Acute renal failure can be a challenging condition for patients and their healthcare providers alike. As a nurse, it is essential to have a thorough understanding of the nursing considerations and management strategies necessary for providing optimal care for patients with this condition. This article aims to provide a concise yet comprehensive overview of the key nursing considerations and management techniques that can help nurses navigate the complexities of acute renal failure. From assessing renal function to implementing appropriate interventions, this article will equip you with the knowledge and skills needed to deliver high-quality care to patients with acute renal failure.
Assessment
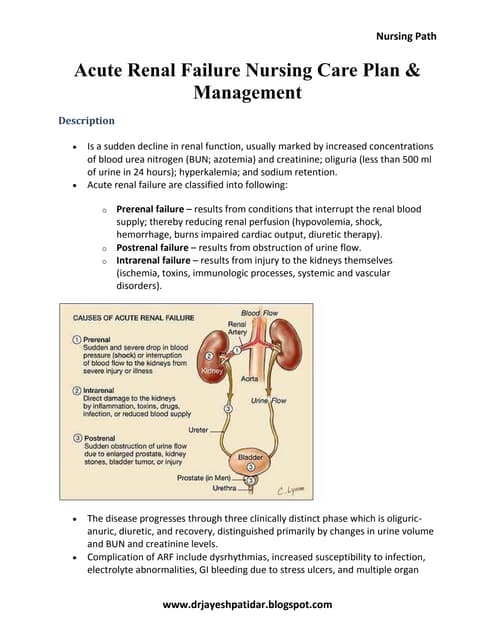
Identifying risk factors
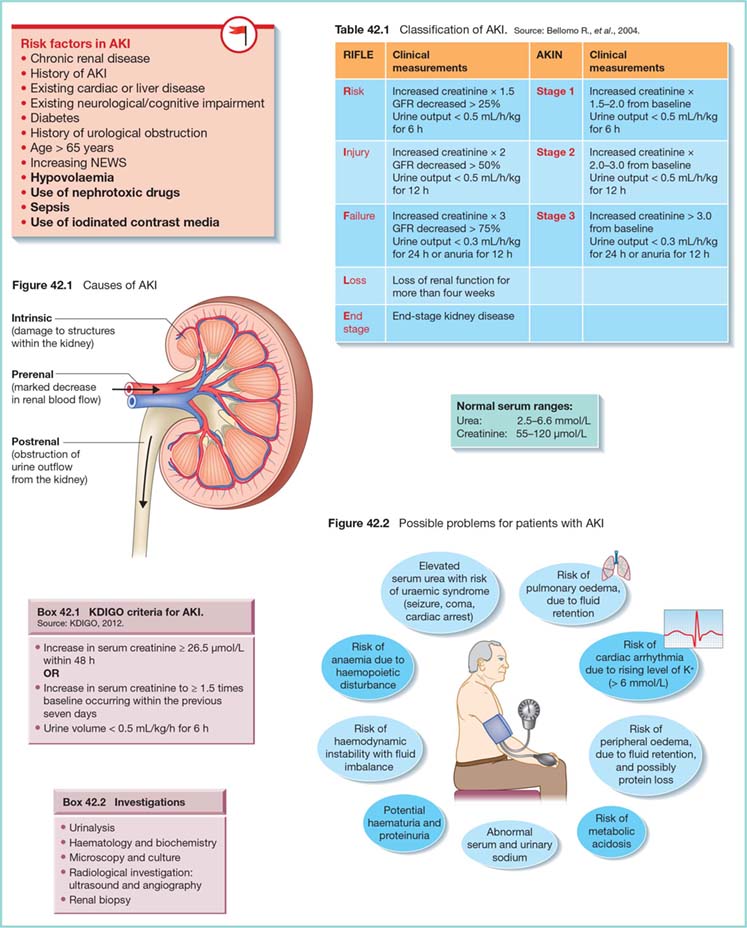
In order to effectively manage and treat acute renal failure, it is important to first identify the risk factors that may contribute to the development of the condition. These risk factors can include conditions such as diabetes, hypertension, heart failure, liver disease, and certain medications like nonsteroidal anti-inflammatory drugs (NSAIDs). By identifying these risk factors, healthcare professionals can take proactive measures to prevent the onset of acute renal failure or intervene early to minimize the damage.
