You’ve just been diagnosed with a serious lung condition, and your doctor has advised you to consider a lung transplant as a possible treatment option. But before you dive into this life-changing decision, it’s crucial to understand the risk factors involved and the precautions you must take for a successful outcome. In this article, we will explore the various risk factors that may affect the success of a lung transplant and the precautions you need to be aware of to ensure a smooth and effective transplantation process. So, let’s get started on this important journey towards a healthier future.
Risk Factors for Lung Transplant
Lung transplantation is a complex and life-saving procedure that offers hope to individuals suffering from end-stage lung diseases. While the procedure itself has greatly advanced over the years, it is crucial to consider various risk factors that can affect the success of a lung transplant. These risk factors encompass a range of factors, including age, underlying lung disease, general health status, smoking history, infections, prior transplants, rejection history, mental health, financial considerations, and donor availability. Understanding these risk factors is essential for both patients and healthcare professionals involved in the lung transplant process to ensure the best possible outcome for the recipient.
Age
Age plays a significant role in lung transplantation. Younger patients generally have better outcomes due to their stronger physiological resilience and ability to tolerate the procedure. However, age alone should not exclude anyone from being considered for a lung transplant. Older patients can still undergo successful transplantations if they are in good health overall and do not have any significant comorbidities that could negatively impact the transplantation process or recovery.
Underlying Lung Disease
The underlying lung disease is a crucial factor that determines the need for a lung transplant. Several chronic lung diseases may necessitate transplantation, including chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), cystic fibrosis, alpha-1 antitrypsin deficiency, bronchiectasis, and pulmonary hypertension. Each of these diseases presents different challenges and considerations for the transplant team and the patient. The severity and progression of the underlying lung disease are essential to evaluate when assessing the appropriateness of a lung transplant.
General Health Status
The general health status of a patient is a critical factor in determining their suitability for a lung transplant. Various aspects of overall health must be evaluated, including an assessment of the patient’s body mass index (BMI), cardiovascular function, renal function, liver function, and presence of any immunocompromised conditions. A comprehensive evaluation of the patient’s overall health helps the transplant team understand the patient’s ability to endure the transplantation process and recover successfully.
Smoking History
Smoking has long been associated with a range of respiratory diseases, including those that may necessitate lung transplantation. Consequently, a patient’s smoking history plays a significant role in transplant eligibility and post-transplant outcomes. Current smokers are generally advised to quit smoking before undergoing a transplant to reduce the risk of complications and to improve overall health. Former smokers should also be mindful of the potential residual damage caused by smoking. Additionally, exposure to secondhand smoke can also have detrimental effects on lung health and needs to be taken into consideration.

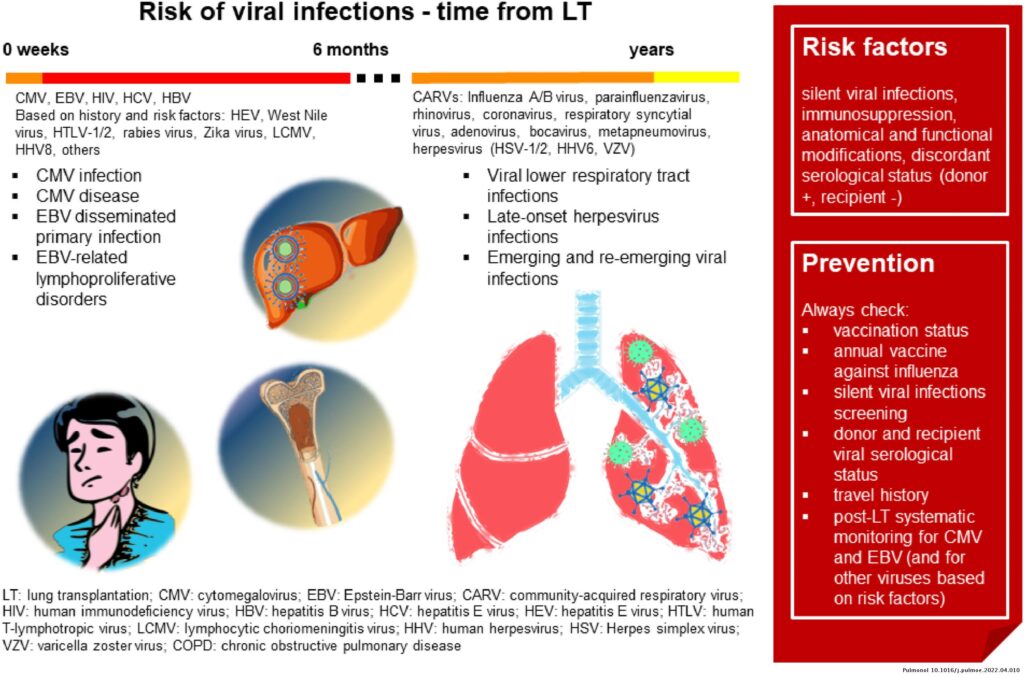
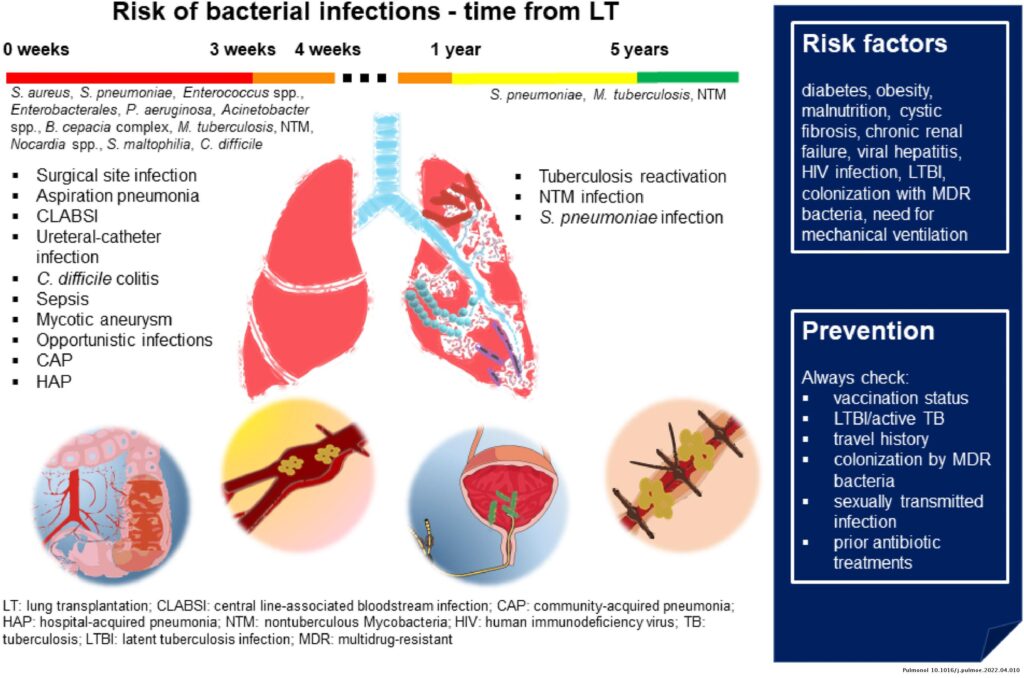
Infections
