So you’re considering a cornea transplant? It’s important to be aware of the potential risks and take necessary precautions before undergoing the procedure. This article will provide you with valuable information on the risk factors associated with cornea transplants and the precautions you can take to ensure a successful outcome. Whether you’re a prospective recipient or simply curious about the process, understanding these key factors will help you make informed decisions about your eye health.
Potential Risk Factors for Cornea Transplant
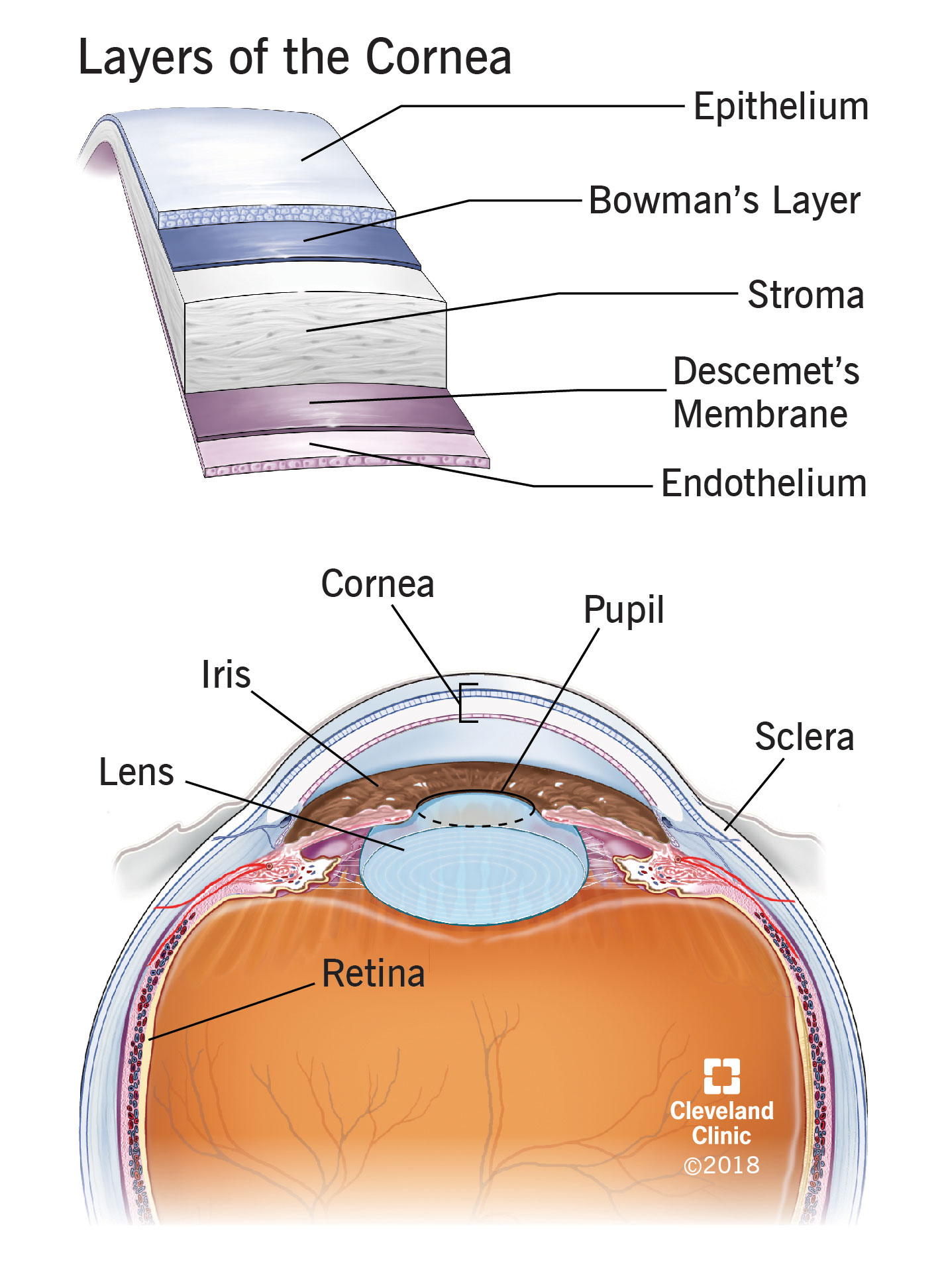
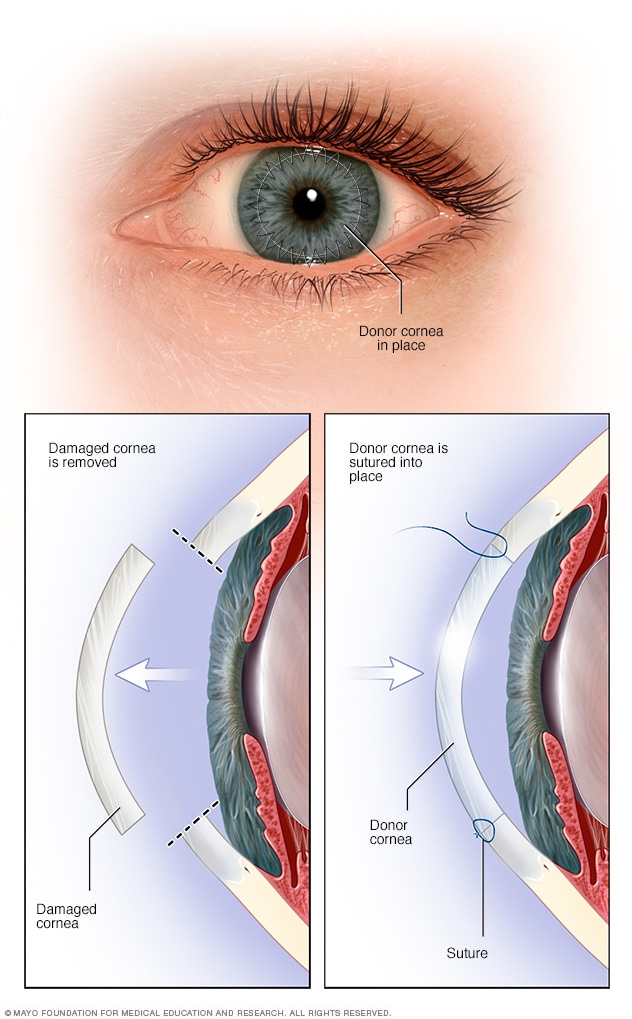
Cornea transplantation, or corneal grafting, is a surgical procedure that involves replacing a damaged or diseased cornea with a healthy donor cornea. While this procedure has shown remarkable success in restoring vision and improving quality of life for many patients, it is important to be aware of the potential risk factors associated with cornea transplant. Understanding these risk factors can help both patients and healthcare providers make informed decisions and take necessary precautions to ensure a successful outcome.
Age
Age plays a crucial role in the success of cornea transplant surgery. Both young and elderly patients have unique considerations that need to be taken into account.
Effect of Age on Transplant Success
Studies have shown that younger patients generally have better graft survival rates compared to older individuals. This may be attributed to the overall health of younger patients and a more resilient immune system. However, advanced age alone should not disqualify a patient from receiving a cornea transplant. Other factors such as overall health and potential complications should also be considered.
Minimum Age Requirements
There is no specific minimum age requirement for cornea transplant surgery. However, it is important for pediatric patients to undergo a thorough evaluation by an ophthalmologist to determine if they are suitable candidates for the procedure.
Maximum Age Limitations
While there is no strict maximum age limit for cornea transplant, advanced age can increase the risk of complications and affect long-term graft survival. Older patients should be carefully evaluated to determine if they are suitable candidates for the surgery.
Impact of Age on Recovery
Recovery from cornea transplant surgery may be slower in older patients due to a natural decline in the body’s healing abilities. Close post-operative monitoring and adherence to the doctor’s instructions can help mitigate any potential complications and ensure a smooth recovery.
