If you or someone you know suffers from eczema, you understand the frustration and discomfort it can cause. But fear not, because in this article, we will discuss some important nursing considerations and management techniques to help you effectively manage eczema. From understanding triggers and symptoms to implementing a personalized care plan, we’ve got you covered. So sit back, relax, and get ready to learn how to tackle eczema head-on with the guidance of nursing expertise.
Assessment and Diagnosis
Identifying symptoms and triggers
As a nurse, one of your key responsibilities is to identify the symptoms of eczema in patients. This may include red, inflamed skin, intense itching, dryness, and the presence of small, raised bumps or blisters. Additionally, you should take note of any potential triggers that worsen the symptoms, such as exposure to certain fabrics, soaps, or environmental factors like pollen or pet dander.
Evaluating severity and impact on daily activities
Assessing the severity of eczema is crucial to develop an appropriate treatment plan. Determine the extent of the patient’s symptoms and how they impact their daily activities and quality of life. This evaluation will help you understand the level of care and support required, and whether the condition is mild, moderate, or severe.
Performing a physical examination
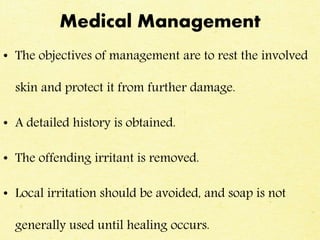
A thorough physical examination is essential to validate a diagnosis of eczema. During the examination, observe the physical manifestations of the condition, paying particular attention to areas commonly affected by eczema, such as the elbows, knees, and face. Assess the skin for signs of inflammation, cracking, or oozing, and document any visible lesions or open wounds.
Assessing the patient’s medical history
Understanding the patient’s medical history is crucial in managing eczema effectively. Inquire about any previous diagnosis of eczema, past treatments, and family history of the condition. Identifying coexisting medical conditions, allergies, or sensitivities can help pinpoint potential triggers or exacerbating factors and tailor the treatment approach accordingly.
Ruling out other skin conditions
While it is important to identify eczema, ruling out other similar skin conditions is essential to ensure an accurate diagnosis. There are various skin conditions that can mimic the symptoms of eczema, including psoriasis, contact dermatitis, or fungal infections. Thoroughly assess the patient’s skin and collaborate with the healthcare team to rule out any alternative diagnoses.
Patient Education
Explaining the nature of eczema
As a nurse, it is crucial to provide comprehensive education to patients about the nature of eczema. Explain that eczema is a chronic inflammatory skin condition characterized by flare-ups and remissions. Help patients understand that it is not contagious and can be managed effectively with proper care and treatment.
Discussing potential triggers and preventive measures
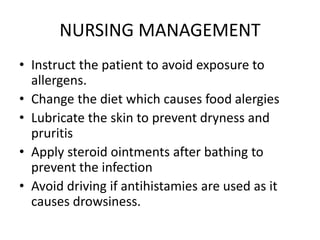
Educating patients about potential triggers and preventive measures is vital in managing eczema. Discuss common triggers such as certain fabrics, harsh soaps, allergens, or extreme weather conditions. Teach patients strategies to minimize exposure to triggers, such as using fragrance-free products, wearing cotton clothing, and maintaining a consistent skincare routine.
Teaching proper skincare techniques
Proper skincare techniques are essential in managing eczema and preventing flare-ups. Demonstrate and instruct patients on gentle cleansing using mild, fragrance-free cleansers, followed by the application of a moisturizer. Emphasize the importance of moisturizing regularly to maintain skin hydration and strengthen the skin barrier.