Infections are a concern both before and after a lung transplant. Active infections can significantly impact the success of a transplantation as they increase the risk of complications and can impede the healing process. Chronic infections, such as tuberculosis or fungal infections, need to be thoroughly evaluated and treated before a lung transplant can take place. Infectious disease screening is an essential part of the evaluation process to identify and address any existing infections that may affect the transplant candidacy.
Prior Transplants
Patients who have undergone previous lung transplants or other solid organ transplants present unique considerations for subsequent lung transplantation. Previous lung transplants introduce additional complexities into the transplantation process, as the patient may have adhesions or scar tissue that can complicate the procedure. Individuals with prior solid organ transplants may have additional comorbidities or complications that need to be carefully managed throughout the transplantation process.

Rejection History
A history of previous rejections presents a significant risk factor for future lung transplants. Patients with a history of rejection need to be closely monitored and may require more intensive immunosuppressive therapy to prevent rejection in subsequent transplants. Treatment for previous rejections can vary depending on the underlying cause and severity. Additionally, patients who have developed antibodies against previous transplants may be more prone to future rejections and require careful evaluation and management.
Mental Health
Mental health plays a crucial role in the success of a lung transplantation. Patients must undergo an evaluation and treatment for any underlying mental health conditions before proceeding with transplantation. Depression, anxiety, and other psychological factors can impact a patient’s ability to adhere to post-transplant medication regimens, attend follow-up appointments, and manage stress during the recovery process. Psychosocial support is essential to ensure the patient’s overall well-being and helps prevent potential complications that may arise from untreated mental health conditions. Additionally, a patient’s substance abuse history must also be evaluated and addressed as part of the transplant process.
Financial Considerations
Lung transplantation is a complex and costly procedure, and financial considerations play a crucial role in the transplantation process. Patients and their families must be aware of the financial implications associated with transplantation, including pre-transplant evaluations, surgical costs, post-transplant care, medication expenses, rehabilitation, and follow-up visits. It is vital to have a comprehensive understanding of the available healthcare coverage, insurance options, and potential financial assistance programs to alleviate the burden on the patient and their family.
Donor Availability
The availability of suitable donor lungs greatly influences the success of a lung transplant. The scarcity of donor organs poses a significant challenge to the transplantation process. Factors such as blood type compatibility, size matching, and geographical proximity play essential roles in activating the transplant waiting list and facilitating the timely transplantation of a compatible organ. It is important for patients to understand the logistics of waiting for a suitable donor and to maintain good health while awaiting transplantation.
In conclusion, lung transplantation is a complex procedure that carries inherent risks. Understanding the various risk factors involved is crucial for both patients and healthcare professionals. Age, underlying lung disease, general health status, smoking history, infections, prior transplants, rejection history, mental health, financial considerations, and donor availability all contribute to the overall success of a lung transplant. By carefully assessing these risk factors, healthcare professionals can provide comprehensive care and support to patients, ensuring the best possible outcomes for those in need of a life-saving lung transplant.