In this article, you will explore the essential nursing considerations for managing signs of eating disorders. As a nurse, understanding these considerations is crucial for effectively supporting individuals struggling with eating disorders. By recognizing the signs, assessing their physical and emotional well-being, and implementing appropriate nursing interventions, you can play a vital role in helping patients on their journey towards recovery. Let’s delve into the essential nursing management strategies and discover how you can make a positive difference in their lives.
Assessment and Diagnosis
Screening for eating disorders
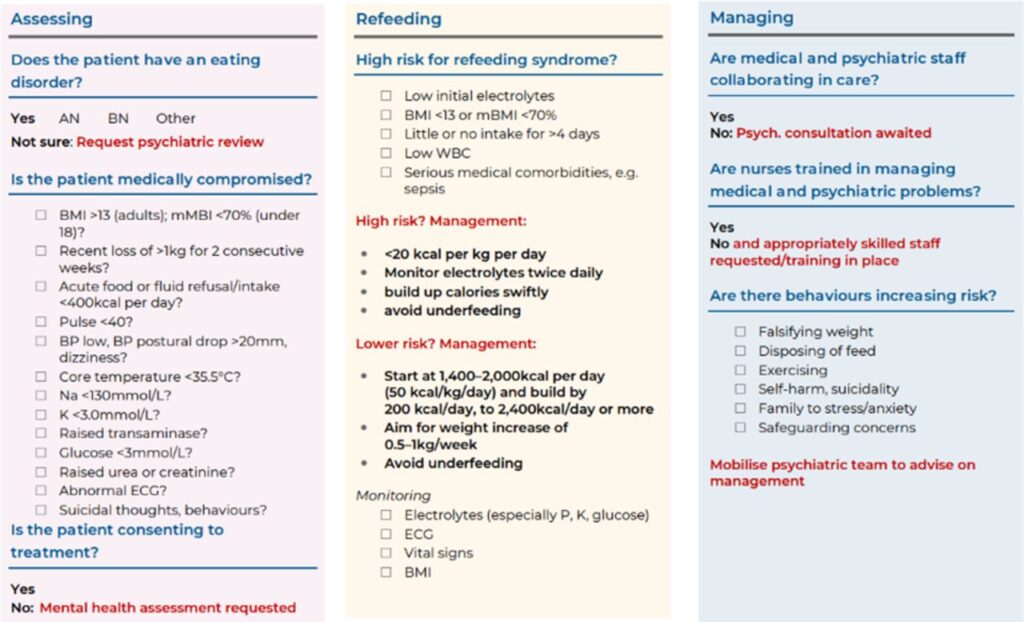
When it comes to assessing and diagnosing eating disorders, screening plays a crucial role. Screening methods can include structured interviews, questionnaires, and physical assessments. These tools help healthcare professionals identify potential eating disorders in patients. By using validated screening tools, healthcare providers can gather essential information about eating habits, body image, and other related factors. It’s important to screen for eating disorders regularly, as early identification and intervention can greatly improve outcomes.
Assessing physical and psychological symptoms
Assessing physical and psychological symptoms is an integral part of diagnosing and managing eating disorders. Physical symptoms can range from weight loss or gain to gastrointestinal issues and nutrient deficiencies. Psychological symptoms may include anxiety, depression, body dissatisfaction, and distorted body image. By conducting a comprehensive assessment of both physical and psychological symptoms, healthcare professionals can gain a better understanding of the patient’s overall health and tailor their care accordingly.
Identifying co-occurring disorders
Many individuals with eating disorders also experience co-occurring disorders such as anxiety, depression, substance abuse, or self-harm behaviors. Identifying these co-occurring disorders is crucial for developing an effective treatment plan. Healthcare professionals need to conduct thorough assessments and collaborate with mental health professionals to address all aspects of the patient’s mental well-being. Treating both the eating disorder and the co-occurring disorders simultaneously can yield better outcomes and improve the overall quality of life for patients.
