Are you curious about the nursing considerations and management for osteoporosis? Well, look no further! In this article, we will explore the important nursing considerations when caring for patients with osteoporosis. From understanding the risk factors to implementing preventive measures and providing appropriate support, this article will provide you with the knowledge and tools you need to effectively manage and care for individuals with this bone-weakening condition. So, grab a cup of tea and get ready to dive into the world of nursing considerations for osteoporosis!

Assessment
Medical history
In order to effectively manage osteoporosis, it is crucial to gather a comprehensive medical history from the patient. This includes information such as previous fractures, family history of osteoporosis, and any chronic medical conditions that may contribute to bone loss. The medical history also provides insight into the patient’s overall health status and can help identify potential risk factors for osteoporosis. By understanding the patient’s medical history, healthcare providers can tailor their approach to treatment and prevention to best meet the individual’s needs.
Medication review
A thorough medication review is an essential component of assessing a patient with osteoporosis. It is important to identify any medications that may contribute to bone loss or increase the risk of fractures. Certain medications, such as glucocorticoids, anticonvulsants, and some cancer treatments, have been shown to have negative effects on bone density. By reviewing the patient’s current medication regimen, healthcare providers can make informed decisions about the most appropriate treatment options and potential adjustments to the patient’s medications.
Bone density testing
Bone density testing, commonly done through a dual-energy x-ray absorptiometry (DEXA) scan, is the gold standard for diagnosing osteoporosis and assessing fracture risk. This non-invasive test measures the mineral density of the bones, typically in the hip and spine. The results of the bone density test can help guide treatment decisions and provide a baseline for monitoring response to therapy. It is recommended that postmenopausal women, men over 50 years old, and individuals with risk factors for osteoporosis undergo bone density testing.
Physical examination
A thorough physical examination is important in assessing a patient with osteoporosis. The physical examination provides valuable information about the patient’s overall health, functional status, and potential musculoskeletal abnormalities. Healthcare providers should pay particular attention to signs of kyphosis (abnormal curvature of the spine), as this can be indicative of vertebral fractures. Additionally, examination of the patient’s gait and balance can help identify any deficits that may increase the risk of falls and subsequent fractures. By conducting a comprehensive physical examination, healthcare providers can gather important data that will inform their management of the patient’s osteoporosis.
Patient Education
Risk factors for osteoporosis
Educating patients about the risk factors for osteoporosis is crucial for both prevention and management of the disease. Risk factors include advancing age, female gender, a family history of osteoporosis, low body weight, smoking, excessive alcohol consumption, and certain chronic medical conditions (such as rheumatoid arthritis and chronic kidney disease). By understanding these risk factors, patients can make lifestyle modifications and take steps to minimize their risk of developing osteoporosis or suffering from fractures.
Importance of diet and exercise
Proper nutrition and regular exercise play a vital role in maintaining strong and healthy bones. It is important to educate patients on the importance of a balanced diet rich in calcium and vitamin D, as these nutrients are essential for bone health. Encouraging patients to consume foods such as dairy products, leafy greens, and fortified cereals can help ensure an adequate intake of calcium and vitamin D. Additionally, regular weight-bearing exercises, such as walking and dancing, can help improve bone density and reduce the risk of fractures. By emphasizing the importance of diet and exercise, healthcare providers can empower patients to take an active role in their bone health.
Fall prevention
As osteoporosis increases the risk of fractures, fall prevention is a key component of managing the disease. Patients should be educated on strategies to minimize the risk of falls, such as removing tripping hazards in the home, using handrails on stairs, and wearing appropriate footwear. Additionally, patients should be reminded to take precautions when walking on slippery surfaces and to use assistive devices if necessary. By providing education and guidance on fall prevention, healthcare providers can help reduce the risk of fractures and improve patient outcomes.