Underlying Medical Conditions
Underlying medical conditions can significantly impact the outcome of a cornea transplant. It is important to evaluate these conditions and manage them appropriately prior to undergoing surgery.
Effect of Diabetes on Transplant Outcome
Diabetes is a chronic condition that affects the body’s ability to regulate blood sugar levels. Uncontrolled diabetes can hinder the healing process and increase the risk of infection and graft rejection. Patients with diabetes should strive for optimal blood sugar control before undergoing cornea transplant surgery.
Autoimmune Diseases and Transplant Complications
Autoimmune diseases such as rheumatoid arthritis and systemic lupus erythematosus can affect the body’s immune response and increase the risk of graft rejection. Patients with autoimmune diseases should work closely with their healthcare team to manage their conditions effectively both before and after cornea transplant surgery.
Hypertension and Transplant Surgery
High blood pressure, or hypertension, can impact the success of cornea transplant by affecting the blood flow to the transplant site. Adequate blood pressure control is essential for minimizing potential complications and optimizing the chances of a successful outcome.
Infectious Diseases and Transplant Suitability
Certain infectious diseases, such as hepatitis, HIV, and active tuberculosis, can prevent a patient from being eligible for cornea transplantation. The presence of active infections can increase the risk of complications during surgery and compromise the success of the transplant. It is important for patients to undergo thorough screenings for infectious diseases before being considered for cornea transplant surgery.
Previous Eye Surgeries
Prior eye surgeries can pose additional risks and considerations when undergoing a cornea transplant. The impact of these surgeries should be evaluated carefully to ensure a successful outcome.
Effect of Prior Surgeries on Transplant Success
Previous eye surgeries, such as cataract removal or retinal surgery, can affect the success of a cornea transplant by altering the anatomy of the eye and potentially complicating the surgical procedure. The surgeon should be aware of any prior eye surgeries and evaluate their impact on the cornea transplant.
Correlation with Higher Complication Rates
Studies have shown that patients with a history of previous eye surgeries may be at a higher risk of developing complications during and after cornea transplant surgery. It is crucial for the surgeon to assess the patient’s medical history and determine the best course of action to minimize potential risks.
Specific Surgical Procedures and Risks
Certain eye surgeries, such as radial keratotomy or LASIK, can weaken the structural integrity of the cornea and make it more susceptible to complications during cornea transplant surgery. The surgeon should carefully evaluate the impact of these procedures and make informed decisions regarding the transplant procedure.
Corneal Scarring or Infection
Corneal scarring or infection can significantly impact the success of a cornea transplant. Evaluating the severity of scarring or infection and implementing appropriate precautions are crucial for a positive outcome.
Impact of Existing Scarring on Transplant
Existing corneal scarring can make the surgical procedure more challenging and increase the risk of complications during cornea transplant surgery. The surgeon should evaluate the extent of the scarring and determine the best approach for the transplant.
Risk of Infection and Rejection
A history of corneal infection can increase the risk of infection and graft rejection after cornea transplant surgery. Precautionary measures, such as appropriate antibiotic prophylaxis and close post-operative monitoring, should be implemented to minimize these risks.
Precautions and Management Strategies
In cases where there is corneal scarring or a previous history of infection, additional measures may be necessary to ensure a successful cornea transplant. The surgeon may utilize specialized surgical techniques or medications to enhance the chances of a positive outcome.
Corneal Thinning
Corneal thinning conditions, such as keratoconus, can affect the suitability and success of a cornea transplant. Special considerations should be taken when evaluating patients with corneal thinning.
Understanding Thinning Conditions
Corneal thinning conditions, such as keratoconus or pellucid marginal degeneration, can make the cornea structurally weak and impact overall vision. The surgeon should assess the severity of the thinning and determine if a cornea transplant is the appropriate course of action.
