You’ve landed on a page filled with valuable information and insights about nursing considerations for Hashimoto’s Thyroiditis. From nursing management strategies to essential considerations, this article aims to equip you with the knowledge you need to provide top-notch care for patients with this condition. So, whether you’re a seasoned nurse or just starting your career, get ready to enhance your understanding and skills in supporting individuals with Hashimoto’s Thyroiditis. Let’s embark on this journey together!
Assessment
Thyroid function tests
When assessing a patient with Hashimoto’s Thyroiditis, thyroid function tests play a crucial role in determining the extent of thyroid dysfunction. These tests include measuring levels of thyroid-stimulating hormone (TSH), free thyroxine (T4), and triiodothyronine (T3). Elevated TSH levels and decreased T4 and T3 levels are typically observed in individuals with Hashimoto’s Thyroiditis, indicating hypothyroidism. Regular monitoring of these levels is important to assess the effectiveness of treatment and ensure appropriate management of the condition.
Symptom assessment
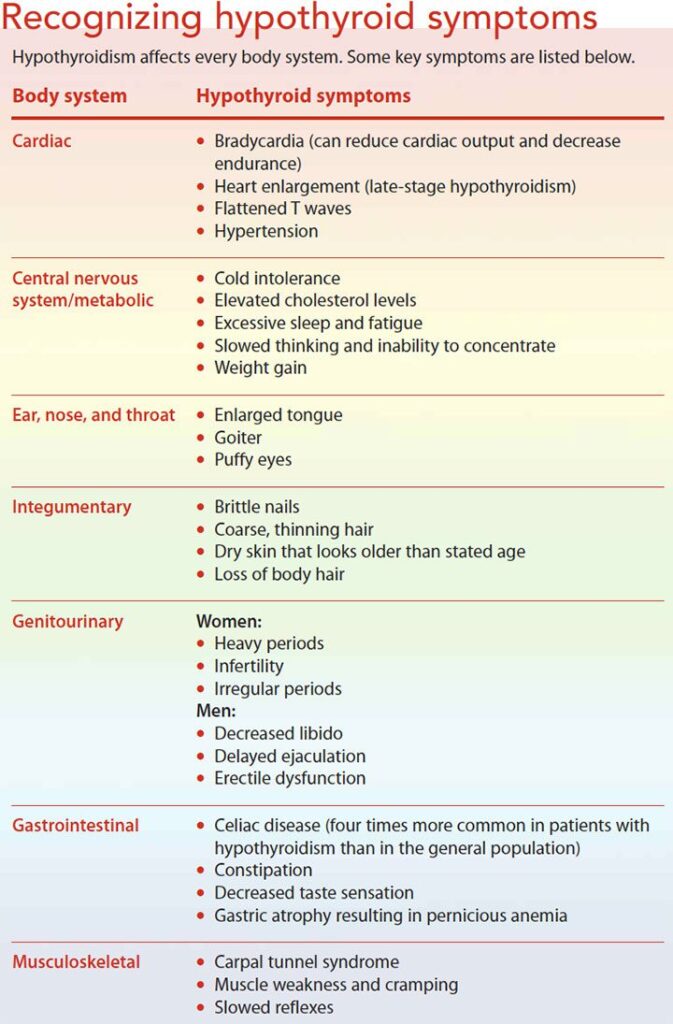
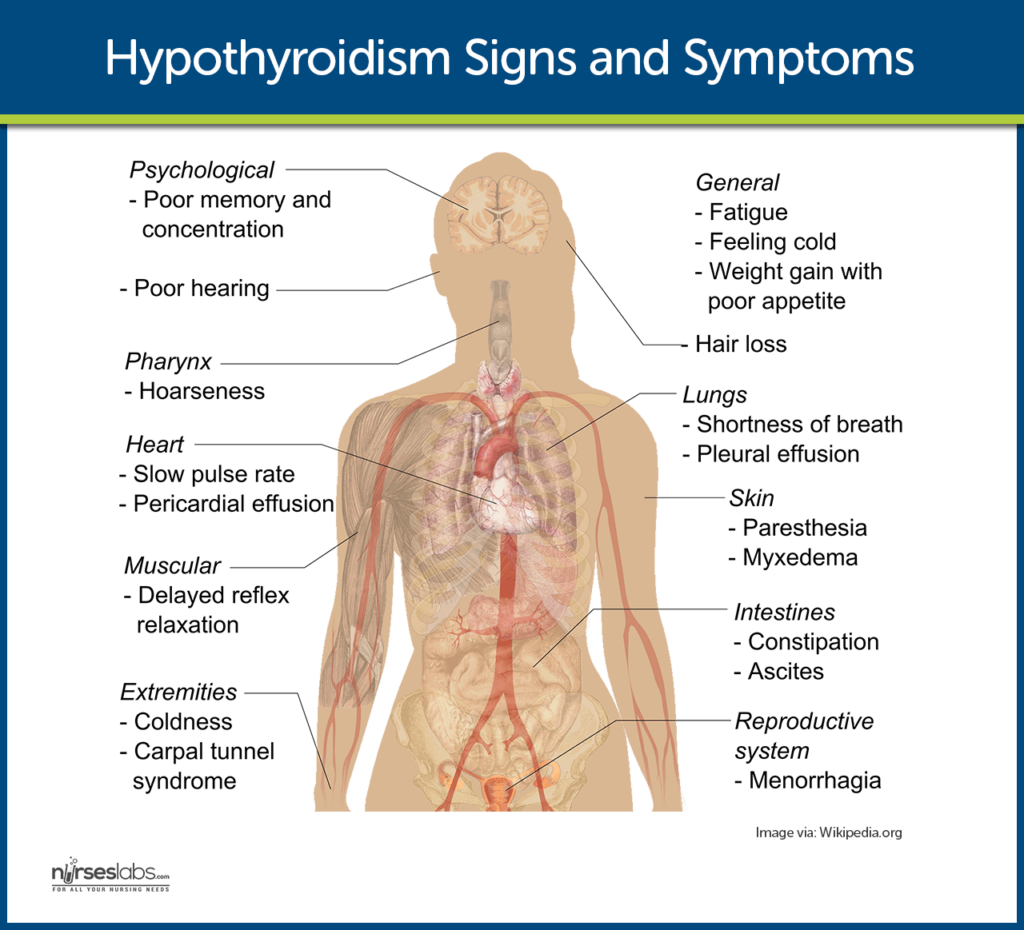
Assessing the symptoms experienced by a patient with Hashimoto’s Thyroiditis is essential for understanding the impact of the disease on their daily life. Common symptoms include fatigue, weight gain, cold intolerance, constipation, dry skin, and depression. Additionally, patients may experience muscle aches, joint pain, and menstrual irregularities. By thoroughly assessing these symptoms, healthcare providers can tailor treatment plans to alleviate discomfort and improve the patient’s overall well-being.
Patient history
Obtaining a detailed patient history is crucial for understanding the progression and management of Hashimoto’s Thyroiditis. This includes identifying risk factors, such as a family history of thyroid disorders or autoimmune diseases, previous exposure to radiation, and potential triggers that may have contributed to the development of the condition. Additionally, it is important to review the patient’s medical history, including any previous or current thyroid dysfunction, as well as their current medications and allergies. Gathering this information enables healthcare providers to develop a personalized care plan that addresses the specific needs and concerns of each individual.
Diagnostic Evaluation
Physical examination
A comprehensive physical examination is an important component of diagnosing and managing Hashimoto’s Thyroiditis. During the examination, healthcare providers assess for physical manifestations of the disease, such as a goiter (enlarged thyroid gland), dry skin, and hair loss. Identifying other associated signs, such as weight gain, slow reflexes, and bradycardia, can further aid in confirming the diagnosis of hypothyroidism. Additionally, the examination may reveal other potential complications or comorbidities that require further evaluation and management.