Assessing symptoms
When assessing a patient for acute renal failure, it is crucial to pay close attention to the signs and symptoms that may indicate the presence of the condition. Common symptoms of acute renal failure include decreased urine output, fluid retention, fatigue, nausea, and confusion. Additionally, a physical examination may reveal swelling, particularly in the lower extremities or around the eyes. By carefully assessing these symptoms, healthcare professionals can make an accurate diagnosis and determine the appropriate treatment plan.
Collecting medical history
Collecting the patient’s medical history is an essential part of the assessment process for acute renal failure. This includes gathering information about any pre-existing conditions, prior episodes of kidney dysfunction, and medications taken regularly. Additionally, it is important to inquire about any recent exposure to nephrotoxic substances or any recent surgical procedures that may have contributed to the development of acute renal failure. By obtaining a comprehensive medical history, healthcare professionals can better understand the potential underlying causes of the condition and tailor the treatment accordingly.
Obtaining vital signs
Obtaining accurate vital signs is crucial for assessing and monitoring patients with acute renal failure. Key vital signs to monitor include blood pressure, heart rate, respiratory rate, and temperature. Changes in blood pressure can indicate fluid imbalance, while an irregular heart rate may suggest electrolyte imbalances. Regular monitoring of vital signs can help healthcare professionals identify any trends or abnormalities that may require immediate intervention or adjustments to the treatment plan.
Performing physical examination
A thorough physical examination is a vital component of the assessment for acute renal failure. During the examination, healthcare professionals will assess the patient’s overall appearance, looking for any signs of edema, jaundice, or abnormal skin coloration. Special attention is given to the cardiovascular and respiratory systems, as well as the abdomen, to check for any abnormalities that may be associated with acute renal failure. By performing a comprehensive physical examination, healthcare professionals can detect any potential complications or underlying conditions that may be contributing to the patient’s renal dysfunction.
Diagnostic Tests
Urinalysis
Urinalysis is a valuable diagnostic tool for assessing and monitoring patients with acute renal failure. It involves analyzing a urine sample to evaluate various components, including the presence of blood, protein, and other substances. Abnormal findings in a urinalysis, such as the presence of red blood cells or proteinuria, can indicate kidney dysfunction and help guide the treatment plan. Additionally, urinalysis can provide information about kidney function, including the urine specific gravity and osmolality. Regular monitoring of urinalysis results can help healthcare professionals evaluate the effectiveness of interventions and adjust the treatment plan accordingly.
Blood tests
Blood tests are essential for diagnosing and monitoring patients with acute renal failure. These tests measure various components in the blood, including creatinine and blood urea nitrogen (BUN) levels. Elevated creatinine and BUN levels can indicate impaired kidney function and the accumulation of waste products in the blood. Additionally, blood tests can assess electrolyte imbalances, such as elevated potassium levels, which may require immediate intervention. Regular monitoring of blood tests, including complete blood count and electrolyte panel, is crucial for managing and treating acute renal failure effectively.
Ultrasound
Ultrasound imaging is a non-invasive diagnostic tool that can provide valuable information about the structure and function of the kidneys. It can help identify any anatomical abnormalities or obstructions that may be contributing to acute renal failure. Additionally, ultrasound can assess the size, shape, and blood flow to the kidneys. This information can help guide the treatment plan and determine the appropriate interventions for the patient. Ultrasound is a safe and effective diagnostic tool that can be used throughout the course of acute renal failure to monitor changes and evaluate the response to treatment.
Renal biopsy
In some cases, a renal biopsy may be necessary to diagnose and manage acute renal failure. This procedure involves obtaining a small sample of kidney tissue for examination under a microscope. A renal biopsy can provide valuable information about the underlying cause of renal dysfunction, such as glomerulonephritis or acute tubular injury. It can also help assess the severity of kidney damage and guide the treatment plan. Renal biopsies are typically performed by interventional radiologists or nephrologists and require close monitoring of the patient during and after the procedure.
