that need to be provided to patients with PMDD, also known as Premenstrual Dysphoric Disorder. This condition affects a significant number of women, and understanding how to effectively manage and support them during their monthly cycle is crucial. By examining the symptoms, potential risk factors, and evidence-based approaches to treatment, you will gain valuable insight into the compassionate care needed for patients with PMDD. Let’s dive in and discover the key nursing considerations in supporting these individuals through their journey.

Understanding PMDD
Definition of PMDD
Premenstrual Dysphoric Disorder (PMDD) is a severe form of premenstrual syndrome (PMS) that affects a small percentage of menstruating individuals. It is characterized by a cluster of physical, emotional, and psychological symptoms that occur during the late luteal phase of the menstrual cycle and significantly impact the daily functioning and quality of life of those affected.
Difference between PMDD and PMS
While both PMDD and PMS share some common symptoms, the key difference lies in the severity and impact of these symptoms. PMS refers to a milder set of symptoms that occur before menstruation and may cause discomfort, irritability, and temporary changes in mood. On the other hand, PMDD involves more severe symptoms that are disruptive to daily life, leading to significant distress and impairment in functioning.
Prevalence of PMDD
PMDD is estimated to affect between 3% to 8% of menstruating individuals. It is believed to be underdiagnosed and often mistaken for PMS due to overlapping symptoms. The exact cause of PMDD is still uncertain, but hormonal changes, genetic factors, and underlying neurotransmitter imbalances are believed to play a role in its development.
Assessment and Diagnosis
Recognizing symptoms of PMDD
Identifying the symptoms of PMDD is crucial for accurate diagnosis and appropriate management. These symptoms typically occur in the week before menstruation and subside shortly after the start of the menstrual flow. Common emotional and psychological symptoms include severe depression, anxiety, mood swings, irritability, and feelings of hopelessness. Physical symptoms may include breast tenderness, joint or muscle pain, fatigue, and bloating.
Diagnostic criteria for PMDD
In order to diagnose PMDD, healthcare professionals use specific criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). These criteria require the presence of at least five physical and/or psychological symptoms, and at least one of the symptoms must be related to mood disturbances, such as depression, anxiety, anger, or irritability.
Patient history and physical examination
To support the diagnosis of PMDD, a comprehensive patient history and physical examination are essential. The healthcare provider will gather information about the patient’s menstrual cycle and determine whether the symptoms are cyclical and related to the luteal phase. A physical examination may be conducted to rule out other underlying conditions that may present with similar symptoms.
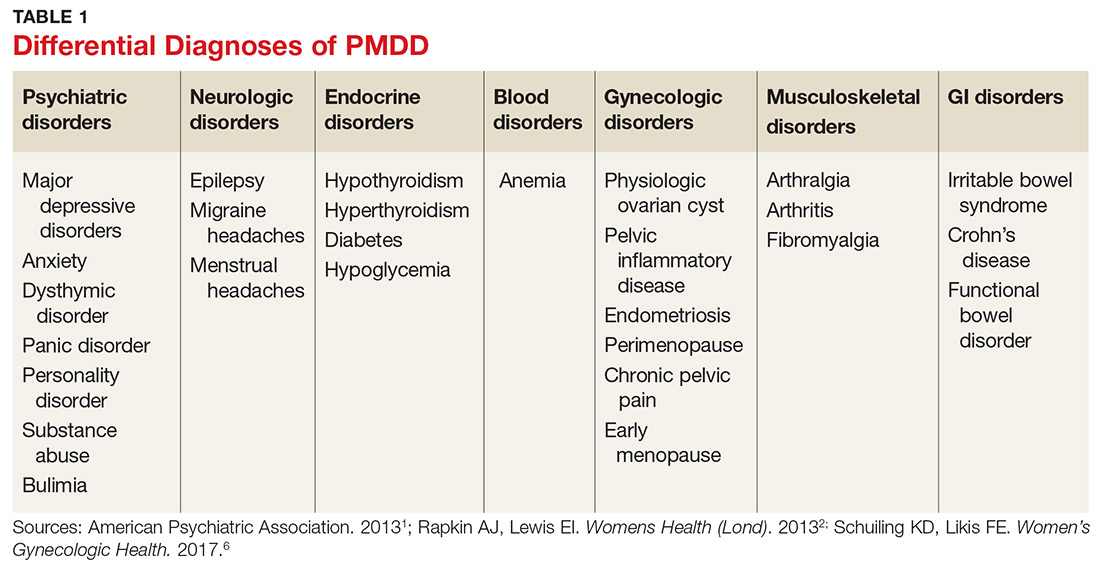
Differential diagnoses
It is important to consider other conditions that may present with similar symptoms to PMDD. Conditions such as major depressive disorder, anxiety disorders, bipolar disorder, and thyroid disorders can mimic the symptoms of PMDD. A thorough evaluation is necessary to differentiate PMDD from these other conditions and ensure appropriate treatment.