Diagnostic criteria for different eating disorders
Different eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, have specific diagnostic criteria. These criteria help healthcare professionals make an accurate diagnosis and determine appropriate treatment strategies. For example, the diagnostic criteria for anorexia nervosa include a significantly low body weight, an intense fear of gaining weight, and a distorted body image. Understanding the diagnostic criteria for each eating disorder guides healthcare professionals in providing evidence-based care and tailoring interventions to meet the specific needs of each patient.
Collaborative Care Planning
Involving the interdisciplinary team
Collaboration among healthcare professionals is key to providing comprehensive care for individuals with eating disorders. In addition to nurses, the interdisciplinary team may include doctors, psychologists, dietitians, therapists, and social workers. Each team member brings a unique perspective and expertise to the table, ensuring all aspects of the patient’s care are addressed. By involving the interdisciplinary team in care planning, healthcare professionals can create a holistic treatment approach that takes into account the physical, psychological, and social aspects of the patient’s well-being.
Developing an individualized care plan
Every patient with an eating disorder has unique needs and challenges. Developing an individualized care plan is essential for providing effective treatment. The care plan should consider the patient’s specific symptoms, co-occurring disorders, and personal goals. It should also take into account the patient’s cultural background, support system, and resources available. By tailoring the care plan to each individual, healthcare professionals can enhance patient engagement and increase the likelihood of successful treatment outcomes.
Setting realistic goals
Setting realistic goals is essential in the treatment of eating disorders. It’s important to work closely with patients to establish achievable objectives that align with their personal preferences and circumstances. Unrealistic goals can lead to frustration and a sense of failure, which can hinder the recovery process. By setting realistic goals, healthcare professionals can help patients build confidence and motivation as they make progress towards their recovery.
Engaging the patient in decision-making
Empowering patients to actively participate in their care is a crucial aspect of managing eating disorders. Engaging the patient in decision-making helps foster a sense of ownership and autonomy, leading to increased adherence to treatment plans. Healthcare professionals should involve patients in discussions about their diagnosis, treatment options, and goal-setting. By respecting patients’ preferences and involving them in the decision-making process, healthcare professionals can enhance patient satisfaction and improve treatment outcomes.
Medical Considerations
Monitoring vital signs and lab values
Regular monitoring of vital signs and lab values is essential for managing the medical implications of eating disorders. Patients with eating disorders may experience abnormalities in blood pressure, heart rate, electrolyte balance, and blood glucose levels. By closely monitoring these vital signs and lab values, healthcare professionals can detect early signs of complications and intervene promptly. Regular monitoring also provides an opportunity to assess the effectiveness of treatment interventions and adjust the care plan as needed.
Addressing medical complications
Eating disorders can have severe medical complications that require diligent attention. Some common complications include electrolyte imbalances, osteoporosis, amenorrhea, and gastrointestinal issues. Healthcare professionals play a vital role in addressing these complications through medical interventions, such as rehydration, electrolyte replacement, calcium and vitamin D supplementation, and managing gastrointestinal symptoms. By addressing medical complications promptly and effectively, healthcare professionals can support the patient’s overall recovery and prevent long-term health consequences.
Providing nutrition support
Nutrition plays a vital role in the management of eating disorders. Healthcare professionals, particularly dietitians, can provide nutrition support by assessing the patient’s current dietary intake and developing individualized meal plans. Nutrition support may involve ensuring adequate energy and nutrient intake, promoting a balanced diet, and working collaboratively with patients to establish a healthy relationship with food. By addressing nutritional needs, healthcare professionals can optimize the patient’s physical health and support their overall recovery.
Administering medications as prescribed
In some cases, the use of medications may be necessary to manage specific symptoms or co-occurring disorders associated with eating disorders. Healthcare professionals should administer medications as prescribed by the physician or psychiatrist. Medications may include antidepressants, antianxiety medications, mood stabilizers, or medications to address medical complications. Close monitoring of medication effects and potential side effects is essential to ensure patient safety and promote optimal treatment outcomes.
