Hey there! Want to learn about the important nursing considerations for managing celiac disease? Well, you’ve come to the right place! In this article, we’ll be discussing the key aspects and strategies that nurses should keep in mind when caring for patients with celiac disease. From understanding the basics of this autoimmune condition to providing effective education and support, we’ve got you covered. So, let’s dive in and explore how nurses can play a crucial role in promoting the well-being of individuals living with celiac disease.
Diagnostic Considerations
Confirming the Diagnosis
When it comes to celiac disease, confirming the diagnosis is crucial to ensure appropriate management and treatment. As a nurse, you play an integral role in this process. The first step is to carefully assess the patient’s medical history, paying close attention to symptoms such as chronic diarrhea, weight loss, abdominal pain, and fatigue. Additionally, it is important to inquire about family history, as celiac disease has a strong genetic component.
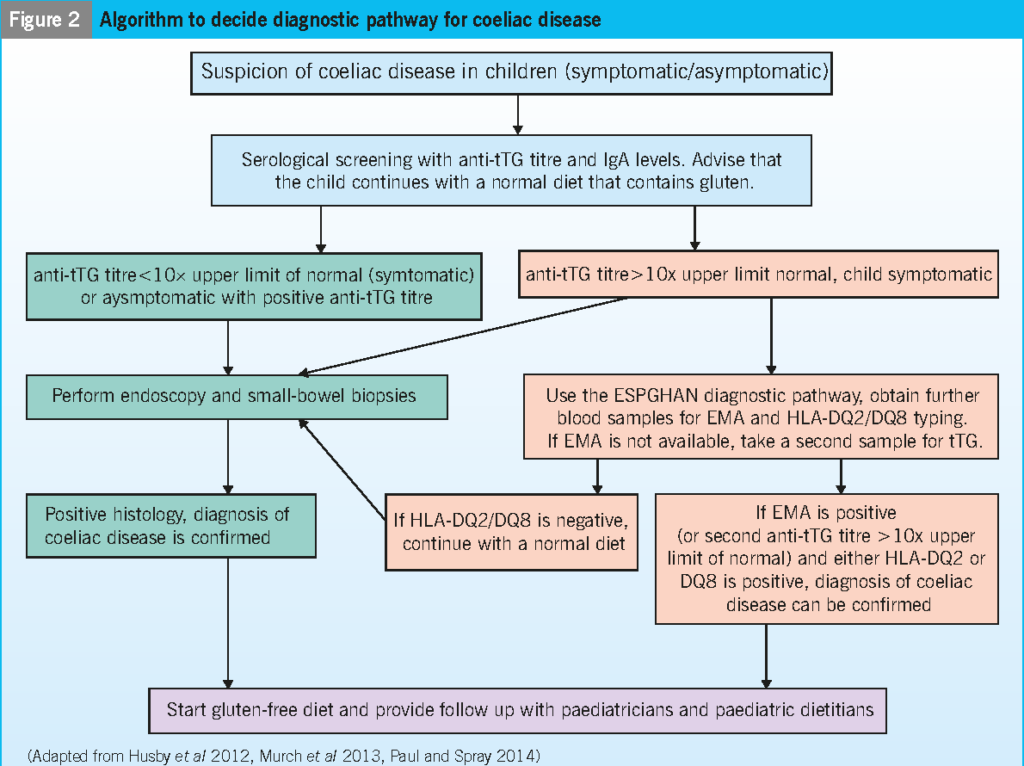
After a thorough history assessment, laboratory tests can be used to confirm the diagnosis. Serologic testing for celiac disease-specific antibodies, such as anti-tissue transglutaminase (TTG) and anti-endomysial antibodies (EMA), can be conducted. These tests are highly sensitive and specific for celiac disease. However, it is important to note that a small percentage of individuals with celiac disease may have negative serologic tests, highlighting the need for further diagnostic evaluation.
To definitively confirm the diagnosis, an intestinal biopsy is often performed. This involves obtaining a small tissue sample from the small intestine during an endoscopy procedure. The biopsy will reveal characteristic histologic changes in the intestinal lining, such as villous atrophy and increased intraepithelial lymphocytes, which are consistent with celiac disease.
Differentiating Celiac Disease from Other Conditions
Celiac disease can present with symptoms that overlap with other gastrointestinal disorders, making it essential to differentiate it from similar conditions. Conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and non-celiac gluten sensitivity (NCGS) may have similar symptoms but require different management approaches.
