The Connection Between Diabetes and Skin Health
When you think of diabetes, the first things that might come to mind are blood sugar levels, insulin resistance, and perhaps changes in diet. But did you know that diabetes can also have a significant impact on your skin health? In this article, we’ll delve into the intricate connection between diabetes and your skin, exploring how this condition affects not only your internal health but your external well-being as well. If you or someone you know is managing diabetes, this information is vital for taking care of your skin in addition to your metabolic health.
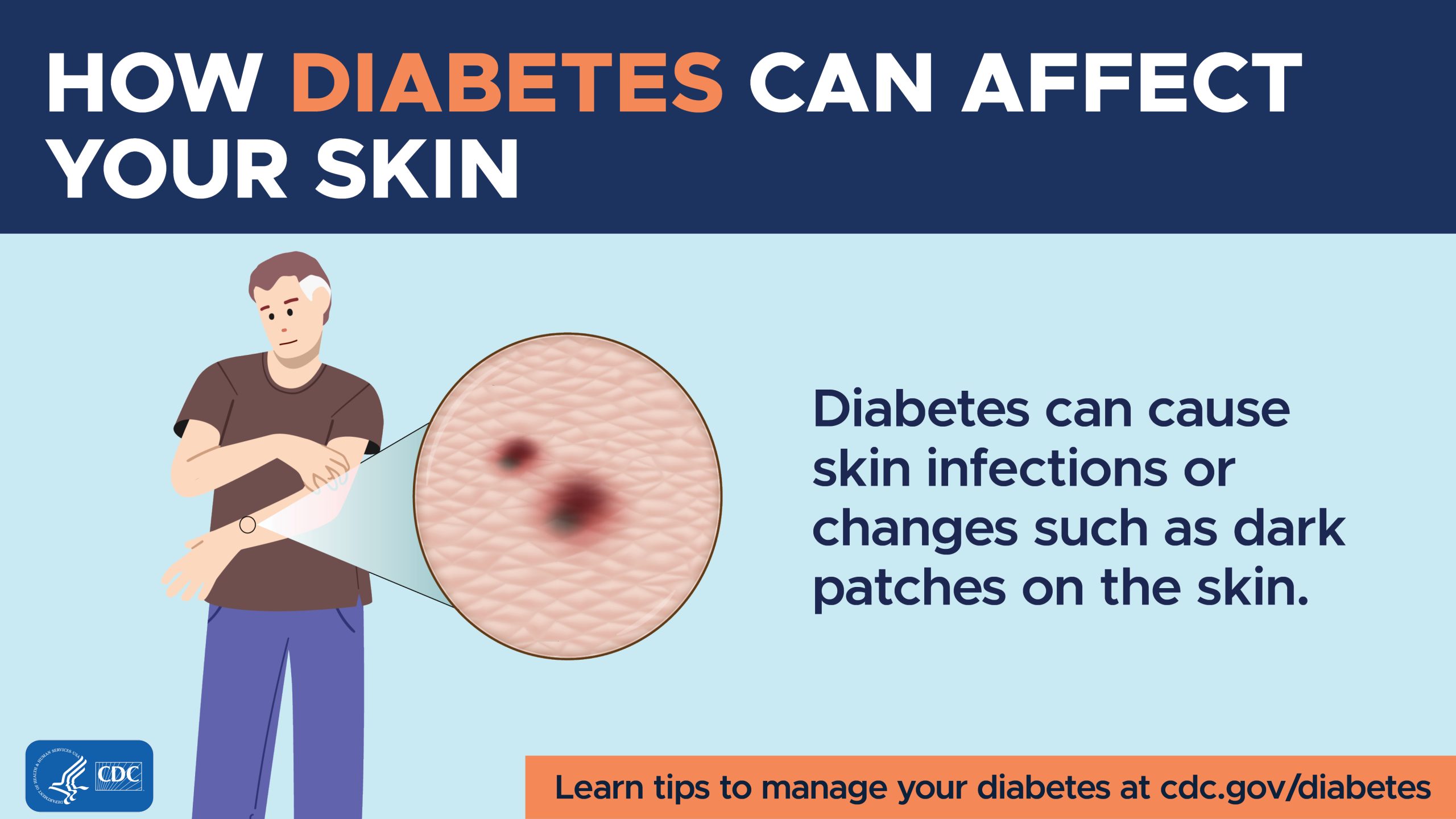
How Diabetes Affects Your Skin
Diabetes is a multifaceted condition that influences various aspects of your health, including your skin. High blood sugar levels can lead to a series of skin issues, largely due to the changes that occur in your body as a result of this condition. When your blood sugar remains elevated for extended periods, it can result in thickening of the skin and compromised circulation. This can leave your skin looking dull or even contributing to various skin disorders. Understanding this connection is the first step toward ensuring that you maintain healthy skin despite the challenges diabetes poses.