Psychiatric Support
Assessing and managing suicidal ideation
Individuals with eating disorders are at an increased risk of suicidal ideation and self-harm behaviors. Healthcare professionals need to conduct thorough assessments to identify and manage these risks effectively. Assessments should include questions about suicidal thoughts, plans, and intent. If suicidal ideation or self-harm behaviors are present, appropriate interventions, such as safety planning, psychological support, and referral to mental health professionals, should be implemented. Regular monitoring of suicidal ideation throughout the treatment process is crucial to ensure patient safety and provide appropriate support.
Addressing body image distortion
Distorted body image is a common feature of eating disorders and can significantly impact an individual’s self-esteem and overall well-being. Healthcare professionals should assess and address body image distortion as part of the treatment plan. This may involve cognitive-behavioral therapy (CBT) techniques, such as cognitive restructuring and exposure therapy, to challenge and modify negative body image perceptions. By addressing body image distortion, healthcare professionals can help patients develop a healthier and more positive perception of themselves.
Implementing cognitive-behavioral therapy
Cognitive-behavioral therapy (CBT) is a well-established treatment approach for eating disorders. CBT focuses on identifying and modifying the thoughts, behaviors, and emotions associated with disordered eating patterns. Healthcare professionals can implement CBT techniques, such as self-monitoring, challenging negative thoughts, and developing coping strategies, to help patients develop healthier attitudes towards food, body image, and self-care. CBT can be used as an individual or group therapy modality, depending on the patient’s needs and preferences.
Providing psychoeducation to patient and family
Psychoeducation is an integral component of eating disorder treatment. Healthcare professionals should provide patients and their families with information about eating disorders, including the signs and symptoms, risk factors, and treatment options. Psychoeducation helps patients and families gain a better understanding of the disorder, reduce stigma, and actively engage in the treatment process. By providing accurate and evidence-based information, healthcare professionals can empower patients and their families to become active participants in their recovery journey.
Nutritional Management
Assessing nutritional status
Assessing the nutritional status of individuals with eating disorders is a crucial step in developing an effective care plan. Healthcare professionals, particularly dietitians, can assess the patient’s current dietary intake and evaluate for nutrient deficiencies. Nutritional assessments may involve collecting detailed dietary histories, reviewing food records, and conducting physical assessments, such as measuring height, weight, and body composition. By assessing nutritional status, healthcare professionals can identify specific areas of concern and develop targeted interventions to improve the patient’s overall nutrition.
Calculating daily caloric needs
Calculating daily caloric needs is essential in helping patients with eating disorders achieve and maintain a healthy weight. Healthcare professionals, particularly dietitians, can use various equations and formulas to estimate an individual’s energy requirements. Factors such as age, gender, height, weight, and physical activity level are taken into account. By calculating daily caloric needs, healthcare professionals can ensure that patients are receiving an appropriate amount of energy to support their physiological and psychological well-being.
Designing a balanced meal plan
Designing a balanced meal plan is essential for individuals with eating disorders to establish regular eating patterns and meet their nutritional needs. Healthcare professionals, particularly dietitians, can develop meal plans that include a variety of foods from different food groups while taking into account the patient’s preferences and dietary restrictions. A balanced meal plan should provide a range of macronutrients, vitamins, and minerals to support overall health and promote optimal recovery.
Promoting regular eating patterns
Establishing regular eating patterns is a crucial aspect of managing eating disorders. Healthcare professionals can support patients in developing consistent meal and snack times to promote a balanced intake of nutrients. Regular eating patterns help regulate hunger and fullness cues, prevent extreme hunger or excessive fullness, and reduce disordered eating behaviors. By promoting regular eating patterns, healthcare professionals can support patients in their journey towards establishing a healthier relationship with food and eating.
Behavioral Interventions
Helping patients develop coping strategies
Individuals with eating disorders often rely on disordered eating behaviors as coping mechanisms for emotional distress. Healthcare professionals play a vital role in helping patients develop healthier coping strategies. This may involve providing psychoeducation on emotion regulation, stress management techniques, and alternative coping mechanisms, such as engaging in hobbies, practicing mindfulness, or seeking social support. By helping patients develop effective coping strategies, healthcare professionals can decrease reliance on disordered eating behaviors and promote overall psychological well-being.