Collaborative Care Team
Roles and responsibilities of nurses
Nurses play a vital role in the care of patients with PMDD. They provide comprehensive assessments, administer medications, implement non-pharmacological interventions, and educate patients about their condition and available treatment options. Nurses also monitor and evaluate the effectiveness of interventions, provide emotional support, and promote self-care practices. Additionally, they collaborate with other healthcare professionals to ensure holistic and patient-centered care.
Collaboration with other healthcare professionals
Managing PMDD requires a collaborative approach involving healthcare professionals from various disciplines. Nurses work closely with physicians, psychiatrists, psychologists, and other mental health professionals to develop individualized treatment plans based on the patient’s needs. This interdisciplinary approach ensures that patients receive comprehensive care that addresses both their physical and psychological symptoms.
Interdisciplinary approach to PMDD management
An interdisciplinary approach is essential for the effective management of PMDD. The collaborative care team may include healthcare professionals such as gynecologists, endocrinologists, psychiatrists, primary care physicians, nurses, and mental health counselors. By working together, the team can provide a well-rounded and comprehensive approach to treatment that takes into account the multidimensional nature of PMDD.
Pharmacological Interventions
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are commonly prescribed as first-line pharmacological treatment for PMDD. These medications help regulate serotonin levels in the brain, which can alleviate the emotional and psychological symptoms associated with PMDD. Examples of SSRIs include fluoxetine, sertraline, and escitalopram. It is important for healthcare providers to closely monitor patients for any potential side effects or adverse reactions.
Hormonal therapy
Hormonal therapy, such as the use of combined oral contraceptives or progesterone-only contraceptives, may be beneficial in managing the symptoms of PMDD. These medications help regulate hormone levels and stabilize the menstrual cycle, reducing the severity of both physical and psychological symptoms. However, hormonal therapy may not be suitable for everyone and should be carefully evaluated on an individual basis.
Other medications for symptom management
In some cases, other medications may be prescribed to manage specific symptoms associated with PMDD. For example, nonsteroidal anti-inflammatory drugs (NSAIDs) may help relieve physical symptoms such as breast tenderness and pain. Anti-anxiety medications or mood stabilizers may be prescribed for individuals with severe anxiety or mood disturbances.
Patient education and medication adherence
Patient education plays a crucial role in ensuring optimal medication adherence and treatment outcomes. Nurses should provide clear and concise information about the prescribed medications, including potential side effects and interactions. They should also encourage open communication, address any concerns or questions, and emphasize the importance of taking medications as prescribed.
Non-pharmacological Interventions
Cognitive-behavioral therapy (CBT)
CBT is a type of therapy that focuses on changing negative thought patterns and behaviors. It has shown promise in the management of PMDD by helping individuals develop coping strategies and improve their overall well-being. CBT can be done individually or in a group setting, and it provides patients with tools to identify and challenge negative thoughts, manage stress, and regulate emotions.