Medication adherence
Medication adherence is crucial in the management of osteoporosis. Patients should be educated on the importance of taking their prescribed medications as directed and any potential side effects or drug interactions to be aware of. Healthcare providers can offer strategies to improve medication adherence, such as pill organizers, reminder systems, and regular follow-up appointments to monitor the patient’s progress. By emphasizing the importance of medication adherence, healthcare providers can support patients in maximizing the benefits of their prescribed treatments.
Nutrition
Importance of calcium and vitamin D intake
Calcium and vitamin D are essential nutrients for maintaining strong and healthy bones. Calcium is the primary mineral found in bones, and vitamin D plays a crucial role in the absorption and utilization of calcium. Educating patients on the importance of adequate calcium and vitamin D intake is essential for preventing and managing osteoporosis. Calcium-rich foods include dairy products, leafy greens, and fortified cereals, while vitamin D can be obtained through sunlight exposure and dietary sources such as fatty fish and fortified products.
Dietary sources of calcium and vitamin D
In addition to educating patients about the importance of calcium and vitamin D, it is important to provide information on dietary sources of these nutrients. This can encourage patients to make healthy food choices and ensure they are getting an adequate intake of calcium and vitamin D. By incorporating calcium-rich foods into the diet, such as milk, yogurt, and cheese, patients can increase their calcium intake. Similarly, foods high in vitamin D, such as salmon, sardines, and fortified dairy products, can help meet the body’s vitamin D requirements.
Nutritional supplements
In some cases, it may be necessary for patients to supplement their diet with nutritional supplements to ensure they are getting an adequate intake of calcium and vitamin D. Healthcare providers should assess the patient’s dietary intake and, if necessary, recommend supplements to meet their specific needs. Calcium supplements are available in various forms, such as calcium carbonate and calcium citrate, and can be taken with or without food. Vitamin D supplements, typically in the form of vitamin D3, are also available and may be recommended depending on the patient’s individual circumstances.
Exercise
Weight-bearing exercises
Weight-bearing exercises are an integral part of managing osteoporosis and improving bone density. These exercises involve bearing the weight of the body against gravity, such as walking, dancing, or climbing stairs. Weight-bearing exercises stimulate bone remodeling and help prevent bone loss. Patients should be encouraged to engage in weight-bearing exercises for at least 30 minutes a day, most days of the week. Healthcare providers can provide guidance on appropriate exercises based on the patient’s individual fitness level and any specific limitations they may have.
Resistance training
In addition to weight-bearing exercises, resistance training is important for maintaining and building muscle strength. This form of exercise involves using external resistance, such as weights or resistance bands, to challenge the muscles. Resistance training can help improve balance and stability, reducing the risk of falls and subsequent fractures. Patients should be encouraged to incorporate resistance training exercises into their routine, focusing on major muscle groups and performing 2-3 sessions per week. Healthcare providers can provide guidance on proper form and technique to maximize the benefits of resistance training.
Balance and coordination exercises
Maintaining good balance and coordination is crucial for preventing falls and fractures in patients with osteoporosis. Balance and coordination exercises, such as yoga or tai chi, can help improve stability and reduce the risk of falls. These exercises focus on body awareness, flexibility, and mindfulness. Patients should be encouraged to participate in balance and coordination exercises at least 2-3 times per week, in addition to other forms of exercise. By incorporating these exercises into their routine, patients can improve their overall balance and reduce their risk of falls.
Safe exercise guidelines
When prescribing exercise for patients with osteoporosis, it is important to provide safe exercise guidelines to minimize the risk of injury. Patients should be advised to start slowly and gradually increase the intensity and duration of their exercise routine. It is also important to emphasize the importance of proper form and technique, as incorrect movements can increase the risk of fractures. Patients should listen to their bodies and modify exercises as needed to avoid pain or discomfort. healthcare providers can provide specific recommendations and modifications based on the patient’s individual needs and limitations.