Additionally, the inability for the body to properly heal can be magnified in individuals with diabetes. When you have cuts or scratches, your skin’s natural healing mechanisms may be less efficient. This can lead to prolonged recovery times and an increased risk of infections, which not only result in discomfort but can also lead to serious complications.
Common Skin Conditions Linked to Diabetes
Living with diabetes can expose you to a range of skin conditions that may be uncomfortable or distressing. Here are some common skin issues that those with diabetes may face:
Diabetic Dermopathy
Diabetic dermopathy features light brown, scaly patches that occur mostly on the shins. Often harmless, these skin changes are associated with long-term diabetes and result from the damage that elevated blood sugar levels can inflict on small blood vessels. While there’s no cure, maintaining good blood sugar levels can help manage and prevent further development.
Atopic Dermatitis
If you experience dry, itchy skin, it could be more than just a nuisance; it might also be related to your diabetes. Individuals with diabetes are at higher risk for atopic dermatitis, a condition characterized by inflamed, itchy skin. Managing your blood sugar effectively can greatly alleviate these symptoms, providing you with much-needed comfort.
Fungal Infections
The warm, moist environments often present in the folds of your skin can create the perfect breeding ground for fungal infections, such as athlete’s foot or yeast infections. If you have diabetes, you may be more susceptible to these infections, making it crucial to practice diligent hygiene.
Bacterial Infections
High blood sugar levels can weaken your immune system, leaving your skin open to bacterial infections. Conditions like boils or styes may become more common, serving as a reminder that skin health is intricately linked to your blood sugar control.

The Role of Blood Sugar Management
You might wonder how maintaining stable blood sugar levels directly correlates with healthier skin. The answer lies in how fluctuations in your glucose levels affect not just your internal systems but also the outward appearance and resilience of your skin. When blood sugar is well-managed, your skin has a better chance to repair itself, preventing issues like dryness and infections.
There are multiple strategies for managing blood sugar, including adhering to a balanced diet, exercising regularly, monitoring your glucose levels consistently, and even managing stress. While you’re focused on maintaining your overall health, don’t forget to pay attention to your skin. A happy body often reflects a healthy outer layer.
Importance of Skincare Routines for Diabetics
In addition to managing blood sugar, establishing a skincare routine can significantly benefit those living with diabetes. You might want to consider incorporating moisturizers, gentle cleansers, and products rich in antioxidants into your daily regimen. Here’s why a consistent skincare routine can make a world of difference:
Moisturizing Your Skin
For individuals with diabetes, skin can become dry and irritated due to various factors, including dehydration and low circulation. Opt for a high-quality moisturizer that includes ingredients like glycerin or hyaluronic acid. Not only do these ingredients hydrate your skin, but they also create a protective barrier against external irritants.
Gentle Cleansing
It’s essential to cleanse your skin gently. Look for mild, non-irritating cleansers that don’t strip your skin of moisture. Using harsh soaps may worsen skin issues, making it vital to treat your skin delicately.