Fluid and Electrolyte Balance
Monitoring intake and output
Monitoring a patient’s fluid intake and output is essential for managing fluid and electrolyte balance in acute renal failure. This involves accurately measuring and documenting all fluids consumed and excreted by the patient. Monitoring intake includes measuring oral fluids, intravenous fluids, and any other sources of fluid intake. Assessment of output includes measuring urine output, as well as monitoring any other fluid losses, such as through diarrhea or vomiting. By closely monitoring intake and output, healthcare professionals can ensure that the patient’s fluid balance is optimized and adjust interventions accordingly.
Assessing fluid status
Assessing a patient’s fluid status is critical for managing acute renal failure effectively. Healthcare professionals assess factors such as skin turgor, mucous membranes, and edema to determine if the patient is adequately hydrated or experiencing fluid overload. Additionally, weight measurement is an important indicator of fluid status, as sudden weight gain can suggest fluid retention. Regular assessment of fluid status helps healthcare professionals identify any imbalances and make appropriate adjustments to the patient’s fluid management plan.
Managing fluid replacement
In acute renal failure, managing fluid replacement is crucial to optimize the patient’s fluid balance and prevent complications such as fluid overload or dehydration. Depending on the patient’s specific needs, fluid replacement may involve intravenous fluids, oral rehydration solutions, or diuretics to promote diuresis. Healthcare professionals carefully titrate fluid replacement therapy based on the patient’s fluid status, vital signs, and laboratory values. Regular monitoring and adjustment of fluid replacement ensure that the patient’s fluid balance is maintained within the desired range.
Maintaining electrolyte balance
Maintaining electrolyte balance is essential in managing acute renal failure as imbalances can lead to significant complications. Healthcare professionals monitor and manage electrolyte levels such as sodium, potassium, calcium, and phosphorus to prevent abnormalities in the body. This may involve adjusting the patient’s diet, administering electrolyte supplements, or using medications to correct imbalances. Regular monitoring of electrolyte levels through blood tests ensures that any abnormalities are promptly identified and remedied, promoting optimal kidney function.
Nutritional Support
Assessing nutritional needs
Assessing the patient’s nutritional needs is crucial for managing acute renal failure effectively. Impaired kidney function can affect the patient’s ability to adequately metabolize nutrients, leading to malnutrition. Healthcare professionals evaluate the patient’s dietary intake, weight loss, and laboratory values to determine their nutritional status. This assessment helps identify any deficiencies or excesses in nutrients and guides the development of an individualized nutritional plan.
Monitoring dietary intake
Regular monitoring of the patient’s dietary intake is essential in managing acute renal failure. Healthcare professionals closely monitor the patient’s food choices and portion sizes to ensure that they are receiving the appropriate balance of nutrients. In many cases, dietary restrictions may be necessary to manage electrolyte imbalances or reduce the workload on the kidneys. Regular monitoring of dietary intake helps ensure that the patient’s nutritional needs are being met and that any necessary modifications are made promptly.
Collaborating with dietitian
Collaboration with a dietitian is essential in managing the nutritional support of patients with acute renal failure. Dietitians specialize in assessing nutritional needs and developing individualized meal plans that meet the patient’s specific requirements. They can provide information on dietary modifications, portion control, and substitution of high-protein foods. Collaborating with the dietitian ensures that the patient’s nutritional needs are accurately assessed and effectively addressed, promoting optimal recovery and preventing complications.
Administering enteral or parenteral nutrition
In some cases, enteral or parenteral nutrition may be necessary to meet the patient’s nutritional needs during acute renal failure. Enteral nutrition involves administering nutrients directly into the gastrointestinal tract, usually through a feeding tube, while parenteral nutrition involves administering nutrients intravenously. Healthcare professionals carefully assess the patient’s ability to tolerate enteral nutrition and select the appropriate formulation based on their specific needs. If enteral nutrition is not feasible or contraindicated, parenteral nutrition may be initiated under close monitoring and with the guidance of a nutrition support team.