Laboratory tests
Laboratory tests are essential for diagnosing Hashimoto’s Thyroiditis and monitoring the patient’s thyroid function. In addition to the thyroid function tests mentioned earlier, it is important to measure thyroid peroxidase antibodies (TPOAb) and thyroglobulin antibodies (TgAb). Elevated levels of these antibodies are indicative of an autoimmune process and confirm the diagnosis of Hashimoto’s Thyroiditis. Regular monitoring of these antibody levels allows healthcare providers to assess disease progression, adjust treatments accordingly, and identify potential complications.
Ultrasound imaging
Ultrasound imaging is a valuable tool for evaluating the structure and size of the thyroid gland in patients with Hashimoto’s Thyroiditis. This non-invasive procedure provides detailed images of the gland, allowing healthcare providers to assess for the presence of nodules or other abnormalities. Ultrasound imaging also aids in distinguishing between Hashimoto’s Thyroiditis and other thyroid diseases, such as thyroid cancer. By detecting any structural changes or complications, healthcare providers can ensure appropriate management and timely intervention if necessary.

Medication Management
Levothyroxine therapy
Levothyroxine therapy is the cornerstone of treatment for individuals with Hashimoto’s Thyroiditis who are hypothyroid. This medication provides synthetic thyroid hormone to supplement the body’s insufficient production. Levothyroxine is taken orally on an empty stomach, usually in the morning, to ensure optimal absorption. The initial dosage is typically based on the patient’s weight, age, and severity of hypothyroidism. Regular monitoring of thyroid function tests is crucial to determine the appropriate dosage and ensure that the patient’s hormone levels are within the target range.
Medication administration
Proper administration of levothyroxine is vital for ensuring its effectiveness. It is important to counsel patients on the correct technique for taking the medication. Levothyroxine should be taken consistently, around the same time each day, preferably on an empty stomach. It is important to avoid certain substances that may interfere with its absorption, such as calcium and iron supplements, antacids, and certain foods. Patients should also be aware that other medications, such as proton pump inhibitors and certain antidepressants, may interact with levothyroxine and affect its absorption or metabolism. Educating patients on proper medication administration helps optimize treatment outcomes and prevents potential drug interactions.
Monitoring drug effectiveness
Regular monitoring of thyroid function tests is essential for assessing the effectiveness of levothyroxine therapy. Patients’ TSH levels should ideally be maintained within the normal reference range, while T4 and T3 levels should be optimized to alleviate hypothyroid symptoms. Healthcare providers should establish a follow-up schedule tailored to each patient’s unique needs. Any adjustments to the dosage should be based on the patient’s symptoms, hormone levels, and response to treatment. Ensuring optimal medication effectiveness is a key component of managing Hashimoto’s Thyroiditis and promoting the patient’s overall well-being.
Patient Education
Disease understanding
Educating patients about Hashimoto’s Thyroiditis is crucial for empowering them to actively participate in their own care. Patients should be provided with a clear explanation of the disease process, including its autoimmune nature and the impact on thyroid function. Understanding the chronic nature of the condition helps patients develop realistic expectations and cope with the challenges they may face. Healthcare providers should also address common misconceptions about the disease, promoting accurate knowledge and dispelling any myths or fears associated with it.
Medication adherence
Ensuring medication adherence is essential for optimal management of Hashimoto’s Thyroiditis. Patients should be educated on the importance of taking their prescribed medication consistently and as instructed. Healthcare providers should provide detailed instructions on proper administration, including the timing, potential interactions, and precautions to take. Emphasizing the long-term nature of levothyroxine therapy and its role in maintaining thyroid hormone levels within the target range helps patients understand the need for ongoing adherence. Regular discussions and follow-up appointments can help identify and address any challenges or concerns that may affect medication adherence.