Sun Protection
Sun exposure can exacerbate existing skin conditions and lead to faster skin aging. Make it a habit to use a broad-spectrum sunscreen with at least SPF 30 every day, regardless of the weather. This will not only protect your skin from harmful UV rays but also help maintain a more even complexion.

Healing Wounds with Diabetes
Wound healing can be a significant concern for individuals with diabetes. Minor cuts or scrapes may take longer to heal, increasing the risk of infections. Understanding how to care for wounds is essential to maintaining overall skin health.
The Healing Process
When a cut occurs, your body goes through a healing process that requires nutrients, oxygen, and adequate blood flow. Unfortunately, diabetes can impair this process, making it crucial to take steps to promote healing. Keeping your wounds clean and covered while also monitoring them for any signs of infection can reduce complications.
Seek Professional Help
If you notice a wound that doesn’t seem to be healing or is showing signs of infection, don’t hesitate to reach out to a healthcare professional. Timely intervention can prevent more severe complications and help maintain your quality of life.
Lifestyle Changes for Healthy Skin
You have the power to make lifestyle changes that can enhance both your diabetes management and skin health. Here are a few strategies that can lead to improvements:
Balanced Diet
A well-balanced diet can Help you manage blood sugar levels, and it plays a vital role in supporting your skin’s health. Incorporate plenty of fruits, vegetables, whole grains, and lean proteins while limiting processed foods and sugars. Eating nutrient-dense foods will provide your skin with the vitamins it needs to remain resilient.
Hydration Matters
It’s easy to overlook, but drinking adequate water is crucial for maintaining skin elasticity and moisture levels. Aim for at least eight glasses of water each day, and you may be surprised by how much it benefits your skin health.
Regular Exercise
Engaging in physical activity isn’t just essential for managing blood sugar; it also promotes healthy skin. Exercise increases blood circulation, which allows nutrients to reach your skin more effectively. Whether it’s going for a walk, taking a yoga class, or hitting the gym, find an activity you love and make it part of your routine.

Psychological Well-Being and Skin Health
Living with diabetes can take an emotional toll on many individuals, and stress can have a direct negative impact on your skin. Stressful situations can worsen skin conditions, leading to flare-ups or increased sensitivity. Therefore, managing your mental health is just as important as your physical health.
Mindfulness and Relaxation Techniques
Finding ways to cope with stress is essential. Consider incorporating mindfulness techniques like meditation or deep breathing exercises into your daily routine. Taking time for yourself can help you feel grounded and improve your overall outlook on life.
Stay Connected
Don’t underestimate the importance of social support. Whether it’s through friends, family, or diabetes support groups, talking about your challenges can lighten your emotional load. You’ll likely find it comforting to know you’re not alone in your experiences.
The Role of Healthcare Providers
Finally, you play an important role in managing your skin health alongside your diabetes. Regular check-ins with healthcare providers like dermatologists and endocrinologists can offer tailored advice and treatment options. This will ensure you receive the necessary guidance to prevent skin issues and maintain healthy skin over the long term.
Skin Specialists
If you’re noticing persistent skin issues related to your diabetes, consulting a dermatologist specializing in diabetic skin conditions can be incredibly helpful. They can provide personalized treatment plans and recommend products suited to your individual needs.
Team Approach
Don’t hesitate to advocate for yourself and discuss your skin concerns during doctor visits. Your skin health is an integral part of your overall health, and having a team that understands how diabetes affects your skin can make a significant difference.

In Conclusion
The connection between diabetes and skin health is profound, impacting various aspects of your well-being. From common skin conditions to the importance of blood sugar management, understanding this relationship is crucial for taking proactive steps. You have the power to work towards healthy skin by making appropriate lifestyle changes, maintaining a diligent skincare routine, and engaging with your healthcare team.
As you continue your journey with diabetes, remember that your skin reflects the care you give to your entire body. With the right knowledge and practices, you can maintain both your health and your skin in harmony.
If you found this article helpful, please consider clapping for it, leaving a comment, and subscribing to my Medium newsletter for regular updates. Your engagement motivates me and helps create a supportive community around important health topics!