Medication Administration
Administering diuretics
Diuretics play a crucial role in managing fluid overload and promoting diuresis in patients with acute renal failure. Healthcare professionals assess the patient’s fluid status, electrolyte levels, and renal function before initiating diuretic therapy. The selection and administration of diuretics are tailored to the individual patient’s needs, considering factors such as the type of diuretic, route of administration, and potential side effects. Regular monitoring of urine output, electrolyte levels, and vital signs helps evaluate the effectiveness of diuretic therapy and guide dosage adjustments.
Managing electrolyte imbalances
Electrolyte imbalances are common in acute renal failure and require careful management to prevent complications. Healthcare professionals closely monitor electrolyte levels, particularly potassium, sodium, and calcium, and take appropriate measures to correct any imbalances. This may involve dietary modifications, medication administration, or the temporary restriction of certain electrolyte-rich foods. Regular monitoring of electrolyte levels through blood tests helps guide the management of imbalances and ensures the patient’s safety and well-being.
Providing appropriate pain management
Patients with acute renal failure may experience pain as a result of their condition, underlying causes, or interventions. Healthcare professionals assess the patient’s pain level, location, and quality to determine the most appropriate pain management strategies. This may involve the administration of analgesic medications, such as non-opioid or opioid pain relievers, as well as non-pharmacological interventions, like heat or cold therapy. Regular assessment of pain levels ensures that appropriate and timely pain relief is provided, promoting patient comfort and well-being.
Administering antibiotics or immunosuppressants
In some cases, acute renal failure may be due to infections or autoimmune conditions that require treatment with antibiotics or immunosuppressants. Healthcare professionals closely monitor the patient’s clinical and laboratory findings to determine the need for these medications. Antibiotics are administered to treat bacterial infections, while immunosuppressants are used to manage autoimmune conditions. Close monitoring of the patient’s response to these medications and regular laboratory tests ensure the effectiveness of treatment and minimize the risk of adverse reactions.
Fluid Restriction
Educating the patient about fluid restriction
In cases where fluid overload is a concern, healthcare professionals provide education and counseling to patients about fluid restriction. They explain the importance of adhering to prescribed fluid limits and provide practical strategies to help patients manage their fluid intake effectively. Education may include providing information about low-liquid or liquid-consistency diets, the use of small serving sizes, and alternative ways to manage thirst. Clear and concise communication about fluid restriction helps patients understand the rationale behind the recommendations and encourages active participation in their care.
Monitoring and documenting fluid intake
Accurate monitoring and documentation of fluid intake are essential in managing fluid restriction effectively. Healthcare professionals record all fluids consumed by the patient, including oral intake, intravenous fluids, and any other sources of fluid. This documentation helps ensure that the patient’s fluid intake remains within the prescribed limits and provides a record for the healthcare team to evaluate trends and adjust the care plan accordingly. Regular monitoring and documentation of fluid intake enhance patient safety and contribute to the overall management of acute renal failure.
Assessing for signs of dehydration
While fluid restriction is important, it is equally crucial to monitor for signs of dehydration in patients with acute renal failure. Healthcare professionals assess vital signs, skin turgor, oral mucous membranes, and urine output to evaluate the patient’s hydration status. Additionally, they monitor laboratory parameters like serum electrolyte levels and urine specific gravity. Regular assessment for signs of dehydration allows healthcare professionals to promptly intervene and adjust the fluid management plan to maintain the patient’s fluid balance appropriately.
Implementing strategies to promote adherence to fluid restrictions
Promoting adherence to fluid restrictions can be challenging for patients with acute renal failure. Healthcare professionals work closely with patients to develop strategies that help them manage their fluid intake effectively. These strategies may include providing educational materials, encouraging the use of portion control tools, and involving family members or caregivers in monitoring and supporting the patient’s fluid restriction efforts. By collaborating with patients and involving them in their care, healthcare professionals can enhance patient engagement and support successful adherence to fluid restrictions.
