You’re in for an informative read as we explore the crucial nursing considerations and management strategies for Paragonimiasis. This article will highlight the key points that every nurse should keep in mind when caring for patients with this parasitic infection. From understanding the causes and symptoms to implementing effective treatment plans, we’ll cover it all. So grab a cup of coffee, sit back, and get ready to enhance your nursing knowledge!
Assessment
Signs and Symptoms
When assessing a patient with paragonimiasis, it is important to be aware of the signs and symptoms associated with this parasitic infection. Common signs and symptoms include cough that may produce blood-streaked sputum, chest pain, shortness of breath, and fever. Other symptoms may include fatigue, weight loss, and abdominal pain. It is important to thoroughly assess the patient’s respiratory and gastrointestinal systems for any abnormalities.
Medical History
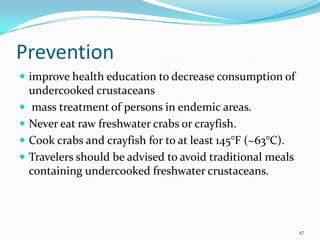
Obtaining a detailed medical history is crucial in managing a patient with paragonimiasis. This includes gathering information about the patient’s travel history, as paragonimiasis is commonly acquired in regions where the parasite is endemic. Additionally, it is important to inquire about any exposure to raw or undercooked freshwater crustaceans, such as crabs or crayfish, as these are common sources of infection. Gathering information about the duration and progression of symptoms is also important in order to provide appropriate care and treatment.
Physical Examination
A thorough physical examination is essential in assessing a patient with paragonimiasis. The nurse should focus on respiratory and abdominal assessments. Auscultation of the lungs may reveal crackles or wheezing, indicating pulmonary involvement. The abdomen should be carefully palpated for tenderness or organ enlargement, as the parasite can cause abdominal symptoms. The nurse should also assess for any signs of malnutrition or weight loss, as paragonimiasis can lead to nutritional deficiencies.
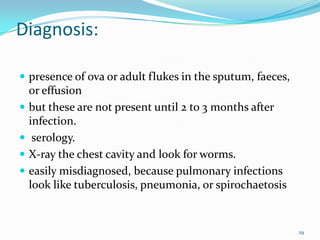
Diagnostic Tests
Several diagnostic tests may be utilized to confirm the presence of paragonimiasis. A sputum sample may be obtained and examined for the presence of parasite eggs. Imaging studies, such as chest X-ray or computed tomography (CT) scan, may be performed to assess the extent of lung involvement and identify any characteristic findings, such as pulmonary infiltrates or pleural effusion. In some cases, a bronchoscopy or lung biopsy may be necessary to obtain a definitive diagnosis.
Planning and Implementation
Collaborative Care
Collaborative care is essential in managing patients with paragonimiasis. The healthcare team should include physicians, nurses, and other healthcare professionals who work together to ensure comprehensive care for the patient. Collaborative care may involve consulting with a specialist, such as a pulmonologist or infectious disease specialist, to guide the appropriate treatment and management strategies.
Patient Education
Patient education is pivotal in managing paragonimiasis. The nurse should provide comprehensive education to the patient and their family regarding the nature of the infection, its transmission, and prevention strategies. It is important to emphasize the avoidance of raw or undercooked freshwater crustaceans, as well as proper food handling and preparation techniques. The importance of completing the prescribed treatment regimen should also be emphasized to ensure successful recovery.
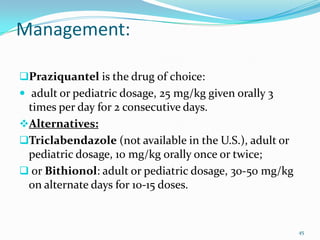
Medication Administration
Medication administration plays a crucial role in the management of paragonimiasis. The primary treatment for paragonimiasis is the use of antiparasitic medications, such as praziquantel or triclabendazole. The nurse should ensure that the medications are administered at the prescribed doses and time intervals. It is important to closely monitor the patient for any adverse effects or allergic reactions to the medications.
Nutritional Support
Paragonimiasis can lead to malnutrition and weight loss in affected individuals. Therefore, nutritional support is an important aspect of nursing care. The nurse should collaborate with a registered dietitian to develop a nutrition plan that addresses the patient’s specific needs. This may involve providing a well-balanced diet rich in protein, vitamins, and minerals. In severe cases, enteral or parenteral nutrition may be necessary to ensure adequate nutrient intake.
Fluid and Electrolyte Balance
Patients with paragonimiasis may experience fluid and electrolyte imbalances due to symptoms such as diarrhea, vomiting, and fever. The nurse should closely monitor the patient’s intake and output, as well as electrolyte levels. If necessary, intravenous fluids may be administered to maintain proper hydration and electrolyte balance. Regular assessment of vital signs and fluid status is important to guide appropriate interventions.
Respiratory Support
In severe cases of paragonimiasis, respiratory support may be necessary. The nurse should monitor the patient’s oxygenation and respiratory status closely. Administration of supplemental oxygen or respiratory therapies, such as nebulization or chest physiotherapy, may be required to improve respiratory function. It is important to provide adequate support and reassurance to the patient, as respiratory involvement can significantly impact their quality of life.
Pain Management
Pain management is an integral part of nursing care for patients with paragonimiasis. The nurse should assess the patient’s pain levels regularly and administer appropriate pain medications as prescribed. Non-pharmacological pain management techniques, such as relaxation exercises or heat therapy, may also be utilized to alleviate discomfort. It is important to provide emotional support and reassurance to the patient, as pain can significantly affect their well-being.
Prevention of Complications
Preventing complications is paramount in managing paragonimiasis. The nurse should closely monitor the patient for any signs of worsening symptoms or development of complications, such as respiratory distress or pleural effusion. Prompt intervention and appropriate management strategies should be implemented to prevent further deterioration of the patient’s condition. Additionally, educating the patient about the importance of seeking medical care for any new or worsening symptoms is crucial in preventing complications.

Evaluation
Monitoring Treatment Effectiveness
Regular evaluation of the patient’s response to treatment is essential in managing paragonimiasis. The nurse should monitor the patient’s symptoms, such as cough, chest pain, and shortness of breath, to assess the effectiveness of the prescribed antiparasitic medications. Imaging studies, such as chest X-rays or CT scans, may be repeated to evaluate any changes in lung involvement. Monitoring laboratory values, such as sputum examination for parasite eggs, can also provide valuable information about treatment effectiveness.
Assessing Patient Response to Therapy
In addition to monitoring treatment effectiveness, it is important to assess the patient’s overall response to therapy. The nurse should assess the patient’s quality of life, functional status, and ability to perform activities of daily living. Improvement in respiratory symptoms, nutritional status, and well-being are important indicators of positive response to therapy. The patient’s feedback and self-reporting should be taken into consideration when evaluating treatment outcomes.
Evaluating Patient’s Understanding of Educational Materials
Evaluation of the patient’s understanding of educational materials is crucial in managing paragonimiasis. The nurse should assess the patient’s knowledge and comprehension of the infection, its transmission, and preventive measures. This can be done through verbal or written assessments, such as quizzes or discussions. Any knowledge gaps or misconceptions should be addressed promptly to ensure that the patient has a clear understanding of the infection and its management.
In conclusion, nursing considerations for paragonimiasis are multifaceted and require a comprehensive approach. Through thorough assessment, collaborative care, patient education, appropriate medication administration, nutritional support, and proactive monitoring and evaluation, nurses can play a vital role in managing paragonimiasis and promoting the health and well-being of affected individuals.