Lifestyle modifications
In addition to medication management, lifestyle modifications can significantly impact the well-being of individuals with Hashimoto’s Thyroiditis. Patients should be encouraged to maintain a healthy and balanced diet, rich in fruits, vegetables, and lean proteins. Dietary considerations, such as adequate iodine intake and potential goitrogenic foods, should be discussed to help patients make informed choices. Regular physical activity is also important for managing weight and improving overall health. Patients should be encouraged to engage in appropriate exercise routines based on their individual capabilities and preferences. Promoting a healthy lifestyle as part of the patient education process is essential for optimizing the management of Hashimoto’s Thyroiditis.
Dietary Considerations
Iodine intake
Iodine plays a crucial role in thyroid hormone synthesis, and ensuring appropriate iodine intake is important for individuals with Hashimoto’s Thyroiditis. However, the level of iodine supplementation needed can vary based on the individual’s specific circumstances. Healthcare providers should assess the patient’s iodine levels and consider the dietary sources of iodine. Some patients may benefit from iodine supplementation, while others require caution due to the presence of coexisting conditions, such as iodine-induced hyperthyroidism or a predisposition to thyroid nodules. Individualized dietary advice and appropriate monitoring of iodine levels are essential to guide patients in maintaining optimal thyroid health.
Goitrogenic foods
Goitrogenic foods are substances that can interfere with the production of thyroid hormones and potentially exacerbate the symptoms of Hashimoto’s Thyroiditis. These foods contain compounds that can inhibit the uptake of iodine by the thyroid gland or interfere with the conversion of thyroxine (T4) to triiodothyronine (T3). Patients should be informed about these foods and their potential effects. Cruciferous vegetables, such as broccoli, cabbage, and kale, are common examples of goitrogenic foods. However, it is important to note that cooking can deactivate some of the goitrogenic compounds, reducing their impact. Encouraging patients to consume these foods in moderation and be mindful of their preparation methods helps promote a balanced diet while minimizing any potential negative effects on thyroid function.
Nutritional counseling
Nutritional counseling plays a valuable role in the management of Hashimoto’s Thyroiditis. Individual dietary needs vary, and healthcare providers should consider factors such as the patient’s age, weight, coexisting conditions, and preferences. Registered dietitians can provide personalized counseling sessions and create meal plans tailored to the patient’s unique needs. They can also address any diet-related concerns the patient may have, such as weight management, food allergies, or sensitivities. Collaborating with a dietitian ensures that patients receive accurate, evidence-based information and practical guidance to make informed dietary choices that support their overall health and well-being.
Psychosocial Support
Emotional well-being
Hashimoto’s Thyroiditis can have a significant impact on a patient’s emotional well-being. The chronic nature of the disease, along with its associated symptoms, can lead to feelings of frustration, anxiety, and even depression. It is essential for healthcare providers to address the emotional aspect of the disease during patient interactions. Taking the time to actively listen to patients, validating their feelings, and providing emotional support can positively impact their overall well-being. Incorporating mental health professionals into the care team and referring patients for counseling or therapy may be beneficial for those who require additional support.
Coping strategies
Helping patients develop effective coping strategies can enhance their ability to manage the challenges of living with Hashimoto’s Thyroiditis. Encouraging patients to engage in stress-reducing activities, such as exercise, meditation, or hobbies, can help alleviate symptoms and promote overall well-being. Providing information on relaxation techniques, deep breathing exercises, or mindfulness practices can assist in managing stress and anxiety. Additionally, connecting patients with support groups or online communities where they can share experiences and receive encouragement from others facing similar challenges can be empowering and comforting.
Support groups
Support groups can be invaluable resources for individuals with Hashimoto’s Thyroiditis. These groups provide a safe space for patients to share their experiences, ask questions, and learn from one another. Support group meetings, whether in-person or virtual, offer opportunities for patients to connect, gain emotional support, and gather practical tips for managing their condition. Healthcare providers should provide information on local support groups and online communities to patients, empowering them to access these valuable resources. The sense of community and mutual support obtained from participating in support groups can contribute positively to the well-being of individuals with Hashimoto’s Thyroiditis.