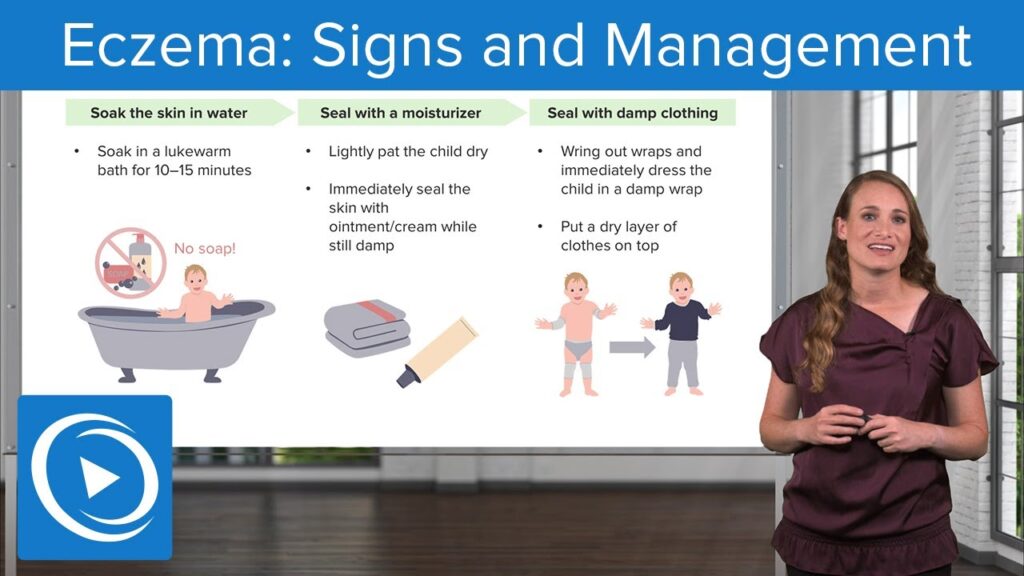
Providing guidance on bathing and moisturizing routines
Bathing and moisturizing routines play a crucial role in managing eczema. Advise patients to take lukewarm showers or baths for short durations to avoid excessive drying of the skin. Encourage them to immediately apply a moisturizer after bathing to lock in moisture. Recommend using fragrance-free and hypoallergenic products to minimize potential irritants.
Educating on the importance of avoiding irritants or allergens
Educating patients on the importance of avoiding irritants and allergens is essential in managing eczema. Emphasize the need to minimize exposure to substances that may trigger flare-ups, such as certain fabrics, harsh chemicals, or allergenic foods. Encourage patients to read labels carefully and identify potential irritants in their environment.
Treatment Options
Topical corticosteroids
Topical corticosteroids are commonly prescribed to manage eczema flare-ups. These medications help reduce inflammation and relieve itching. As a nurse, educate patients on the proper application technique, ensuring they understand the importance of following the prescribed dosage and duration of treatment. Monitor for any potential side effects, such as skin thinning or discoloration, and report them to the healthcare team.
Calcineurin inhibitors
Calcineurin inhibitors, such as tacrolimus or pimecrolimus, are alternative medications prescribed for eczema treatment. These topical medications work by suppressing the immune response in the skin, reducing inflammation. Instruct patients on proper application techniques, potential side effects, and the importance of regular follow-up appointments to assess treatment effectiveness and monitor for adverse reactions.
Moisturizers and emollients
Moisturizers and emollients form a crucial part of eczema management by restoring and maintaining skin hydration. Educate patients on the importance of selecting non-irritating, fragrance-free moisturizers and emollients. Instruct them on the correct and frequent application, emphasizing the need for consistency to prevent dryness and minimize flare-ups.
Antihistamines
Antihistamines may be recommended to manage the itching associated with eczema. These medications help alleviate the discomfort and promote better sleep, particularly in patients with severe itching. Explain the potential side effects of drowsiness or dry mouth and advise patients to follow the prescribed dosage and timing.
Immunomodulators
Immunomodulators, like dupilumab, may be prescribed for patients with moderate to severe eczema. These medications work by targeting specific immune system pathways involved in eczema flare-ups. Provide education on the administration methods, potential side effects, and the importance of long-term compliance with the prescribed treatment plan.
Systemic corticosteroids
Systemic corticosteroids may be prescribed for short-term use in severe cases of eczema, but they are not typically recommended for long-term management due to potential side effects. Educate patients on the risks and benefits of systemic corticosteroids and emphasize the need for close monitoring by the healthcare team during their use.
Medication Administration
Demonstrating proper application of topical medications
Proper application of topical medications is essential for their effectiveness. As a nurse, demonstrate the correct technique to patients, ensuring they understand the importance of applying the medication to the affected areas and avoiding excessive use. Teach them how to wash their hands before and after application to prevent inadvertent spread of the medication.
Educating on potential side effects and proper usage
Educate patients about potential side effects associated with the prescribed medications, such as skin thinning, discoloration, or allergic reactions. Discuss the importance of adherence to the prescribed dosage and duration to achieve optimal outcomes. Encourage patients to promptly report any concerning side effects to the healthcare team.
Ensuring proper dosage and adherence to prescribed regimen
Monitoring proper dosage and adherence to the prescribed regimen is crucial in managing eczema effectively. Work closely with patients to ensure they understand the prescribed dosage instructions and the frequency of medication administration. Provide tools such as pillboxes or medication reminders to enhance medication adherence.
Monitoring for adverse reactions or interactions with other medications
As a nurse, it is important to monitor patients for adverse reactions or interactions that may occur due to the prescribed medications. Regularly assess for any signs of allergic reactions, increased skin irritation, or excessive dryness. Educate patients on the importance of reporting any new symptoms or changes in their condition promptly.
