Psoriatic arthritis can present unique challenges for those living with the condition, and as a nurse, it is important to understand the specific nursing considerations and management strategies for individuals with this condition. From assessing the severity of symptoms and monitoring for potential complications to providing education and support, nurses play a crucial role in helping patients navigate the complexities of psoriatic arthritis. This article aims to provide nurses with a comprehensive overview of the nursing considerations and management strategies necessary to provide high-quality care for patients with psoriatic arthritis.
Assessment
Assessing Symptoms
In order to effectively manage and treat psoriatic arthritis (PsA), it is crucial to assess the patient’s symptoms thoroughly. Common symptoms of PsA include joint pain, stiffness, swelling, and redness. It is important to ask the patient about the location, intensity, and duration of their joint pain. Additionally, inquire about any skin symptoms, such as psoriasis plaques, which may indicate PsA. Assessing symptoms helps in accurately diagnosing PsA and creating an individualized treatment plan.
Evaluating Joint Involvement
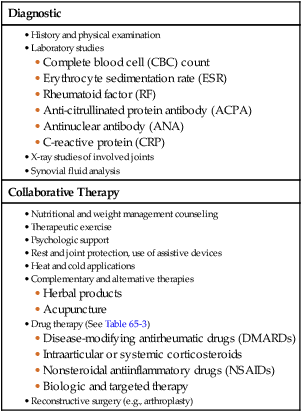
When assessing a patient with PsA, it is essential to evaluate the extent and severity of joint involvement. This includes assessing the number of affected joints, as well as the degree of inflammation and deformity. Perform a thorough physical examination, palpating each joint and assessing range of motion. Radiographic imaging, such as X-rays or MRI scans, may be useful in determining the extent and severity of joint damage. Evaluating joint involvement assists in determining the appropriate treatment strategies and monitoring disease progression.
Assessing Psoriasis Severity
PsA is often associated with psoriasis, a chronic skin condition characterized by red, scaly patches. Assessing the severity of psoriasis in patients with PsA is essential in determining the overall disease burden and selecting appropriate treatment options. Use standardized tools, such as the Psoriasis Area and Severity Index (PASI) or the Body Surface Area (BSA), to quantify the severity of psoriasis. Performing regular skin assessments and documenting the severity of psoriasis helps in monitoring treatment effectiveness and adjusting therapy as needed.
Assessing Impact on Daily Activities
PsA can significantly impact a patient’s ability to carry out daily activities, such as dressing, bathing, or performing household tasks. Assess the patient’s functional abilities and limitations using tools like the Health Assessment Questionnaire (HAQ) or the Disability Index of the Health Assessment Questionnaire (HAQ-DI). These assessments provide valuable information on the impact of PsA on the patient’s quality of life and assist in developing tailored interventions to improve daily functioning.
Planning
Setting Realistic Goals
When planning the care of a patient with PsA, it is important to set realistic goals that focus on improving the patient’s overall well-being and quality of life. Collaborate with the patient to identify their individual goals and aspirations. These goals may include reducing pain, improving joint mobility, or managing psoriasis symptoms. Setting realistic goals helps guide the treatment process and ensures that the patient’s needs and desires are addressed.
Collaborative Care Planning
PsA is a chronic condition that requires a multidisciplinary approach to care. Collaborate with other healthcare professionals, such as rheumatologists, physical therapists, and occupational therapists, to develop a comprehensive care plan for the patient. Regularly communicate and exchange information with the healthcare team to ensure coordinated and holistic care. Collaborative care planning ensures that all aspects of the patient’s health and well-being are addressed effectively.
Education and Coping Strategies
Educating the patient about PsA and providing coping strategies are essential components of the nursing management of PsA. Provide information about the condition, its potential complications, and available treatment options. Teach the patient strategies to manage pain, such as relaxation techniques or heat and cold therapy. Additionally, provide emotional support and refer the patient to mental health professionals if needed. Education and coping strategies empower the patient to actively participate in their care and better manage their symptoms.