Implementing behavior modification techniques
Behavior modification techniques can be effective tools in managing eating disorders. Healthcare professionals can employ strategies such as self-monitoring, reinforcement, and stimulus control to help patients modify their eating behaviors. These techniques aim to increase awareness of eating patterns, reinforce positive behaviors, and provide structure and guidance for meal planning and timing. By implementing behavior modification techniques, healthcare professionals can support patients in making sustainable changes towards a healthier relationship with food and eating.
Monitoring and documenting food intake
Monitoring and documenting food intake is an important part of managing eating disorders. Healthcare professionals can work with patients to develop a system for tracking food consumption. This may involve keeping a food diary, utilizing smartphone apps, or using other tools to monitor and document eating patterns. Regular monitoring and documentation of food intake can help identify problematic behaviors, assess progress, and provide valuable information for making adjustments to the treatment plan.
Promoting healthy body image
Promoting a healthy body image is a key component of managing eating disorders. Healthcare professionals can incorporate body acceptance and positive body image practices into the treatment plan. This may involve encouraging patients to engage in activities that promote self-care and self-compassion, rather than focusing solely on physical appearance. By promoting a healthy body image, healthcare professionals can help patients develop a more positive relationship with their bodies and decrease body dissatisfaction.
Education and Counseling
Providing information on eating disorders
Education plays a crucial role in the management of eating disorders. Healthcare professionals should provide patients and their families with accurate and age-appropriate information about eating disorders. This includes explaining the causes, consequences, and treatment options available. By providing education, healthcare professionals can dispel myths, reduce stigma, and empower patients to actively participate in their treatment and recovery.
Exploring underlying issues and triggers
Eating disorders are often linked to underlying psychological, emotional, or interpersonal issues. Healthcare professionals should engage in open and non-judgmental discussions with patients to explore these underlying issues and identify triggers for disordered eating behaviors. By addressing these underlying issues, healthcare professionals can help patients develop healthier coping mechanisms and reduce the likelihood of relapse.
Teaching stress management techniques
Stress is a common trigger for disordered eating behaviors. Healthcare professionals should teach patients stress management techniques to help them develop healthier ways of coping with stressors. These techniques may include deep breathing exercises, progressive muscle relaxation, mindfulness meditation, or engaging in physical activity. By providing patients with effective stress management tools, healthcare professionals can support them in developing alternative coping strategies and improving their overall well-being.
Offering relapse prevention strategies
Relapse prevention is an essential aspect of managing eating disorders. Healthcare professionals should work with patients to develop relapse prevention strategies that are tailored to their specific needs and circumstances. These strategies may include regular follow-up appointments, ongoing psychoeducation, continued support from the treatment team, and involving patients in support groups or community resources. By offering relapse prevention strategies, healthcare professionals can help patients maintain their recovery journey and prevent setbacks.
Family Involvement
Assessing the family’s understanding of eating disorders
Family involvement is critical in the management of eating disorders, as the family can provide valuable support and play a significant role in the recovery process. Healthcare professionals should assess the family’s understanding of eating disorders to ensure they have accurate information and are equipped to provide appropriate support. This assessment may involve open and non-judgmental conversations with family members, providing education, and answering any questions or concerns they may have.
Educating the family about supportive behaviors
Educating the family about supportive behaviors is essential for creating a conducive environment for recovery. Healthcare professionals should provide guidance to family members on how to communicate effectively, promote positive body image, and encourage healthy eating behaviors. It’s important to emphasize the significance of empathy, patience, and non-judgmental attitudes when supporting a loved one with an eating disorder. By educating the family, healthcare professionals can enhance the patient’s support system and contribute to their overall recovery.