Wound Care
Assessing and cleaning open lesions or areas with infection
In severe cases of eczema, open lesions or areas with infection may be present. As a nurse, assess these wound sites to determine the extent of the infection and the need for further medical intervention. Cleanse the wounds using an appropriate antiseptic solution or as per the healthcare provider’s instructions to minimize the risk of secondary infections.
Applying appropriate wound dressings
Once the wounds have been assessed and cleansed, apply appropriate wound dressings to promote healing and prevent further complications. Advise patients on proper wound care techniques and demonstrate how to change dressings appropriately. Emphasize the importance of using sterile techniques to prevent infection.
Promoting healing and preventing secondary infections
Promoting wound healing and preventing secondary infections are essential aspects of eczema management. Educate patients on proper wound care techniques, such as keeping the affected areas clean and dry, and avoiding scratching or picking at the wounds. Emphasize the importance of following the prescribed treatment plan and promptly reporting any signs of infection.
Educating on wound care techniques for self-management
Empowering patients to manage their wound care effectively is crucial for long-term management of eczema. Provide thorough education on wound care techniques, including proper cleansing, dressing changes, and recognizing signs of wound healing or infection. Encourage patients to ask questions and seek clarification, ensuring they feel confident in managing their wounds independently.
Psychosocial Support
Addressing the emotional and psychological impact of eczema
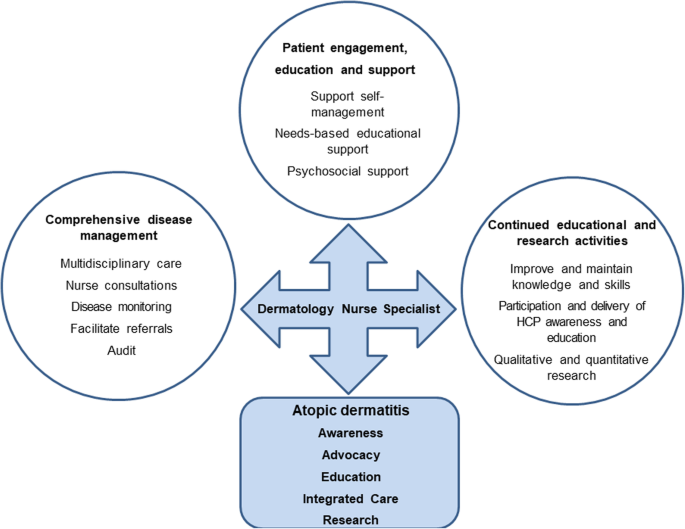
Eczema can have a significant emotional and psychological impact on patients. As a nurse, it is important to address these aspects of the condition. Provide emotional support and actively listen to patients’ concerns, validating their experiences. Offer empathy and reassurance, and emphasize that they are not alone in their journey with eczema.
Providing resources for counseling or support groups
Connecting patients with appropriate counseling or support groups can be beneficial in managing the psychosocial impact of eczema. Share relevant resources, such as local support groups or online communities, that provide emotional support, information, and practical strategies for coping with the challenges associated with eczema.
Promoting self-esteem and body positivity
Eczema can affect an individual’s self-esteem and body image. Encourage patients to appreciate their strengths beyond their skin condition and focus on their overall well-being. Promote self-acceptance and body positivity by emphasizing the importance of self-care, engaging in activities they enjoy, and surrounding themselves with supportive individuals.
Assisting with coping mechanisms and stress reduction
Stress often exacerbates eczema symptoms, so assisting patients with coping mechanisms and stress reduction techniques is essential. Teach relaxation techniques, such as deep breathing exercises or mindfulness meditation, to help manage stress. Encourage patients to engage in activities that bring them joy and relaxation, such as hobbies, exercise, or spending time with loved ones.
Managing Itch and Discomfort
Identifying triggers and implementing strategies to reduce itching
Itch is a hallmark symptom of eczema, and managing it effectively is crucial for patient comfort. Work with patients to identify potential triggers that worsen itching, such as certain fabrics or exposure to dry environments. Develop strategies to minimize exposure to triggers and implement measures to soothe and relieve itching, such as cool compresses or prescribed anti-itch creams.
Encouraging proper skincare routines to minimize discomfort
Proper skincare routines are vital in minimizing discomfort associated with eczema. Educate patients on the importance of gentle cleansing, moisturizing, and avoiding excessive scrubbing or hot water. Emphasize the need to follow prescribed treatment regimens consistently to maintain skin hydration and minimize dryness or itching.