Implementation
Pharmacological Interventions
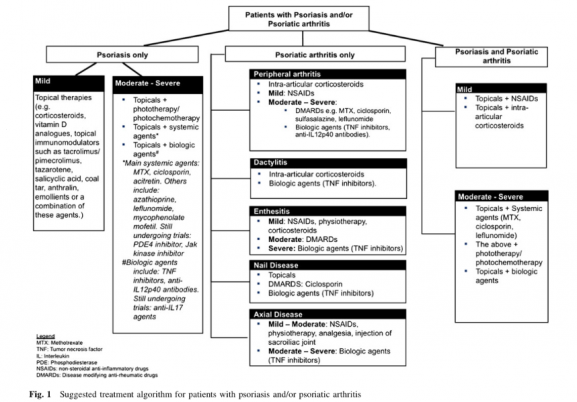
Pharmacological interventions play a key role in the management of PsA. Non-steroidal anti-inflammatory drugs (NSAIDs) are often prescribed to reduce joint pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) are used to slow down disease progression and preserve joint function. Biologic response modifiers, such as tumor necrosis factor (TNF) inhibitors, target specific molecules involved in inflammation and are effective in treating PsA. Corticosteroids may be prescribed for short-term symptom relief. It is crucial to educate patients about the potential benefits and side effects of these medications, as well as monitor their response to treatment closely.
Patient Education and Self-Management
Empowering patients with knowledge and skills to manage their condition is a vital aspect of nursing care for PsA. Provide education on self-care strategies, including joint protection techniques, proper body mechanics, and exercises that promote joint flexibility and strength. Teach patients about the importance of medication adherence and the potential side effects of their medications. Additionally, encourage patients to keep a symptom diary to track changes in their condition and discuss any concerns with their healthcare team.
Promoting Physical Activity
Regular physical activity is beneficial for patients with PsA as it helps maintain joint flexibility, strengthens muscles, and improves overall well-being. Assess the patient’s current physical activity levels and collaborate with a physical therapist to develop an individualized exercise plan. Encourage activities such as swimming, cycling, or low-impact exercises that are gentle on the joints. Monitor exercise tolerance and progress closely, adjusting the exercise plan as needed. Promoting physical activity supports the management and overall health of patients with PsA.
Pain Management Techniques
Pain management is a crucial aspect of nursing care for patients with PsA. Assess and document the patient’s pain using a standardized pain scale. Use non-pharmacological pain relief strategies, such as cold or heat therapy, transcutaneous electrical nerve stimulation (TENS), or relaxation techniques. Administer analgesics as prescribed, carefully monitoring their effects and any potential side effects. Regularly reassess the patient’s pain levels and adjust pain management strategies accordingly.
Assistive Devices and Adaptive Aids
For patients with PsA experiencing joint pain and limited mobility, assistive devices and adaptive aids can greatly improve their daily functioning and quality of life. Collaborate with an occupational therapist to assess the patient’s needs and recommend appropriate aids, such as canes, walkers, or splints. Educate the patient on how to properly use and maintain these devices. Assistive devices and adaptive aids provide support and enable patients to engage in daily activities with less pain and difficulty.
Evaluation
Monitoring Treatment Effectiveness
Regularly monitor the patient’s response to treatment to evaluate its effectiveness in managing PsA symptoms. Assess joint pain, stiffness, range of motion, and skin involvement. Use validated outcome measures, such as the Disease Activity Score (DAS) or the Psoriatic Arthritis Response Criteria (PsARC), to objectively evaluate treatment response. Adjust the treatment plan as needed based on the patient’s progress and feedback.
Assessing Adherence to Medication Regimens
Medication adherence is crucial for a successful PsA treatment outcome. Regularly assess the patient’s adherence to medication regimens, discussing any barriers they may encounter, such as side effects or forgetfulness. Explore strategies to improve adherence, such as simplifying medication schedules or reminder systems. Collaborate with the healthcare team to address any adherence challenges and optimize the patient’s treatment.