To differentiate celiac disease from other conditions, a comprehensive assessment is crucial. It is important to consider the patient’s clinical presentation, medical history, and diagnostic test results. Laboratory tests for celiac-specific antibodies should be interpreted in the context of the patient’s symptoms and biopsy findings. Collaboration with gastroenterologists and other healthcare professionals is vital to ensure an accurate diagnosis.
Nutritional Considerations
Educating on Gluten-Free Diet
Once the diagnosis of celiac disease is confirmed, educating the patient about a lifelong gluten-free diet becomes a key nursing consideration. As a nurse, you have the opportunity to provide essential education and support to help patients navigate the challenges of following a gluten-free lifestyle.
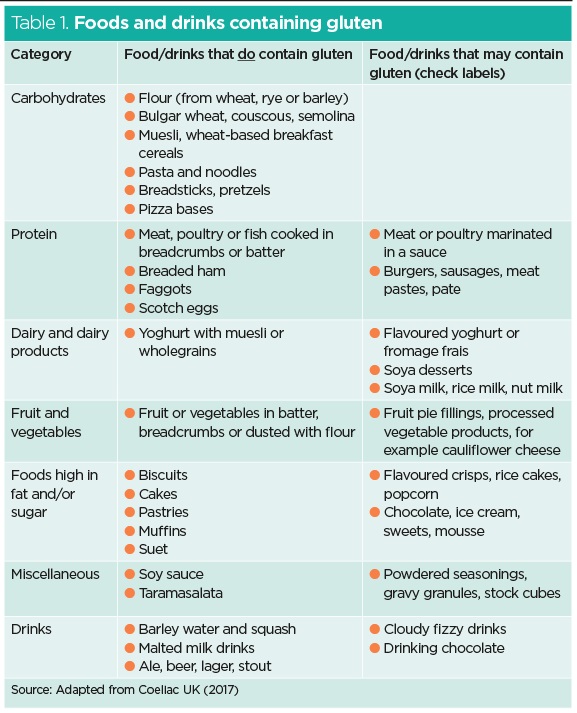
Start by explaining the concept of gluten and its presence in various food products. Illustrate the importance of avoiding gluten-containing grains like wheat, barley, and rye, as well as processed foods that may contain hidden sources of gluten. Emphasize the need for careful label reading and the importance of selecting certified gluten-free products.
Monitoring Nutritional Intake
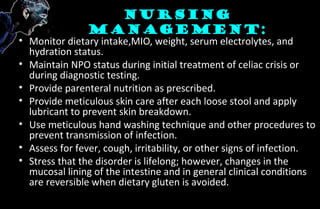
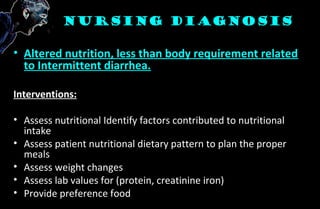
Following a gluten-free diet can pose challenges in meeting nutritional needs. The exclusion of gluten-containing grains may lead to a deficiency in essential nutrients such as fiber, iron, calcium, and B vitamins. To ensure optimal nutritional status, it is crucial to monitor the patient’s nutritional intake and provide guidance on appropriate substitutions.
Collaborating with a registered dietitian can be immensely helpful in creating a personalized meal plan that meets the patient’s specific dietary needs. Regular follow-ups with the dietitian can address any concerns and help monitor the patient’s overall nutrition.
Supplementation and Deficiencies
In some cases, despite efforts to maintain a well-balanced gluten-free diet, patients with celiac disease may still experience nutrient deficiencies. This can be due to impaired nutrient absorption in the damaged intestines or inadequate dietary intake. As a nurse, you should monitor for common deficiencies such as iron, calcium, vitamin D, and vitamin B12.
Supplementation may be necessary to address deficiencies and optimize overall health. Collaborate with the healthcare team, including the dietitian, to determine appropriate supplementation based on the patient’s specific needs and laboratory results.
Importance of a Balanced Diet
Encourage patients to focus on maintaining a balanced diet even while following a gluten-free lifestyle. Emphasize the inclusion of a variety of fruits, vegetables, lean proteins, and gluten-free grains such as quinoa, rice, and corn. A balanced diet helps ensure the intake of essential nutrients and promotes overall health and well-being.