Medication Management
Review of medication regimen
A comprehensive review of the patient’s medication regimen is necessary to ensure optimal management of osteoporosis. This includes assessing the patient’s current medications, including over-the-counter and herbal supplements, to identify any potential interactions or contraindications. Healthcare providers should also evaluate the patient’s comorbidities and consider any medications that may contribute to bone loss. By reviewing the medication regimen, healthcare providers can make informed decisions regarding the most appropriate osteoporosis treatments and potential adjustments to the patient’s medications.
Bisphosphonates
Bisphosphonates are the most commonly prescribed medications for the treatment of osteoporosis. These medications work by inhibiting bone resorption, helping to maintain bone density and reduce the risk of fractures. Commonly prescribed bisphosphonates include alendronate, risedronate, and ibandronate. Healthcare providers should educate patients on the correct administration and potential side effects of bisphosphonates. It is important for patients to take these medications as directed, usually on an empty stomach with a full glass of water, and to remain upright for at least 30 minutes to minimize the risk of esophageal erosion.
Selective estrogen receptor modulators
Selective estrogen receptor modulators (SERMs) are another class of medications used in the treatment of osteoporosis. These medications work by binding to estrogen receptors in the body, mimicking some of the effects of estrogen. SERMs, such as raloxifene, help to maintain bone density and reduce the risk of fractures. Healthcare providers should educate patients about the benefits and potential risks of SERMs, including an increased risk of blood clots. It is important for patients to be aware of the potential side effects and to discuss any concerns with their healthcare provider.
Calcitonin
Calcitonin is a hormone that helps regulate calcium levels in the body. It is available as a nasal spray or an injection and is used in the treatment of osteoporosis to help reduce bone loss and the risk of fractures. Healthcare providers should educate patients on the proper administration and potential side effects of calcitonin. Patients should be aware that calcitonin may cause nasal irritation or flushing and should follow the instructions for use provided by their healthcare provider.
Teriparatide
Teriparatide is a medication used in the treatment of severe osteoporosis. It is a synthetic form of parathyroid hormone that helps stimulate bone remodeling and increase bone density. Teriparatide is given as a daily injection and is typically used for a limited duration due to safety concerns. Healthcare providers should educate patients on the proper administration and potential side effects of teriparatide. Patients should be aware of the potential risks associated with long-term use and should discuss any concerns with their healthcare provider.
Denosumab
Denosumab is a medication that helps reduce the risk of fractures by inhibiting the activity of cells that break down bone. It is given as an injection every six months and is an alternative treatment for patients who are unable to tolerate bisphosphonates or other osteoporosis medications. Healthcare providers should educate patients on the proper administration and potential side effects of denosumab. Patients should be aware of the potential risks, including an increased risk of infection, and should promptly report any signs of illness or infection to their healthcare provider.
Fall Prevention
Assessment of fall risk
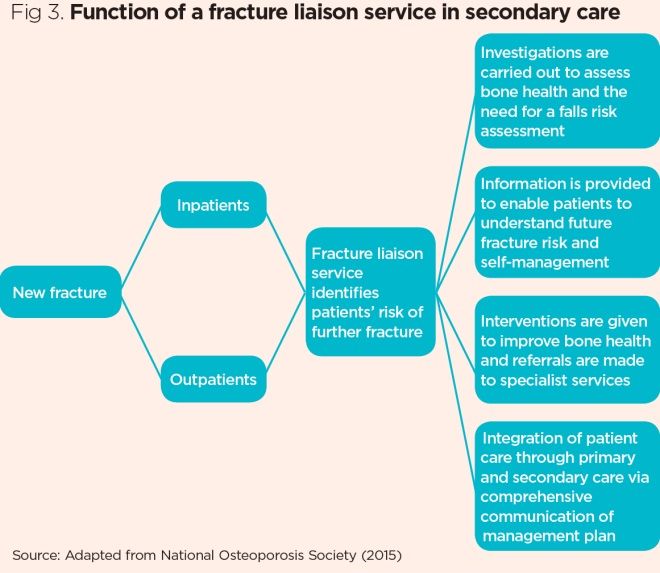
Assessing a patient’s risk of falls is crucial in the management of osteoporosis. Healthcare providers should conduct a thorough assessment to identify factors that may increase the patient’s risk of falling, such as muscle weakness, gait abnormalities, balance deficits, vision impairments, and environmental hazards. Special attention should be given to patients with a history of falls, as they are at increased risk of subsequent fractures. By identifying and addressing these risk factors, healthcare providers can implement appropriate interventions to reduce the risk of falls and improve patient safety.