Evaluating Patient’s Understanding and Compliance
Assess the patient’s understanding of their condition and treatment plan. Ask open-ended questions and encourage them to express any concerns or misconceptions. Use teach-back techniques to ensure the patient comprehends the information provided. Regularly evaluate the patient’s compliance with the prescribed self-care strategies, such as exercise routines, joint protection techniques, and medication adherence. Providing ongoing education and reinforcement can enhance patients’ understanding and compliance with their PsA management.
Monitoring for Potential Complications
Patients with PsA may experience complications such as joint damage, deformities, or comorbidities like cardiovascular disease or metabolic syndrome. Regularly monitor for signs and symptoms of these complications, such as increased joint pain, physical limitations, or cardiovascular risk factors. Collaborate with the healthcare team to promptly address and manage any potential complications that arise. Monitoring for potential complications helps in providing appropriate interventions and optimizing the patient’s overall health.
Collaboration and Communication
Interprofessional Collaboration
Collaboration with other healthcare professionals, such as rheumatologists, physical therapists, and occupational therapists, is essential in providing holistic care for patients with PsA. Regularly communicate and exchange information with the healthcare team to ensure coordinated care. Collaborate in developing care plans, discussing treatment options, and addressing any concerns or challenges. Interprofessional collaboration enhances the quality of care and promotes positive patient outcomes.
Patient and Family Communication
Effective communication with patients and their families is crucial in nursing management for PsA. Provide information about the patient’s condition, treatment options, and self-management strategies in a clear and understandable manner. Encourage patients and their families to ask questions and express their concerns. Foster a supportive and empathetic environment that promotes open dialogue. Effective communication helps patients and their families actively participate in their care and make informed decisions.
Referrals to Specialty Clinics
Patients with PsA may require specialized care and interventions, such as joint injections, orthopedic consultations, or dermatology referrals for severe psoriasis. Identify the need for specialty referrals based on the patient’s condition and collaborate with the healthcare team to facilitate timely referrals. Regularly communicate and follow up with the specialty clinics to ensure coordinated care and optimal patient outcomes.
Utilizing Technology for Remote Monitoring
Technology can be a valuable tool in the nursing management of PsA, particularly for remote monitoring and patient education. Utilize telehealth platforms to conduct virtual follow-up visits, monitor treatment response, and provide ongoing education. Explore the use of mobile applications or wearable devices to track symptoms, medication adherence, or physical activity levels. Applying technology in the management of PsA enhances accessibility and engagement in care, particularly for patients in remote or underserved areas.
Pain Management
Assessing and Documenting Pain
Pain assessment is essential for effective pain management in patients with PsA. Use validated pain assessment tools, such as the Numeric Rating Scale (NRS) or the Visual Analog Scale (VAS), to assess the intensity and characteristics of the patient’s pain. Document the pain scores regularly to monitor changes over time. Assessing and documenting pain provides a basis for individualized pain management interventions and helps in evaluating the effectiveness of interventions.
Non-Pharmacological Pain Relief Strategies
Non-pharmacological pain relief strategies can complement pharmacological interventions in managing pain for patients with PsA. These strategies include heat and cold therapy, massage, acupuncture, relaxation techniques, and guided imagery. Collaborate with the patient to identify and implement the most effective non-pharmacological pain relief strategies. Educate the patient on how to use these techniques and provide resources for additional support.
Administering Analgesics
Analgesics play a crucial role in managing pain for patients with PsA. Non-opioid analgesics such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used for mild to moderate pain. Opioid analgesics may be considered for severe pain that is unresponsive to other measures. Administer analgesics as prescribed, carefully monitoring the patient’s response and any potential side effects. Regularly reassess the patient’s pain levels and adjust the analgesic regimen as needed.
Monitoring Analgesic Effects and Side Effects
Regularly assess and monitor the effectiveness of analgesics in managing the patient’s pain. Evaluate pain scores before and after medication administration to determine the analgesic’s efficacy. Additionally, closely monitor for potential side effects of analgesics, such as gastrointestinal bleeding with NSAIDs or respiratory depression with opioids. Educate the patient about the importance of reporting any side effects promptly. Monitoring analgesic effects and side effects ensures that pain is effectively managed, and the patient’s safety and well-being are maintained.