Medication Administration
Ensuring Gluten-Free Medication
In addition to dietary considerations, it is important to address medication administration in patients with celiac disease. Many medications may contain gluten as an excipient or filler, which can potentially lead to gluten exposure and adverse reactions in susceptible individuals. As a nurse, you play a critical role in ensuring the safety of medication administration.
Thoroughly review the medication list of patients with celiac disease and identify any medications that may contain gluten. Consult with the pharmacist and healthcare team to identify suitable gluten-free alternatives or compounded medications when necessary.
Assessing for Potential Medication Interactions
When managing patients with celiac disease, it is essential to consider potential medication interactions. The damaged intestinal lining in celiac disease can affect the absorption and metabolism of certain medications. This can lead to altered drug efficacy or increased risk of adverse effects.
As a nurse, be vigilant in assessing for potential drug interactions and adverse effects. Collaborate with the healthcare team to monitor medication effectiveness and make any necessary adjustments to the treatment plan.
Administering Medications on Schedule
Consistency in medication administration is crucial in the management of celiac disease. Encourage patients to adhere to their medication schedule and emphasize the importance of taking medications as prescribed.
Supporting patients in adhering to their medication regimen includes providing education on proper administration techniques, setting reminders, and addressing any barriers or concerns they may have. Regular communication with the healthcare team and providing follow-up care can help ensure optimal medication management.
Psychosocial Support
Addressing Emotional Impact
A diagnosis of celiac disease can have a significant emotional impact on patients. The lifestyle changes required, the potential for social isolation, and the limitations associated with following a gluten-free diet can lead to feelings of frustration, sadness, and anxiety.
As a nurse, it is important to address the emotional well-being of patients with celiac disease. Provide a supportive and non-judgmental environment where patients can express their concerns and fears. Offer resources such as counseling services, support groups, or online communities to help patients connect with others facing similar challenges.
Supporting Lifestyle Modifications
Managing celiac disease involves making significant lifestyle modifications. This may include changes in eating habits, meal planning, and navigating social situations that involve food. As a nurse, you can provide guidance and support to help patients adapt to these changes successfully.
Offer practical tips for dining out, traveling, and attending social events while adhering to a gluten-free diet. Educate patients on how to communicate their dietary needs effectively and confidently. By empowering patients with the necessary tools and knowledge, you can help them navigate these challenges more effectively.
Connecting to Support Groups
Support groups can play a crucial role in the management of celiac disease. These groups provide a platform for patients to share experiences, exchange tips, and receive emotional support from individuals facing similar challenges. As a nurse, you can facilitate the connection between patients and local support groups or online communities.
Encourage patients to join support groups and participate in forums or discussions, where they can learn from others who have successfully managed celiac disease. This sense of community can be invaluable in providing emotional support and promoting successful long-term management.
Patient Education
Explaining Celiac Disease
As a nurse, providing accurate and comprehensive education about celiac disease is essential. By explaining the disease process, you can help patients understand the impact of gluten on their bodies and the importance of strict adherence to a gluten-free diet.
Begin by providing a simplified explanation of celiac disease, highlighting the autoimmune nature of the condition and the resulting damage to the small intestine. Emphasize that celiac disease is a lifelong condition that requires continuous management to prevent complications.
Providing Detailed Dietary Guidelines
The cornerstone of managing celiac disease is adherence to a strict gluten-free diet. Patients must be educated on which foods to avoid and provided with detailed dietary guidelines to help them make informed food choices. Collaborate with a registered dietitian to ensure accuracy and to provide personalized guidelines based on the patient’s specific needs.
Illustrate the importance of reading food labels carefully, as gluten can be found in unexpected sources such as sauces, seasonings, and processed foods. Provide a list of gluten-containing grains to avoid and suggest suitable alternatives. Offer resources such as cookbooks, recipe websites, and smartphone apps that can help patients find gluten-free options.
Recognizing and Managing Symptoms
Help patients recognize the common symptoms associated with celiac disease and understand the importance of prompt management. Symptoms such as gastrointestinal discomfort, malabsorption, fatigue, and weight loss should be reported to the healthcare team for appropriate evaluation and treatment.
Educate patients on potential gluten exposure sources and guide them on how to manage accidental ingestion. Discuss strategies for symptom management, such as over-the-counter medications for gastrointestinal discomfort or consulting with the healthcare team for further evaluation.
Importance of Regular Follow-ups
Regular follow-up appointments are essential for monitoring the patient’s progress, assessing nutritional needs, and addressing any concerns or questions. Emphasize the importance of attending scheduled appointments with healthcare providers, including gastroenterologists, dietitians, and other specialists.