Addressing family dynamics and communication
Family dynamics and communication patterns can significantly impact the recovery process. Healthcare professionals should assess the family’s dynamics and identify any potential issues that may hinder the patient’s progress. By addressing and addressing these dynamics, healthcare professionals can help families develop healthier ways of communication and support. This may involve family therapy sessions, providing resources, and guiding family members in resolving conflicts or addressing underlying issues.
Providing resources for family therapy
Family therapy is an effective intervention for supporting patients with eating disorders and their families. Healthcare professionals should provide families with resources and referrals to qualified family therapists. Family therapy helps improve communication, enhance problem-solving skills, and strengthen the family’s understanding and support for the recovery process. By providing resources for family therapy, healthcare professionals can foster a collaborative and supportive approach to managing eating disorders.

Monitoring and Support
Regular assessment of eating disorder signs
Regular assessment of eating disorder signs is crucial in monitoring the progress of treatment and identifying any potential setbacks. Healthcare professionals should conduct routine assessments to evaluate factors such as weight stability, eating patterns, body image perception, and other relevant indicators. By regularly assessing eating disorder signs, healthcare professionals can modify treatment plans and interventions as needed and provide the necessary support to promote recovery.
Monitoring weight and body mass index
Monitoring weight and body mass index (BMI) is an important aspect of managing eating disorders. Healthcare professionals should track changes in weight and BMI to assess the effectiveness of nutritional interventions and the patient’s overall progress. Regular monitoring helps healthcare professionals identify abnormal weight trends and intervene if necessary. It’s important to approach weight and BMI monitoring with sensitivity and avoid placing excessive emphasis on these measurements. Instead, focus on the patient’s well-being as a whole.
Engaging in motivational interviewing
Motivational interviewing is a person-centered approach that helps patients explore and resolve ambivalence about change. Healthcare professionals can utilize motivational interviewing techniques to enhance patient motivation and engagement in their treatment. By using open-ended questions, active listening, and empathy, healthcare professionals can help patients identify their own motivations for recovery and establish goals aligned with their values. Engaging patients in motivational interviewing fosters a sense of autonomy and increases their commitment to the recovery process.
Encouraging participation in support groups
Support groups play a valuable role in the recovery journey of individuals with eating disorders. Healthcare professionals should encourage patients to participate in support groups, whether in-person or online. Support groups provide a safe, non-judgmental space for individuals to share experiences, gain support, and learn coping strategies from others who have faced similar challenges. By encouraging participation in support groups, healthcare professionals can help patients build a support network and feel less isolated in their recovery process.
Transition and Continuity of Care
Planning for transition between care settings
Transitions between care settings, such as inpatient to outpatient or from a residential program to independent living, require careful planning and coordination. Healthcare professionals should collaborate with the patient, family, and treatment team to ensure a smooth transition. This may involve developing a discharge plan, providing self-care resources, and arranging follow-up appointments and community support options. Planning for transition helps support the patient’s continued progress and prevents disruptions in care.
Ensuring a smooth handoff to outpatient care
Handing off the patient’s care from one healthcare professional to another or from an inpatient setting to outpatient care requires clear communication and coordination. Healthcare professionals should ensure that all relevant information, including assessment findings, treatment plans, and medication details, are effectively communicated to the receiving healthcare professional. This helps to ensure continuity of care and provides a seamless experience for the patient as they transition to the next phase of their treatment.
Close monitoring during the early recovery phase
Close monitoring during the early recovery phase is vital to identify potential challenges and provide the necessary support and interventions. Healthcare professionals should maintain frequent contact with patients during this period to assess their progress, identify triggers or relapse warning signs, and adjust the treatment plan as needed. Close monitoring helps to address any emerging issues in a timely manner, mitigating the risk of setbacks and optimizing the chances of successful recovery.
Collaboration with community resources
Collaboration with community resources is essential in providing ongoing support and care for individuals with eating disorders. Healthcare professionals should establish partnerships with local mental health organizations, support groups, and community-based services. These collaborations can provide patients with access to additional resources, such as counseling services, support groups, and specialized outpatient programs. Collaboration with community resources helps augment the patient’s support network and promotes continuity of care beyond the healthcare setting.