Psychosocial Support
Assessing Emotional Well-being
PsA can have a significant impact on a patient’s emotional well-being due to the chronic nature of the condition and its impact on daily functioning. Regularly assess the patient’s emotional well-being using standardized tools, such as the Patient Health Questionnaire (PHQ-9) or the Generalized Anxiety Disorder (GAD-7) scale. Address any signs of depression, anxiety, or other emotional distress promptly. Identifying and addressing emotional well-being facilitates holistic nursing care and enhances overall patient outcomes.
Providing Emotional Support
Emotional support plays a crucial role in the nursing management of patients with PsA. Acknowledge the patient’s emotional struggles and create a supportive environment where they feel comfortable expressing their emotions. Actively listen to their concerns and fears, offer reassurance, and provide coping strategies. Encourage the patient to engage in support groups or individual counseling if needed. Providing emotional support contributes to the patient’s overall well-being and improves their ability to cope with the challenges of living with PsA.
Identifying Coping Mechanisms
Identify the patient’s existing coping mechanisms and explore additional strategies to enhance their ability to cope with the challenges of PsA. Encourage the patient to engage in activities they enjoy, such as hobbies, exercise, or spending time with loved ones. Teach stress management techniques, such as deep breathing exercises or mindfulness meditation. Collaborate with the healthcare team to provide additional resources or referrals to support groups or mental health professionals if needed. Helping patients identify and implement effective coping mechanisms empowers them to manage the emotional impact of PsA.
Referrals to Mental Health Professionals
If a patient with PsA is struggling with significant emotional distress, depression, or anxiety, it may be necessary to refer them to mental health professionals for further assessment and intervention. Mental health professionals, such as psychologists or psychiatrists, can provide specialized support and evidence-based interventions to address the patient’s emotional well-being. Collaborate with these professionals to ensure a comprehensive approach to the patient’s care. Referrals to mental health professionals promote optimal psychosocial support and facilitate improved mental health outcomes.
Patient Education
Explaining Psoriatic Arthritis
Patient education is a cornerstone of nursing care for PsA. Provide a clear and concise explanation of PsA, including its causes, symptoms, and potential complications. Use visual aids or educational materials to enhance understanding. Discuss the chronic nature of the condition and emphasize the importance of long-term management. Answer any questions the patient may have and address any misconceptions. Explaining PsA helps patients gain a better understanding of their condition, promoting active engagement in self-management.
Educating on Self-Care Strategies
Educate patients on self-care strategies that can help manage PsA symptoms and improve quality of life. Teach joint protection techniques, such as proper body mechanics and ergonomic modifications, to reduce joint stress. Instruct patients on the use of heat and cold therapy for pain relief. Provide guidance on activities of daily living, such as how to dress or perform household tasks with minimal joint strain. Educating on self-care strategies empowers patients to take an active role in managing their condition.
Promoting Medication Adherence
Educate patients about the importance of medication adherence in managing PsA effectively. Explain the purpose of prescribed medications, their potential benefits, and possible side effects. Instruct patients on proper medication administration techniques and the importance of following the prescribed dosage schedule. Provide written materials or medication diaries to assist with medication tracking. Promoting medication adherence supports optimal treatment outcomes and minimizes disease progression.
Providing Resources for Additional Information
Offer patients and their families resources for additional information and support regarding PsA. Provide reliable websites, published materials, or patient support groups where they can access accurate and up-to-date information. Refer patients to local or online support groups where they can connect with others facing similar challenges. Encourage them to access community resources for emotional support or financial assistance if needed. Providing patients with resources for additional information enhances their knowledge and enables them to make informed decisions about their care.
Promotion of Physical Activity
Assessing Physical Activity Levels
Assessing the patient’s current physical activity levels is a vital step in promoting physical activity in patients with PsA. Use validated tools, such as the Physical Activity Rating (PAR) or activity trackers, to measure the patient’s daily physical activity levels. Discuss their daily routines and identify barriers or challenges to physical activity. Assessing physical activity levels provides a baseline for developing an individualized exercise plan.