During follow-up visits, patients may undergo laboratory tests, such as checking celiac-specific antibodies, to monitor disease activity and nutritional status. Serologic tests can help assess adherence to the gluten-free diet and aid in identifying potential exposure to gluten.
Monitoring for Complications
Assessing for Nutritional Deficiencies
Due to the impaired absorption of nutrients in celiac disease, patients may be at increased risk for nutritional deficiencies. Regular monitoring of key nutrient levels is crucial to identify deficiencies early and intervene appropriately.
Collaborate with the healthcare team to ensure that patients undergo periodic laboratory tests to assess nutrient levels. Pay particular attention to iron, calcium, vitamin D, and vitamin B12, as these are commonly affected by malabsorption in celiac disease.
Screening for Associated Autoimmune Disorders
Celiac disease is associated with an increased risk of developing other autoimmune disorders, such as type 1 diabetes, autoimmune thyroid disease, and autoimmune liver disease. Regular screening and monitoring for these conditions are essential to ensure early detection and appropriate management.
Work closely with healthcare providers to develop a comprehensive screening plan based on the patient’s individual risk factors and medical history. This may involve periodic blood tests, imaging studies, or referrals to specialists for further evaluation.
Monitoring Bone Health
Untreated celiac disease can lead to reduced bone mineral density and an increased risk of osteoporosis and fractures. As a nurse, it is important to monitor bone health and ensure appropriate interventions are in place to prevent complications.
Encourage patients to discuss bone health with their healthcare provider and undergo bone density testing if indicated. Promote regular weight-bearing exercise, adequate calcium and vitamin D intake, and any prescribed medications to optimize bone health.
Identifying Long-Term Complications
Celiac disease, if left untreated or poorly managed, can lead to various long-term complications. These may include refractory celiac disease, lymphoma, infertility, or neurological disorders. While these complications are relatively uncommon, vigilance in monitoring and early intervention is essential.
Collaborate with the healthcare team to identify potential red flags and educate patients about the signs and symptoms of these complications. Encourage patients to promptly report any new or worsening symptoms to ensure timely evaluation and management.

Collaboration with Healthcare Team
Working with Dietitians
The expertise of a registered dietitian is invaluable when managing patients with celiac disease. Collaborating with dietitians helps ensure patients receive accurate and personalized dietary advice, enabling them to adhere to a gluten-free lifestyle effectively.
Refer patients to registered dietitians who specialize in celiac disease management. Encourage patients to attend appointments and actively engage with the dietitian to address their specific nutritional needs and challenges.
Consulting Gastroenterologists
Gastroenterologists play a central role in the diagnosis and management of celiac disease. Collaborate closely with gastroenterologists to ensure a multidisciplinary approach to patient care.
Maintain open lines of communication with the gastroenterologist, providing updates on the patient’s progress, laboratory test results, and any concerns or changes in symptoms. This collaborative approach helps optimize patient outcomes and facilitates comprehensive care.
Coordinating with Mental Health Professionals
Celiac disease can have a significant impact on patients’ mental health, leading to increased stress, anxiety, and depression. To provide holistic care, it is important to involve mental health professionals in the management of celiac disease.
Collaborate with psychologists, therapists, or counselors who have experience working with patients with chronic illnesses or autoimmune conditions. Facilitate referrals to mental health professionals to ensure patients receive the necessary support to manage the emotional challenges associated with celiac disease.
Engaging in Interprofessional Care
Caring for patients with celiac disease necessitates an interprofessional approach, with multiple healthcare providers working together. Collaborate with the entire healthcare team, including primary care physicians, pharmacists, and allied health professionals, to ensure comprehensive and coordinated care.
Regularly engage in team meetings, case conferences, and other interprofessional activities to foster collaboration and share knowledge. By working together effectively, healthcare providers can improve patient outcomes, optimize care, and enhance the overall patient experience.
Safe Environment
Preventing Cross-Contamination
Creating a safe environment is crucial for patients with celiac disease to avoid gluten exposure. As a nurse, you can help educate patients and their families on strategies to prevent cross-contamination.
Teach patients the importance of having separate kitchen utensils, cutting boards, and toasters dedicated to gluten-free use. Explain the necessity of thoroughly cleaning kitchen surfaces and ensuring that gluten-containing foods are kept away from gluten-free alternatives. Reinforce the importance of safe food storage practices to minimize the risk of accidental gluten exposure.