Comorbidity Management
Management of coexistent conditions
Patients with Hashimoto’s Thyroiditis may be at an increased risk of developing other autoimmune conditions, such as celiac disease, type 1 diabetes, or vitiligo. Healthcare providers should be vigilant in screening for and managing these potential comorbidities. Regular monitoring of relevant laboratory tests, such as screening for celiac disease antibodies or measuring blood glucose levels, can aid in early detection and prompt management. Collaborating with other specialists, such as gastroenterologists or endocrinologists, is crucial in coordinating comprehensive care and optimizing outcomes for patients with Hashimoto’s Thyroiditis and coexisting conditions.
Interactions with other medications
Patients with Hashimoto’s Thyroiditis may require treatment for other conditions or medications that can potentially interact with their thyroid medication. It is important to review the patient’s complete medication profile and assess for any potential drug-drug interactions. Healthcare providers should educate patients on the importance of informing all healthcare professionals about their thyroid condition to ensure safe prescribing practices. Additionally, patients should be encouraged to carefully read medication labels and consult their healthcare providers or pharmacists regarding potential interactions if they initiate any new medications, including over-the-counter or herbal remedies.
Collaboration with healthcare team
Collaboration among healthcare providers is essential to provide comprehensive care for individuals with Hashimoto’s Thyroiditis. Effective interdisciplinary collaboration ensures that all aspects of the patient’s health and well-being are addressed. Communication and coordination among primary care providers, endocrinologists, pharmacists, registered dietitians, mental health professionals, and other specialists facilitate optimal management of the disease. Sharing information, discussing treatment plans, and promptly addressing any concerns or complications arising from the disease or treatment contribute to delivering patient-centered care and improving outcomes.
Monitoring and Follow-up
Lab test monitoring
Regular monitoring of thyroid function tests is crucial in the ongoing management of Hashimoto’s Thyroiditis. Tracking TSH, T4, T3, TPOAb, and TgAb levels is important in assessing treatment effectiveness and ensuring hormone levels are within the desired range. The frequency of monitoring may vary depending on the patient’s stability and response to treatment. Additionally, monitoring indicators of potential complications, such as cholesterol levels, blood pressure, and cardiac function, may be necessary to address additional health risks associated with hypothyroidism. Ongoing lab test monitoring allows healthcare providers to make necessary adjustments to medication dosage, identify potential issues early, and optimize patient care.
Evaluation of symptom management
In addition to lab test monitoring, evaluating the management of Hashimoto’s Thyroiditis involves assessing the patient’s overall symptom burden and quality of life. Regular follow-up appointments provide an opportunity to discuss the patient’s ongoing symptoms, treatment adherence, and any challenges they may be experiencing. Evaluating the patient’s response to treatment involves assessing improvements in symptoms such as fatigue, weight gain or loss, constipation, and mood changes. Identifying persistent or new symptoms helps guide treatment adjustments or referrals to specialists, if necessary, to address and manage Hashimoto’s Thyroiditis comprehensively.
Adjustment of medication dosage
Adjusting the dosage of levothyroxine is a common aspect of managing Hashimoto’s Thyroiditis. The optimal dosage depends on the patient’s symptoms, hormone levels, and response to treatment. Regular monitoring of thyroid function tests, as well as clinical assessments, guides healthcare providers in determining whether a dosage adjustment is needed. Increasing or decreasing the levothyroxine dosage aims to achieve euthyroidism, where the patient’s hormone levels are within the target range, resulting in improved symptom control and overall well-being. Collaborative decision-making and ongoing communication with the patient are crucial in ensuring appropriate dosage adjustments and promoting optimal management of the disease.