Developing Individualized Exercise Plans
Collaborate with a physical therapist to develop an individualized exercise plan tailored to the patient’s needs and abilities. Consider the patient’s joint limitations, comorbidities, and personal preferences. Include a mix of cardiovascular exercises, such as walking or swimming, and joint-friendly exercises, such as yoga or tai chi. Gradually progress the exercise plan, considering the patient’s tolerance and progress. Developing individualized exercise plans promotes physical well-being and joint health in patients with PsA.
Monitoring Exercise Tolerance and Progress
Regularly monitor the patient’s exercise tolerance and progress to ensure that the exercise plan remains safe and effective. Assess the patient’s level of fatigue, joint pain, and any adverse effects during and after exercise. Encourage the patient to keep an exercise diary to track progress and identify areas for improvement. Adjust the exercise plan accordingly based on the patient’s feedback and observed tolerance. Monitoring exercise tolerance and progress helps optimize the benefits of physical activity and minimizes the risk of exacerbating joint symptoms.
Collaborating with Physical Therapists
Collaboration with physical therapists plays a crucial role in the promotion of physical activity for patients with PsA. Physical therapists can offer specialized exercise programs, manual therapy techniques, and assistive devices to enhance mobility and joint function. Regularly communicate with the physical therapist to ensure alignment in goals and strategies. Collaborating with physical therapists optimizes the patient’s functional abilities and promotes long-term joint health.
Systemic and Local Treatment Options
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed to manage pain and inflammation in PsA. These medications work by reducing prostaglandin production, thereby alleviating pain and swelling. Examples of NSAIDs include ibuprofen, naproxen, and celecoxib. It is essential to educate patients about the potential side effects of NSAIDs, such as gastrointestinal irritation or increased risk of cardiovascular events. Monitor patients closely for any adverse effects and adjust treatment as needed.
Disease-Modifying Antirheumatic Drugs (DMARDs)
Disease-modifying antirheumatic drugs (DMARDs) are a cornerstone of PsA treatment. These medications target the underlying immune dysfunction, slowing down disease progression and preserving joint function. Methotrexate, sulfasalazine, and leflunomide are common DMARDs used in PsA. Educate patients about the need for regular monitoring, such as blood tests or liver function tests, while on DMARD therapy. Monitor patients closely for both efficacy and potential side effects, adjusting treatment as needed.
Biologic Response Modifiers
Biologic response modifiers, also known as biologics, are a class of medications that specifically target certain molecules involved in inflammation. These medications are administered by injection or infusion and provide effective relief for many patients with PsA. Tumor necrosis factor (TNF) inhibitors, such as adalimumab or etanercept, are commonly used biologics in PsA. Educate patients about the importance of regular monitoring, potential side effects, and signs of infection. Monitor patients closely for treatment response and adverse events, collaborating with the healthcare team to ensure optimal treatment outcomes.
Topical Medications
Topical medications, such as corticosteroids or topical retinoids, are often used to manage localized skin symptoms in PsA. These medications can reduce inflammation, itching, and redness in psoriatic plaques. Instruct patients on how to properly apply topical medications and discuss potential side effects, such as skin thinning or irritation. Collaborate with dermatologists to determine the appropriate use and duration of topical treatment.
Corticosteroids
Corticosteroids are potent anti-inflammatory medications that can provide significant symptom relief for patients with PsA. These medications may be administered orally, topically, or through injections. Instruct patients on the potential side effects of corticosteroids, such as weight gain, increased blood sugar levels, or increased susceptibility to infections. Corticosteroids should be used judiciously, typically in short-term or acute situations, to minimize the risk of long-term complications.
Overall, a comprehensive nursing management approach for patients with psoriatic arthritis involves thorough assessment, collaborative care planning, implementation of appropriate interventions, and ongoing evaluation of the patient’s response to treatment. By addressing the physical, emotional, and educational needs of patients with PsA, nurses play a vital role in promoting optimal health outcomes and improving the overall quality of life for individuals living with this chronic condition.