Environmental modifications
Making modifications to the patient’s environment can significantly reduce the risk of falls. This may include removing tripping hazards, such as loose rugs or clutter, ensuring adequate lighting throughout the home, installing grab bars in bathrooms and stairways, and using non-slip mats or adhesive strips in the shower or bathtub. It is important to educate patients and their families about the importance of maintaining a safe and hazard-free environment. Assessing the patient’s home and providing specific recommendations for modifications can help prevent falls and promote independence.
Use of assistive devices
For patients at high risk of falls, the use of assistive devices can provide added support and stability. Examples of assistive devices include canes, walkers, and stairlifts. Healthcare providers should assess the patient’s needs and provide appropriate recommendations for assistive devices. It is essential to ensure that the patient is properly trained in the correct use of the device and that it is properly adjusted to their specific needs. By providing patients with the necessary assistive devices, healthcare providers can help minimize the risk of falls and promote safe mobility.
Educating patients on fall prevention
Education plays a crucial role in fall prevention for patients with osteoporosis. Patients should be educated on the importance of maintaining a safe environment and encouraged to take proactive steps to reduce their risk of falls. Important topics to cover include the use of appropriate footwear, strategies for navigating stairs safely, and the importance of exercise and rehabilitation programs to improve balance and strength. By providing patients with the necessary tools and knowledge, healthcare providers can empower them to take an active role in fall prevention and reduce their risk of fractures.
Pain Management
Assessment and documentation of pain
Assessing and managing pain is an important aspect of nursing care for patients with osteoporosis. Patients may experience pain as a result of fractures or musculoskeletal abnormalities associated with the disease. It is important for healthcare providers to assess the patient’s pain level and characteristics, as well as its impact on their daily activities and quality of life. Pain should be documented using validated pain assessment tools, and the patient’s response to pain management interventions should be regularly evaluated. By effectively assessing and documenting pain, healthcare providers can tailor their interventions to meet the patient’s individual needs.
Non-pharmacological interventions
Non-pharmacological interventions can be effective in managing pain in patients with osteoporosis. These interventions include heat or cold therapy, therapeutic exercises, massage, acupuncture, and transcutaneous electrical nerve stimulation (TENS). Healthcare providers should educate patients on these non-pharmacological interventions and encourage their use as adjuncts to pain medication. It is important for patients to understand the proper techniques for these interventions and to consult with their healthcare provider before starting any new treatments.
Analgesic medications
Medication management is an important component of pain management in patients with osteoporosis. Analgesic medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to help manage pain. It is important for healthcare providers to educate patients on the proper use of these medications, including dosing, potential side effects, and the importance of following up with their healthcare provider regularly. Patients should be encouraged to use these medications as prescribed and to report any side effects or concerns to their healthcare provider.
Monitoring and Follow-up
Regular bone density screenings
Regular bone density screenings are important for monitoring the progression of osteoporosis and assessing treatment effectiveness. The frequency of screenings will depend on the patient’s individual risk factors and treatment plan. Typically, bone density screenings are recommended every 1-2 years for individuals with osteoporosis or those at high risk of fractures. By monitoring bone density over time, healthcare providers can make informed decisions regarding adjustments to the patient’s treatment plan and provide appropriate recommendations for lifestyle modifications.