Discussing the use of antihistamines and other itch-relieving techniques
In some cases, the use of antihistamines may be recommended to manage itching. Discuss these options with patients, explaining their potential benefits and side effects. Educate patients on the correct usage and timing of antihistamines, ensuring they understand the importance of following the prescribed dosage and consulting healthcare providers for any concerns.
Assessing the impact of itching on quality of life and adjusting treatment accordingly
Regularly assess the impact of itching on the patient’s quality of life, as it can significantly affect daily activities and sleep patterns. Collaborate with the healthcare team to determine the effectiveness of the current treatment plan and make adjustments as necessary to alleviate itching and improve overall patient comfort.
Preventing Complications
Monitoring for signs of infection or worsening of symptoms
As a nurse, it is crucial to monitor patients for signs of infection or worsening of symptoms. Educate patients on recognizing the signs of infection, such as increased redness, swelling, warmth, or drainage from wounds. Instruct them to seek immediate medical attention if any concerning symptoms arise.
Educating on proper hygiene practices
Proper hygiene practices are essential in preventing complications associated with eczema. Educate patients on the importance of maintaining good hand hygiene, especially before applying medications or touching affected areas. Instruct them to avoid sharing towels, clothing, or personal items that may exacerbate symptoms or lead to potential infections.
Encouraging regular follow-ups and adherence to treatment plans
Regular follow-up appointments play a critical role in monitoring the effectiveness of treatment and adjusting interventions as needed. Encourage patients to attend scheduled appointments and actively participate in their care. Emphasize the importance of adhering to the prescribed treatment plan to prevent complications and promote optimal outcomes.
Identifying and addressing potential triggers to prevent flare-ups
Identifying and addressing potential triggers is crucial in preventing flare-ups and managing eczema effectively. Work collaboratively with patients to identify their individual triggers, such as specific foods, environmental factors, or stressors. Educate patients on strategies to avoid or minimize exposure to triggers, and provide guidance on developing personalized coping mechanisms.
Collaboration with Healthcare Team
Communicating with dermatologists or allergists for specialized care
Collaboration with dermatologists or allergists is essential to provide specialized care for patients with eczema. Communicate effectively with these specialists, sharing relevant patient information, treatment plans, and progress updates. Seek their expertise in managing complex cases or when considering alternative therapies for patients who may require a multidisciplinary approach.
Coordinating with primary care providers for comprehensive treatment
Coordinating with primary care providers ensures comprehensive treatment and continuity of care for patients with eczema. Share relevant patient information, treatment plans, and progress updates to ensure a holistic and integrated approach to manage the condition. Act as a liaison between specialists and primary care providers to facilitate effective communication and collaboration.
Involving occupational therapists for guidance on workplace accommodations
For patients whose eczema may be aggravated in certain occupational settings, involving occupational therapists can be valuable in providing guidance on workplace accommodations. Collaborate with occupational therapists to assess the workplace environment, recommend ergonomic modifications, and provide education on skincare practices that can be integrated into the patient’s working routine.
Consulting with mental health professionals for additional support
When addressing the psychosocial impact of eczema, collaboration with mental health professionals can be beneficial in providing additional support to patients. Consulting with psychologists or counselors can help patients develop effective coping strategies, address any underlying emotional difficulties, and enhance their overall well-being.
Documentation and Follow-up
Maintaining thorough and accurate medical records
Accurate and thorough documentation is paramount in providing quality care. As a nurse, maintain detailed and organized medical records, documenting all assessments, treatments, interventions, and patient responses. Ensure that documentation adheres to legal and ethical standards, facilitating effective communication among the healthcare team.
Monitoring treatment effectiveness and modifying plans as needed
Monitoring the effectiveness of treatment is crucial to ensure optimal patient outcomes. Regularly assess patient progress, evaluating the response to interventions, and document any changes in symptoms, side effects, or quality of life. Collaborate with the healthcare team to modify treatment plans as necessary, based on the patient’s unique needs and responses.
Scheduling regular follow-up appointments
Scheduling regular follow-up appointments is essential to assess treatment effectiveness, monitor progress, and provide ongoing support. Collaborate with patients and the healthcare team to ensure that follow-up appointments are scheduled at appropriate intervals, allowing for adjustments to the treatment plan as needed.
Ensuring continuity of care during transitions between healthcare providers
Maintaining continuity of care during transitions between healthcare providers is critical in managing eczema effectively. Ensure that all necessary patient information is communicated to new healthcare providers, facilitating a seamless transfer of care. Coordinate with the healthcare team to address any potential gaps in care and ensure a smooth transition for the patient.