Complication Recognition
Hypothyroid crisis
Hypothyroid crisis, also known as myxedema coma, is a rare but life-threatening complication of Hashimoto’s Thyroiditis. It occurs when severe hypothyroidism leads to a state of altered mental status, hypothermia, respiratory depression, and cardiovascular collapse. Prompt recognition and immediate medical intervention are necessary to prevent further deterioration and potentially fatal outcomes. Healthcare providers should educate patients on the signs and symptoms of hypothyroid crisis, including extreme fatigue, confusion, lethargy, and unresponsiveness. Teaching patients and their caregivers when and how to seek emergency medical attention is vital to ensure timely intervention in the event of this complication.
Thyroid nodules or cancer
Individuals with Hashimoto’s Thyroiditis may have an increased risk of developing thyroid nodules or thyroid cancer. These nodules can be benign or malignant, and appropriate evaluation is essential to determine their nature and guide management. Healthcare providers should regularly assess the patient’s thyroid gland for any new or changing nodules during physical examinations. In cases where a nodule is identified, further evaluation, such as ultrasound imaging or fine-needle aspiration biopsy, may be necessary to determine its malignant potential. Timely recognition and referral to specialists, such as endocrinologists or surgeons, can facilitate appropriate management and potentially prevent adverse outcomes.
Autoimmune diseases
Hashimoto’s Thyroiditis is an autoimmune disease itself, and individuals who have it may be at an increased risk of developing other autoimmune conditions. These conditions can include rheumatoid arthritis, systemic lupus erythematosus, or Sjögren’s syndrome, among others. Recognizing the potential for these comorbidities is important, as they may require additional monitoring and management. Patients should be educated about the signs and symptoms associated with other autoimmune diseases and advised to report any new or concerning symptoms promptly. Collaborating with other specialists in managing these conditions ensures comprehensive care and aids in improving patient outcomes.
Collaborative Care
Interprofessional collaboration
Collaboration among various healthcare professionals is key to providing optimal care for individuals with Hashimoto’s Thyroiditis. Interprofessional collaboration involves effective communication, shared decision-making, and mutual respect among members of the healthcare team. Primary care providers, endocrinologists, pharmacists, registered dietitians, mental health professionals, and other specialists must work together to coordinate and integrate care for patients with complex needs. Regular case discussions, joint educational initiatives, and care coordination meetings help ensure continuity of care, foster a patient-centered approach, and enhance the overall management of Hashimoto’s Thyroiditis.
Referrals to specialists
Referrals to specialists play an important role in managing Hashimoto’s Thyroiditis, particularly when complications or comorbidities arise. Specific referrals may be necessary for conditions such as thyroid nodules, thyroid cancer, or other autoimmune diseases. Endocrinologists, surgeons, radiologists, and other specialists can provide expert evaluation, guidance, and interventions as needed. Prompt referrals and effective communication with specialists contribute to comprehensive and coordinated care, ensuring that all aspects of the patient’s health are addressed appropriately.
Ongoing communication
Open and ongoing communication between healthcare providers and patients is vital in managing Hashimoto’s Thyroiditis. Establishing a trusting relationship fosters effective care, patient engagement, and shared decision-making. Regular follow-up appointments, either in person or virtually, allow for discussion and monitoring of the patient’s progress, addressing any concerns or questions they may have. Prompt communication channels, such as secure messaging systems or dedicated phone lines, enable patients to seek guidance or report changes in their symptoms promptly. Cultivating a supportive and collaborative environment promotes optimal care outcomes and patient satisfaction.
In conclusion, nursing considerations for Hashimoto’s Thyroiditis encompass a comprehensive approach that encompasses assessment, diagnostic evaluation, medication management, patient education, dietary considerations, psychosocial support, comorbidity management, monitoring, complication recognition, collaborative care, and ongoing communication. By addressing each aspect of care, healthcare providers can support individuals with Hashimoto’s Thyroiditis in effectively managing their condition, promoting overall well-being, and improving their quality of life. A holistic approach, tailored to each patient’s unique needs, ensures comprehensive and patient-centered care for those living with Hashimoto’s Thyroiditis.