Hemodialysis or Continuous Renal Replacement Therapy (CRRT)
Preparing the patient for hemodialysis/CRRT
Hemodialysis and continuous renal replacement therapy (CRRT) are advanced treatment modalities often used in patients with acute renal failure who require more intensive kidney support. Healthcare professionals play a critical role in preparing the patient for these procedures. They explain the purpose and process of hemodialysis or CRRT, address any concerns or questions the patient may have, and obtain informed consent. Preparations may also include assessing vascular access sites for hemodialysis, ensuring the presence of necessary equipment, and coordinating with the interdisciplinary team to optimize patient outcomes.
Monitoring the patient during the treatment
Continuous monitoring of the patient during hemodialysis or CRRT is essential to ensure the treatment’s safety and effectiveness. Healthcare professionals assess vital signs, fluid status, and any signs of complications throughout the procedure. They closely monitor the function of the hemodialysis or CRRT machine, blood flow rates, and the removal of waste products. Monitoring also includes evaluating the patient’s comfort, addressing any adverse reactions or symptoms, and ensuring proper infection control measures are followed. Continuous monitoring helps healthcare professionals identify any deviations from the expected outcomes and take timely interventions as needed.
Assessing vascular access site
Hemodialysis requires vascular access, usually through an arteriovenous fistula, graft, or central venous catheter. Proper assessment and monitoring of the vascular access site are essential to prevent complications such as infection or thrombosis. Healthcare professionals assess the site for the presence of redness, swelling, pain, or any signs of infection. They also evaluate the patency of the access, the adequacy of blood flow rates, and the functionality of the dialysis or CRRT machine. Regular assessment of the vascular access site helps ensure its optimal function and minimizes the risk of complications.
Administering medications during hemodialysis/CRRT
During hemodialysis or CRRT, medication administration requires special attention as the clearance of certain medications might be affected. Healthcare professionals carefully review the patient’s medication list and consult pharmacists or nephrologists to ensure compatibility with the dialysis or CRRT procedure. Medications that need to be adjusted or withheld during the procedure are identified, and appropriate interventions are implemented. Regular assessment and documentation of medication administration during hemodialysis or CRRT help ensure patient safety and optimize therapeutic outcomes.
Prevention of Infection
Promoting hand hygiene
Hand hygiene is a fundamental infection prevention measure in managing acute renal failure. Healthcare professionals ensure that rigorous hand hygiene protocols are followed, including proper handwashing with soap and water or using alcohol-based hand sanitizers. They educate patients, family members, and other healthcare providers about the importance of hand hygiene in preventing the spread of infections. Consistent promotion of hand hygiene practices helps reduce the risk of healthcare-associated infections and protects the well-being of patients and healthcare providers alike.
Educating the patient about infection prevention
Healthcare professionals play a crucial role in educating patients about infection prevention strategies. They provide information on personal hygiene practices, such as proper hand hygiene, respiratory hygiene, and wound care techniques. Patients are educated about the signs and symptoms of infection and advised to report any concerning changes promptly. Additionally, patients are encouraged to adhere to infection control measures, such as following isolation precautions and completing prescribed antibiotic regimens. By empowering patients with knowledge, healthcare professionals promote active involvement in their care and help prevent the occurrence of infection.
Maintaining sterile technique for procedures
Maintaining a sterile technique is essential for preventing infections in patients with acute renal failure. Healthcare professionals adhere to strict aseptic practices when performing invasive procedures, such as dressing changes, catheter insertions, or renal biopsies. This includes wearing sterile gloves, using sterile equipment, and following proper hand hygiene protocols. Regular reinforcement of sterile technique principles and ongoing education of healthcare providers help ensure that a safe and clean environment is maintained during these procedures.
Initiating appropriate isolation precautions
Initiating appropriate isolation precautions is crucial for preventing the transmission of infections in patients with acute renal failure. Healthcare professionals accurately assess the patient’s risk of infection and implement the necessary measures to prevent the spread of pathogens. This may include placing the patient in a private room, using personal protective equipment (PPE), such as gloves and masks, and following specific protocols for handling contaminated materials. Compliance with isolation precautions helps protect vulnerable patients, staff, and visitors from acquiring and spreading infections.