Evaluation of treatment effectiveness
Evaluating the effectiveness of osteoporosis treatment is crucial for optimizing patient outcomes. Healthcare providers should regularly assess the patient’s response to treatment, including improvements in bone density, reduction in fracture risk, and alleviation of symptoms. This can be done through follow-up bone density screenings, evaluation of the patient’s medical history and physical examination findings, and assessment of the patient’s adherence to their prescribed treatment plan. By regularly evaluating treatment effectiveness, healthcare providers can make necessary adjustments to the patient’s management plan and ensure the best possible outcomes.
Assessment of medication side effects
It is important for healthcare providers to assess for potential side effects of osteoporosis medications and to monitor the patient for any adverse reactions. Common side effects of medications used to treat osteoporosis include gastrointestinal symptoms, flu-like symptoms, and musculoskeletal pain. Healthcare providers should educate patients on the potential side effects of their prescribed medications and instruct them to report any new or worsening symptoms. Regular follow-up appointments and open communication with the patient can facilitate early detection and management of medication side effects.
Collaboration with Interdisciplinary Team
Consultation with physical therapist
Collaboration with a physical therapist can greatly benefit patients with osteoporosis. Physical therapists are experts in developing individualized exercise programs to improve strength, balance, and mobility. They can provide guidance on proper exercise technique, safety precautions, and modifications for patients with specific limitations. Healthcare providers should refer patients to physical therapy for comprehensive evaluation and development of a personalized exercise program. By collaborating with physical therapists, healthcare providers can enhance the effectiveness of their management of osteoporosis and improve patient outcomes.
Referral to dietitian
Referral to a dietitian can be beneficial for patients with osteoporosis, particularly those who may have dietary deficiencies or specific nutritional needs. Dietitians can assess the patient’s current dietary intake and provide recommendations for an optimal diet to support bone health. They can educate patients on the importance of a balanced diet rich in calcium and vitamin D and guide them in making appropriate food choices. By involving dietitians in the management of osteoporosis, healthcare providers can ensure that patients receive comprehensive nutritional support to maximize the benefits of their treatment.
Coordination with primary care physician
Coordination with the patient’s primary care physician is essential in managing osteoporosis. The primary care physician plays a key role in overseeing the patient’s overall health and managing any comorbidities that may affect bone health. Healthcare providers should communicate with the primary care physician to share pertinent information, including medication changes, treatment plans, and any new findings from assessments or screenings. By coordinating care with the primary care physician, healthcare providers can ensure that the patient receives comprehensive and cohesive management of their osteoporosis.
Patient Support and Advocacy
Emotional support
Patients with osteoporosis may experience emotional distress related to the diagnosis, fear of fractures, and the impact of the disease on their daily lives. Providing emotional support is an important aspect of nursing care for these patients. Healthcare providers should take the time to listen to patient concerns, validate their feelings, and provide reassurance. Offering counseling or referrals to support groups can also be beneficial in helping patients cope with the emotional aspects of osteoporosis. By providing emotional support, healthcare providers can promote overall well-being and improve patient outcomes.
Connecting patients with community resources
Connecting patients with community resources can provide valuable support and assistance in managing osteoporosis. These resources may include local support groups, educational materials, exercise programs, or other community-based initiatives dedicated to bone health. Healthcare providers should take the time to educate patients about these resources and encourage their participation. By connecting patients with community resources, healthcare providers can empower them to take an active role in managing their condition and improve their overall quality of life.
Advocating for patient autonomy and informed decision-making
Advocating for patient autonomy and informed decision-making is an integral part of nursing care for patients with osteoporosis. Patients have the right to be fully informed about their condition and treatment options and to actively participate in decision-making regarding their care. This involves providing patients with clear and understandable information, discussing the risks and benefits of treatment options, and involving them in the development of their individualized management plan. By advocating for patient autonomy, healthcare providers can empower patients and facilitate their active engagement in their own care.