Relaxation techniques and stress management
Stress can exacerbate the symptoms of PMDD, so learning relaxation techniques and stress management strategies can be beneficial. Patients can be encouraged to practice deep breathing exercises, meditation, mindfulness, or engage in stress-reducing activities such as yoga or tai chi. These techniques can help mitigate the impact of stress on both the body and mind.
Exercise and physical activity
Regular exercise and physical activity have been shown to have a positive impact on mood and overall well-being. Encouraging patients to engage in moderate-intensity aerobic activities, such as brisk walking, jogging, or cycling, can help alleviate symptoms of PMDD. Exercise releases endorphins, which are natural mood elevators, and promotes a sense of well-being.
Dietary modifications and nutritional counseling
Certain dietary modifications may help manage the symptoms of PMDD. Encouraging a balanced diet rich in whole grains, fruits, vegetables, and lean proteins can provide the necessary nutrients and help stabilize mood. Limiting the intake of caffeine, alcohol, and refined sugars may also be beneficial. Nutritional counseling can help patients make informed choices about their diet and its impact on their symptoms.
Symptom Management
Addressing mood and emotional changes
The management of mood and emotional changes is a key aspect of PMDD care. Healthcare professionals can provide support and validation to individuals experiencing intense emotions and work with them to develop coping strategies. Encouraging patients to engage in activities they enjoy, practice mindfulness, and seek social support can help alleviate mood disturbances.
Managing physical symptoms
Physical symptoms associated with PMDD can be managed through a combination of medication and non-pharmacological interventions. Medications such as NSAIDs can relieve pain and inflammation, while relaxation techniques and heat therapy can help alleviate muscle aches and breast tenderness. Adequate rest, hydration, and a balanced diet can also contribute to overall physical well-being.
Promoting healthy coping mechanisms
Promoting healthy coping mechanisms is essential in empowering individuals with PMDD to effectively manage their symptoms. This may involve teaching stress reduction techniques, encouraging creative outlets like art or music, and providing resources for support groups or counseling. Helping patients identify their strengths and develop positive coping strategies can enhance their resilience and ability to navigate through challenging times.
Supportive therapy and counseling
Therapeutic interventions, such as individual or group counseling, can provide a safe space for individuals with PMDD to express their emotions, develop coping skills, and gain insight into their condition. Supportive therapy can also help patients explore how PMDD affects their relationships and work towards building healthier interactions.

Educating and Empowering Patients
Providing information on PMDD
Patient education is crucial in raising awareness and understanding of PMDD. Nurses should provide accurate and comprehensive information about the condition, its symptoms, underlying causes, and available treatment options. They should also address any misconceptions or myths surrounding PMDD, empowering patients to make informed decisions about their care.
Discussing treatment options and goals
Engaging patients in discussions about their treatment options and goals is essential for shared decision-making. Nurses should explain the benefits and risks of different interventions and involve patients in the development of individualized treatment plans. By taking into account their preferences and needs, patients are more likely to adhere to their treatment regimen and experience positive outcomes.
Encouraging self-care practices
Self-care plays a crucial role in the management of PMDD. Nurses should encourage patients to prioritize their physical and emotional well-being by engaging in activities that promote relaxation, stress reduction, and overall self-care. This may include engaging in hobbies, practicing mindfulness or meditation, getting adequate sleep, and maintaining a healthy lifestyle.
Promoting self-advocacy
Empowering patients to become their own advocates is paramount. Nurses should provide guidance on how to effectively communicate with healthcare providers, ask questions, voice concerns, and actively participate in their care. By encouraging self-advocacy, nurses can help patients become actively involved in the decision-making process and take ownership of their health.
Monitoring and Follow-up
Regular assessment of symptom severity
Regular assessment of symptom severity is vital in monitoring the effectiveness of interventions and adjusting treatment plans, if necessary. Using standardized assessment tools, nurses can track the changes in symptoms over time, identify triggers, and evaluate the impact of various interventions. This allows for individualized and targeted care that addresses the specific needs of each patient.