Psychosocial Support
Assessing for emotional distress
Providing psychosocial support to patients with acute renal failure requires assessing for signs of emotional distress. Healthcare professionals regularly assess the patient’s emotional well-being, including their mood, anxiety levels, coping strategies, and social support systems. They use appropriate assessment tools and communication techniques to identify any psychological or emotional challenges the patient may be facing. Identifying emotional distress helps healthcare professionals tailor their support interventions and refer the patient to appropriate resources, such as counseling services or support groups.
Providing counseling and emotional support
Counseling and emotional support are essential components of psychosocial care for patients with acute renal failure. Healthcare professionals provide therapeutic communication, active listening, and empathy to address the patient’s emotional needs. They offer reassurance, validation, and encouragement to help patients cope with the challenges associated with their diagnosis and treatment. Healthcare professionals also involve the patient’s family members or caregivers in counseling sessions, as they play a vital role in providing emotional support and assisting with the patient’s recovery.
Collaborating with the interdisciplinary team
Collaboration with the interdisciplinary team is crucial in providing comprehensive psychosocial support for patients with acute renal failure. Healthcare professionals work closely with social workers, psychologists, psychiatrists, and other healthcare providers to address the patient’s emotional and psychological needs. They engage in regular team meetings, case conferences, and interprofessional communication to ensure coordinated and holistic care. Collaboration with the interdisciplinary team enhances the effectiveness of psychosocial interventions and promotes positive patient outcomes.
Facilitating communication with the patient’s family
Facilitating effective communication with the patient’s family is vital in providing psychosocial support during acute renal failure. Healthcare professionals actively involve family members in the patient’s care, providing updates on the patient’s condition, treatment plan, and progress. They offer emotional support, answer questions, and address any concerns or fears the family may have. Regular communication helps foster trust, ensures the family’s active participation in the patient’s care, and provides the necessary support network for the patient’s recovery.
Monitoring and Evaluation
Monitoring renal function
Close monitoring of renal function is essential in managing acute renal failure. Healthcare professionals regularly assess laboratory parameters such as serum creatinine, blood urea nitrogen (BUN), and urine output to evaluate kidney function. They also monitor signs and symptoms that may indicate improvement or deterioration in renal function, such as changes in urine color or volume. By regularly monitoring renal function, healthcare professionals can identify any changes or trends that may require modifications to the treatment plan.
Assessing for improvement or worsening of symptoms
Regular assessment of the patient’s symptoms is crucial for evaluating the effectiveness of interventions during the management of acute renal failure. Healthcare professionals monitor the patient’s vital signs, fluid status, and urine output to assess for improvement or worsening of symptoms. They also closely observe for any signs or symptoms of complications that may occur as a result of the disease or its treatment. By assessing for improvement or deterioration of symptoms, healthcare professionals can make timely adjustments to the care plan and ensure optimal outcomes for the patient.
Evaluating the effectiveness of interventions
Evaluating the effectiveness of interventions is essential in managing acute renal failure. Healthcare professionals regularly assess the patient’s response to treatment, including laboratory parameters, vital signs, and fluid balance. They evaluate whether the interventions implemented are achieving the desired outcomes, such as improved renal function, stable fluid and electrolyte balance, and resolution of complications. Regular evaluation of interventions helps guide further decision-making and allows for modifications to the care plan as necessary.
Modifying the care plan as needed
Modifying the care plan as needed is a crucial aspect of managing acute renal failure. Healthcare professionals continuously reassess the patient’s condition, response to treatment, and evolving needs to make informed decisions about care. Modifications to the care plan may involve adjustments in medication dosages, fluid management strategies, or dietary recommendations. Regular communication and collaboration with the interdisciplinary team ensure that modifications to the care plan are implemented safely and effectively to optimize patient outcomes.
In conclusion, the nursing considerations and management of acute renal failure encompass a comprehensive assessment, diagnostic tests, fluid and electrolyte balance, nutritional support, medication administration, fluid restriction, hemodialysis or CRRT, prevention of infection, psychosocial support, and ongoing monitoring and evaluation. Through a patient-centered and interdisciplinary approach, healthcare professionals can effectively manage acute renal failure, promote optimal recovery, and enhance the overall well-being of patients.