Ensuring Gluten-Free Meal Preparations
In healthcare settings, it is essential to provide gluten-free meal options and ensure safe meal preparations for patients with celiac disease. Collaborate with the dietary department to ensure they have protocols in place to accommodate gluten-free diets.
Work with the dietary team to create clear guidelines for meal preparation, including the segregation of gluten-free ingredients and safe food handling practices. Regularly communicate with the dietary staff and patients to address any concerns or issues related to gluten-free meal preparations.
Providing Patient and Family Education on Safe Practices
Educating patients and their families on safe practices for a gluten-free lifestyle is essential to prevent inadvertent gluten exposure. Provide detailed education on safe food handling, label reading, and cross-contamination prevention.
Offer resources such as brochures, handouts, or online materials that outline safe practices and provide practical tips for maintaining a gluten-free environment at home. Encourage patients and their families to actively participate in learning and implementing safe practices.
Promoting Self-Management
Empowering Patients to Take Control
Empowerment is key to successful long-term management of celiac disease. As a nurse, you can help patients develop self-management skills to effectively navigate the challenges associated with the condition.
Encourage patients to take an active role in their healthcare, teaching them to advocate for themselves and effectively communicate their needs. Help them set goals and develop action plans to achieve and maintain optimal health and well-being.
Teaching Label Reading
Accurate label reading is a fundamental skill for patients with celiac disease. Provide patients with hands-on education on how to read food labels effectively and identify potential sources of gluten.
Teach patients to identify ingredients that may contain hidden sources of gluten, such as modified food starch, malt, and hydrolyzed vegetable protein. Encourage them to verify the gluten-free status of products through gluten-free certification labels or by contacting manufacturers directly.
Encouraging Meal Planning and Preparation
Meal planning and preparation are critical in maintaining a gluten-free lifestyle. Help patients develop practical strategies for meal planning and preparation that fit their individual needs, preferences, and lifestyle.
Guide patients in creating weekly meal plans, outlining gluten-free breakfast, lunch, dinner, and snack options. Teach them how to batch cook and freeze meals for convenience. Encourage them to explore new recipes and experiment with gluten-free ingredients to ensure dietary variety and enjoyment.
Providing Resources for Recipes and Tips
Providing patients with resources for recipes and tips can greatly support their journey towards successful gluten-free living. Share reliable sources for gluten-free recipes, such as cookbooks, websites, and mobile applications.
Highlight the importance of reaching out to local celiac support groups, both online and offline, where patients can access a wealth of information, recipes, and personal experiences. These resources can help patients expand their culinary repertoire and enhance adherence to a gluten-free diet.
Emergency Preparedness
Educating on Emergency Plans
In emergency situations, patients with celiac disease may face additional challenges in safely managing their dietary needs. As a nurse, it is important to educate patients on emergency preparedness and provide guidance on how to navigate potential disruptions in gluten-free food access.
Encourage patients to develop an emergency plan that includes a supply of gluten-free non-perishable items, such as canned goods, dried fruits, and gluten-free snack bars. Teach them to identify safe food sources in emergency situations, such as local food banks or emergency relief organizations.
Addressing Potential Gluten Exposure Scenarios
Despite diligent efforts, there may be instances where patients with celiac disease accidentally ingest gluten. Educate patients on common scenarios that may result in gluten exposure and provide guidance on managing these situations.
Help patients recognize the signs and symptoms of gluten ingestion and teach them how to manage mild reactions, such as gastrointestinal discomfort or mild allergic symptoms. Emphasize the importance of seeking immediate medical attention in cases of severe allergic reactions or anaphylaxis.
Recognizing and Managing Gluten-Related Emergencies
In rare cases, gluten-related emergencies such as anaphylaxis or severe allergic reactions may occur. As a nurse, being prepared to recognize and manage these emergencies is vital.
Train patients on how to administer self-injectable epinephrine and provide them with a written emergency action plan. Encourage patients to wear medical alert bracelets or carry medical identification cards that describe their diagnosis of celiac disease and potential allergic reactions to gluten.
In summary, managing celiac disease requires a comprehensive and multidisciplinary approach. As a nurse, you play a crucial role in confirming the diagnosis, educating patients about a gluten-free diet, supporting medication administration, providing psychosocial support, and ensuring a safe environment. By promoting self-management and collaborating with the healthcare team, you can empower patients to successfully manage their condition and improve their quality of life.