Eligibility for Transplant with Thin Cornea
In cases of corneal thinning, the surgeon may need to carefully select an appropriate donor cornea that matches the thinning pattern or consider alternative surgical techniques, such as partial-thickness corneal transplantation. These decisions will be made based on the specific needs and circumstances of the patient.
Special Considerations during Surgery
During cornea transplant surgery for thin corneas, the surgeon must exercise caution to avoid further weakening of the cornea. Precise surgical techniques and meticulous intraoperative care are essential to minimize potential complications and optimize the chances of a successful transplant.
Eye Conditions like Glaucoma
Existing eye conditions, such as glaucoma, can pose additional risks and considerations for cornea transplant surgery. Evaluating the impact of glaucoma and implementing appropriate management strategies is crucial for a positive outcome.
Glaucoma as a Risk Factor
Glaucoma is a condition characterized by increased intraocular pressure, which can damage the optic nerve and lead to vision loss. Patients with glaucoma may be at a higher risk of complications during and after cornea transplant surgery due to the potential for increased intraocular pressure.
Transplant Suitability with Glaucoma
Patients with glaucoma can still be considered for cornea transplant, but it is essential for the surgeon to monitor and manage the intraocular pressure both during and after the procedure. Close collaboration with the patient’s ophthalmologist or glaucoma specialist is vital for optimal post-operative care.
Post-Transplant Glaucoma Management
After cornea transplant surgery, patients with glaucoma will require ongoing monitoring of intraocular pressure and implementation of appropriate glaucoma management strategies. This may include the use of medications, laser treatments, or even additional surgical interventions to control the intraocular pressure and preserve the health of the transplanted cornea.

Immunosuppressant Medications
Immunosuppressant medications are often necessary to prevent the body from rejecting the transplanted cornea. However, they can also pose certain risks and require careful monitoring.
Role of Immunosuppressants in Transplants
Immunosuppressant medications are prescribed to cornea transplant recipients to suppress the immune system’s response and prevent rejection of the transplanted cornea. These medications are essential for ensuring the long-term success of the graft.
Potential Side Effects and Complications
Immunosuppressant medications can have potential side effects and complications, including increased susceptibility to infections, impaired wound healing, and metabolic imbalances. The healthcare team will closely monitor the patient’s medication regimen and adjust the dosage as needed to minimize these risks.
Monitoring and Adjustment of Medication Dosage
Regular monitoring of the patient’s immune system markers, drug levels, and overall health is crucial when using immunosuppressant medications. The medication dosage may need to be adjusted over time to achieve a balance between preventing rejection and managing potential side effects.
Smoking and Alcohol Consumption
Smoking and excessive alcohol consumption can have detrimental effects on cornea transplant outcomes. Patients should be aware of the risks associated with these behaviors and make necessary lifestyle changes.
Negative Impact on Transplant Outcomes
Smoking and alcohol consumption can negatively impact the success of cornea transplant surgery. Smoking, in particular, can impair wound healing and increase the risk of infection and graft rejection. Excessive alcohol consumption can also interfere with the body’s healing processes.
Increased Risk of Complications
Patients who smoke or consume alcohol excessively may experience higher rates of complications following cornea transplant surgery. These complications can include increased inflammation, impaired graft survival, and delayed recovery.
Recommendations for Smoking and Alcohol Cessation
To optimize the chances of a successful cornea transplant, patients are strongly encouraged to quit smoking and significantly reduce alcohol consumption before and after the procedure. Support from healthcare providers, smoking cessation programs, and counseling services can assist patients in making these necessary lifestyle changes.
Conclusion
Understanding the potential risk factors associated with cornea transplant surgery is crucial for both patients and healthcare providers. Factors such as age, underlying medical conditions, previous eye surgeries, corneal scarring or infection, corneal thinning, eye conditions like glaucoma, immunosuppressant medications, smoking, and alcohol consumption can all impact the success of the procedure. By carefully evaluating these risk factors, implementing appropriate precautions, and providing comprehensive post-operative care, healthcare providers can optimize the chances of a successful cornea transplant and improve the quality of life for their patients.