Monitoring medication effectiveness and side effects
For patients on pharmacological interventions, monitoring the effectiveness of medications and potential side effects is crucial. Nurses should closely monitor patients’ response to treatment and report any adverse effects to the healthcare provider. This enables timely adjustments to the medication regimen to optimize symptom management while minimizing any potential risks.
Evaluation of treatment adherence
Ensuring treatment adherence is essential for achieving positive outcomes in PMDD management. Nurses can inquire about patients’ adherence to medications, non-pharmacological interventions, and self-care practices during follow-up appointments. By addressing barriers to adherence and providing additional support and education as needed, nurses can help patients stay on track with their treatment plan.
Ensuring appropriate follow-up care
Follow-up care is essential in the long-term management of PMDD. Nurses can schedule regular appointments to assess patients’ progress, provide ongoing education and support, and address any new concerns or challenges that may arise. Regular follow-up care ensures continuity of care and allows for adjustments to treatment plans based on the patient’s evolving needs.

Special Considerations for Adolescents
Unique challenges in diagnosing and managing PMDD in adolescents
Diagnosing and managing PMDD in adolescents can present unique challenges. Hormonal changes during puberty can complicate the assessment and diagnosis process, as symptoms of PMDD may overlap with typical mood swings and emotional changes associated with adolescence. It is important for healthcare professionals to carefully evaluate the timing and severity of symptoms in order to differentiate PMDD from normal developmental changes.
Communication strategies with adolescents
Effective communication is key when working with adolescents experiencing PMDD. Nurses should establish a trusting and non-judgmental relationship, allowing adolescents to openly share their experiences and concerns. Using age-appropriate language and providing information in a clear and concise manner can facilitate understanding and engagement in the treatment process.
Age-appropriate interventions
When developing interventions for adolescents with PMDD, it is important to consider their unique needs and preferences. Collaborating with the adolescent and their family, healthcare professionals can tailor treatment plans to align with the adolescent’s lifestyle and goals. Engaging adolescents in decision-making, promoting peer support, and providing resources specifically designed for this age group can enhance treatment outcomes and promote overall well-being.
Addressing Psychosocial Factors
Recognizing the impact of social and cultural factors on PMDD
Psychosocial factors, such as social and cultural influences, can significantly impact the experience and management of PMDD. Nurses should be aware of the potential stigma associated with mental health conditions and provide an empathetic and non-judgmental environment for patients to share their concerns. Understanding the sociocultural context allows for more comprehensive and culturally sensitive care.
Providing support and counseling for psychosocial stressors
Psychosocial stressors, such as relationship difficulties, work-related stress, or financial concerns, can exacerbate the symptoms of PMDD. Nurses can provide counseling and support, helping patients identify and develop coping strategies specific to their individual stressors. Referrals to social workers, counselors, or community resources can also be made to further support patients in addressing these stressors.
Referring patients to community resources
Patients with PMDD may benefit from additional support services available in the community. Nurses can provide information and referrals to support groups, online forums, and community organizations that specialize in mental health and women’s health. These resources can offer a sense of belonging, peer support, and access to additional educational materials and evidence-based interventions.
Involving family members in the care process
Family support is essential in the management of PMDD. Nurses can involve family members in the care process by providing education about PMDD, its impact on the patient, and strategies for support. Inclusion of family members in therapy sessions or family-centered interventions can facilitate communication, enhance understanding, and promote a supportive environment that contributes to the patient’s overall well-being.
In conclusion, the comprehensive care of patients with PMDD requires a holistic approach that encompasses pharmacological interventions, non-pharmacological interventions, patient education, and a collaborative care team. Nurses play a crucial role in the assessment, diagnosis, management, and support of individuals with PMDD. By providing person-centered care, empowering patients, and fostering collaboration among healthcare professionals, nurses can help individuals with PMDD effectively manage their symptoms, improve their quality of life, and thrive.