So you’ve come across the term ACL injuries, and you’re wondering what it means for nursing considerations and management? Well, look no further! This article will provide you with a concise overview of the nursing considerations and management strategies for ACL injuries. From understanding the anatomy of the ACL to recognizing the signs and symptoms of an injury, we’ve got you covered. So let’s dive in and explore the vital nursing insights into caring for patients with ACL injuries.

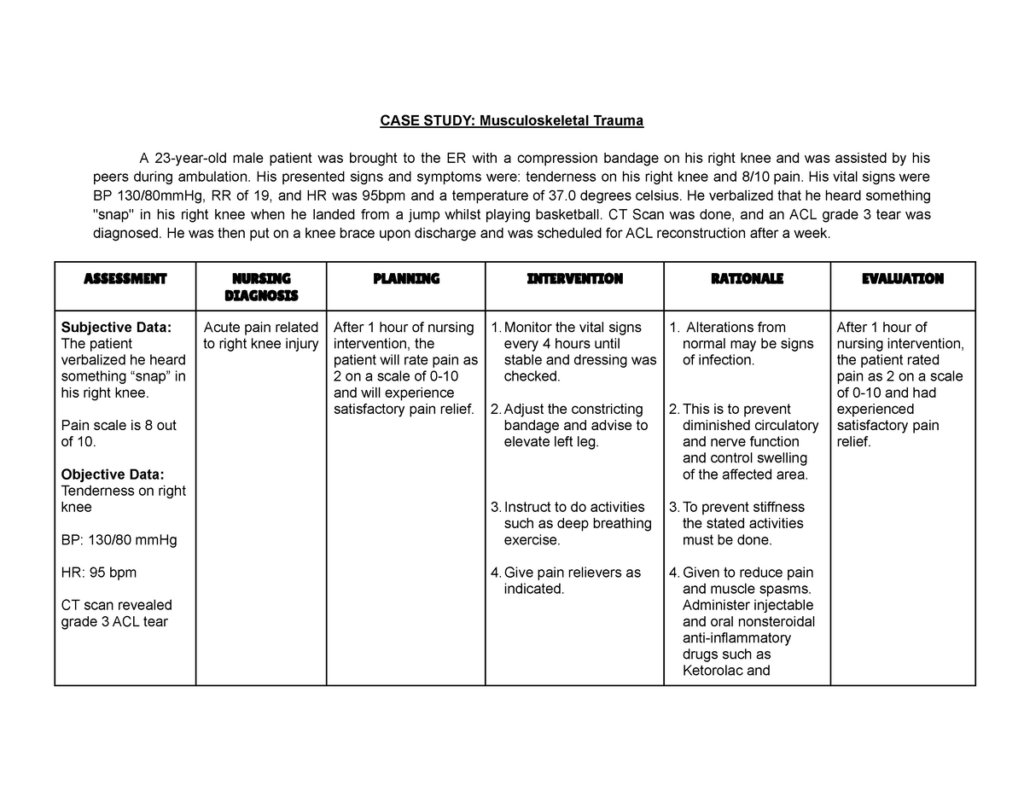
Assessment
When it comes to assessing a patient with an ACL injury, there are several key aspects to consider. The physical assessment involves examining the affected knee for signs of swelling, tenderness, and instability. It is important to assess the range of motion and perform special tests such as the Lachman test and pivot shift test to evaluate the integrity of the ACL. Additionally, obtaining a detailed patient history is essential in understanding the mechanism of injury, any previous knee issues, and identifying any underlying risk factors. Diagnostic tests, such as MRI or arthroscopy, may also be utilized to confirm the diagnosis and assess the extent of the injury.
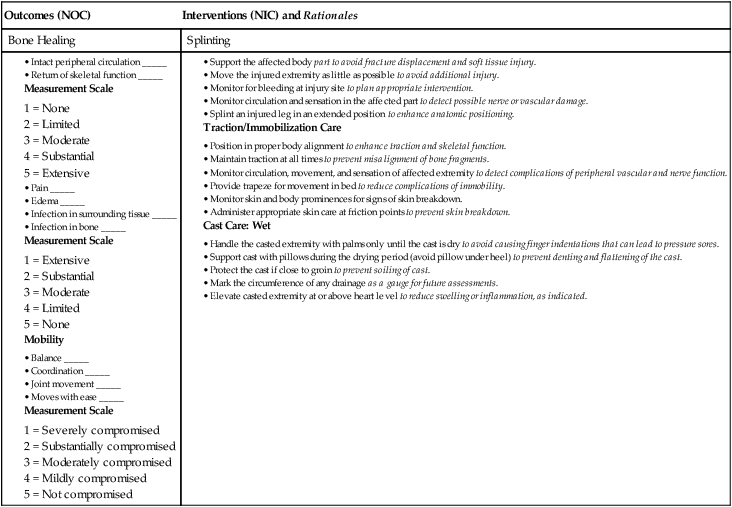
Initial management
Following an ACL injury, early management is crucial to reduce pain and prevent further damage. One of the most commonly recommended initial treatments is the RICE therapy: Rest, Ice, Compression, and Elevation. This helps reduce swelling, alleviate pain, and promote the healing process. Pain management is another essential aspect, and a healthcare provider may prescribe pain medication or recommend over-the-counter analgesics to help control pain. Immobilization of the knee joint, usually achieved through the use of a brace or splint, is often necessary to provide support and protect the injured ACL.
Surgical considerations
In some cases, surgical intervention may be necessary to repair or reconstruct the injured ACL. Preoperative care focuses on optimizing the patient’s overall health and preparing them for the procedure. This may involve ensuring that the patient is well-hydrated, obtaining necessary blood work and imaging studies, and providing education about the surgical process. Postoperative care involves closely monitoring the patient for any complications, such as infection or deep vein thrombosis (DVT). Wound care is essential to ensure proper healing of the surgical incisions, and specific instructions may be provided regarding dressing changes and signs of infection.
Rehabilitation
Rehabilitation plays a vital role in the overall management of ACL injuries. Early mobilization, under the guidance of a physical therapist, helps prevent joint stiffness and muscle atrophy. Range of motion exercises are gradually introduced to improve flexibility and gradually regain full knee function. As the healing progresses, strength training exercises are incorporated to rebuild the muscles surrounding the knee and provide stability. The rehabilitation process is usually tailored to each individual, taking into consideration factors such as the severity of the injury, patient age, and overall physical condition.

Medication management
Medication management for ACL injuries typically involves the use of non-steroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. NSAIDs work by inhibiting the production of prostaglandins, which are responsible for pain and swelling. Anticoagulant therapy may also be prescribed to prevent blood clots postoperatively. These medications help reduce the risk of deep vein thrombosis (DVT) that can occur due to decreased mobility after surgery. Analgesics, including opioids or non-opioid pain relievers, may be prescribed to manage pain during the recovery process.
Patient education
Providing comprehensive patient education is essential in managing ACL injuries effectively. Explaining the nature of the injury and the treatment options available helps patients understand their condition and make informed decisions about their healthcare. Management of symptoms, such as pain and swelling, should be thoroughly explained, including recommendations for proper RICE therapy and pain management techniques. Furthermore, patients need to be informed about the importance of follow-up care, including rehabilitation exercises, physical therapy appointments, and potential complications to watch for.
Psychosocial support
ACL injuries can have a significant emotional impact on patients. It is not uncommon for individuals to experience frustration, anxiety, and even depression as a result of the injury and the potential limitations it imposes. Providing psychosocial support is crucial in helping patients cope with these emotional challenges. Healthcare professionals can offer reassurance, empathy, and an open line of communication to address any concerns or fears the patient may have. Encouraging patients to utilize coping strategies, such as engaging in hobbies, seeking support from friends and family, or participating in counseling, can also be beneficial.
Complications
While managing ACL injuries, it is essential to be aware of potential complications that may arise. Infection is a possible complication, particularly after surgery, and it is crucial to closely monitor the surgical site for any signs of infection, such as redness, swelling, or discharge. Deep vein thrombosis (DVT), a blood clot that forms in the veins, is another complication to be vigilant about. Patients should be educated about the signs and symptoms of DVT, such as leg pain, swelling, and warmth, to seek prompt medical attention if necessary. Joint stiffness is also a complication that can occur if rehabilitation measures are not diligently followed, and patients should be encouraged to adhere to their rehabilitation program to prevent this.
Prevention and risk reduction
Prevention and risk reduction are essential components of managing ACL injuries. Educating patients about proper technique during physical activities, such as using appropriate body mechanics and avoiding sudden twists or pivots, can help reduce the risk of ACL injuries. The use of protective gear, such as knee braces or padding, can provide added support and potentially decrease the risk of injury. Additionally, promoting and maintaining a healthy lifestyle is crucial, as maintaining a healthy weight and engaging in regular exercise can strengthen muscles and reduce the risk of knee injuries.
Collaborative care
ACL injuries often require a multidisciplinary approach to ensure comprehensive care. Collaborating with physical therapists and referring patients for physical therapy is crucial in helping patients regain strength, mobility, and function. Orthopedic consultation may also be necessary in cases where surgical intervention is required or if there are complex factors contributing to the injury. A collaborative approach involving nurses, physicians, therapists, and other healthcare professionals ensures that patients receive the best possible care and support throughout their ACL injury journey.
In conclusion, the nursing considerations and management for ACL injuries involve a holistic approach encompassing assessment, initial management, surgical considerations, rehabilitation, medication management, patient education, psychosocial support, complications prevention, and collaborative care. By focusing on each of these aspects, healthcare professionals can provide optimal care and support to individuals who have experienced an ACL injury, helping them recover and regain their quality of life.
