Diabetes, a prevalent condition affecting millions of individuals worldwide, has been closely associated with various health complications. Among these, a worrying connection has been identified between diabetes and acute renal failure. Acute renal failure, also known as acute kidney injury, is a sudden and rapid decline in kidney function. In this article, we will explore the link between diabetes and acute renal failure, delving into the potential causes, risk factors, and preventive measures that can be taken to mitigate the impact of this concerning association.
Overview of Acute Renal Failure
Acute Renal Failure, also known as acute kidney injury, is a sudden and rapid loss of kidney function. It occurs when the kidneys are unable to filter waste products and excess fluids from the blood. This condition requires immediate medical attention, as it can lead to serious complications if left untreated.
Definition
Acute Renal Failure is defined as a sudden slowdown or cessation of kidney function within a short period, typically within a few hours to a few days. It is characterized by a rapid increase in creatinine levels and a decrease in urine output. This condition can be caused by various factors, such as dehydration, blood loss, obstruction of the urinary tract, or underlying medical conditions.
Causes
There are several causes of Acute Renal Failure. These include:
- Dehydration: Insufficient fluid intake or excessive fluid loss can lead to decreased blood flow to the kidneys, resulting in kidney injury.
- Blood Loss: Severe bleeding, either internally or externally, can cause a drop in blood pressure, reducing blood flow to the kidneys and affecting their function.
- Urinary Tract Obstruction: Blockages in the urinary system, such as kidney stones or an enlarged prostate, can prevent the normal flow of urine and lead to kidney damage.
- Infections: Bacterial or viral infections, such as urinary tract infections or kidney infections, can cause inflammation and damage to the kidneys.
- Medications and Toxins: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or antibiotics, as well as exposure to toxins, can harm the kidneys and cause Acute Renal Failure.
Risk factors
While Acute Renal Failure can affect anyone, there are certain factors that may increase the risk of developing this condition. These risk factors include:
- Advanced age: Older adults are more prone to Acute Renal Failure due to age-related changes in kidney function.
- Chronic medical conditions: Individuals with pre-existing conditions like diabetes, high blood pressure, or heart disease have a higher risk of developing Acute Renal Failure.
- Kidney disease: People with chronic kidney disease are more susceptible to Acute Renal Failure because their kidneys are already compromised.
- Certain medications: Certain medications, especially when taken in high doses or over a long period, can increase the risk of kidney damage and Acute Renal Failure.
Symptoms
The symptoms of Acute Renal Failure can vary depending on the severity and underlying cause. Common symptoms include:
- Decreased urine output or complete cessation of urine production
- Swelling in the legs, ankles, or face
- Fatigue and weakness
- Shortness of breath
- Nausea and vomiting
- Confusion or difficulty concentrating
Diagnosis
Diagnosing Acute Renal Failure involves a combination of medical history, physical examination, and laboratory tests. The healthcare provider may ask about symptoms, medical conditions, and any recent medications or interventions. Physical examination may reveal signs of fluid retention, high blood pressure, or other relevant findings.
Laboratory tests play a crucial role in the diagnosis of Acute Renal Failure. Blood tests can measure levels of creatinine, a waste product normally cleared by the kidneys, and determine the glomerular filtration rate (GFR), which reflects kidney function. Urine tests can detect the presence of protein, blood, or other abnormalities that may indicate kidney damage.
In some cases, additional imaging studies or a kidney biopsy may be necessary to determine the underlying cause of Acute Renal Failure and guide treatment decisions.
Treatment options
The treatment of Acute Renal Failure aims to address the underlying cause, provide supportive care, and prevent complications. Treatment options may include:
- Fluid replacement: Intravenous fluids are administered to restore fluid balance and maintain adequate blood pressure.
- Medications: Medications may be prescribed to manage symptoms, control blood pressure, or treat underlying infections.
- Dialysis: In severe cases, dialysis may be required to remove waste products and excess fluids from the body when the kidneys are unable to do so.
- Treatment of the underlying cause: If Acute Renal Failure is caused by a specific condition, such as dehydration or urinary tract obstruction, treating the underlying cause is essential for recovery.
Complications
Acute Renal Failure can lead to various complications if not promptly treated. These complications may include:
- Chronic kidney disease: Prolonged or severe cases of Acute Renal Failure may cause irreversible damage to the kidneys, resulting in chronic kidney disease.
- Fluid overload: The inability to remove excess fluids from the body can lead to fluid overload, causing swelling and putting strain on the heart and lungs.
- Electrolyte imbalances: Acute Renal Failure can disrupt the balance of electrolytes in the body, leading to abnormal levels of sodium, potassium, calcium, and other essential minerals.
- Infections: Weakened immune function and compromised kidney function increase the risk of infections, such as urinary tract infections or bloodstream infections.
It is essential to seek medical attention if you experience symptoms of Acute Renal Failure to prevent these complications and protect your overall health.
Understanding Diabetes
Definition
Diabetes is a chronic condition characterized by high levels of blood glucose (sugar) due to the body’s inability to produce or effectively utilize insulin. Insulin is a hormone that regulates glucose metabolism, allowing cells to use glucose for energy. Without proper insulin function, glucose accumulates in the bloodstream, leading to various complications.
Types of Diabetes
There are three main types of diabetes:
- Type 1 diabetes: This type of diabetes occurs when the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. People with type 1 diabetes require insulin injections or an insulin pump to manage their blood glucose levels.
- Type 2 diabetes: Type 2 diabetes is the most common form and typically develops as a result of insulin resistance, where the body’s cells become resistant to the effects of insulin. Lifestyle factors, such as obesity and physical inactivity, play a significant role in the development of type 2 diabetes. It can often be managed with a combination of healthy eating, regular physical activity, and medication if necessary.
- Gestational diabetes: Gestational diabetes occurs during pregnancy when hormonal changes make cells more resistant to insulin. While it usually resolves after childbirth, it increases the risk of developing type 2 diabetes later in life.
Causes
The exact causes of diabetes vary depending on the type of diabetes. In type 1 diabetes, it is believed to be an autoimmune reaction that causes the destruction of insulin-producing cells in the pancreas. The triggers for this autoimmune response are still not fully understood.
Type 2 diabetes is primarily caused by a combination of genetic factors and lifestyle choices. Factors such as obesity, sedentary lifestyle, unhealthy eating habits, and insulin resistance contribute to the development of type 2 diabetes.
Gestational diabetes occurs due to the hormonal changes during pregnancy that affect insulin function. The placenta produces hormones that can impair the body’s ability to use insulin effectively.
Symptoms
The symptoms of diabetes can vary depending on the type and severity of the condition. Some common symptoms include:
- Frequent urination
- Increased thirst and hunger
- Weight loss (in type 1 diabetes)
- Fatigue and weakness
- Blurred vision
- Slow wound healing
- Recurrent infections, such as urinary tract infections or yeast infections
While these symptoms may be present in all types of diabetes, type 1 diabetes often presents with more severe and sudden symptoms, while type 2 diabetes may have a more gradual onset and milder symptoms.
Diagnosis
Diagnosing diabetes involves a combination of blood tests and assessment of symptoms. The most common test for diagnosing diabetes is the fasting plasma glucose (FPG) test. This involves measuring blood glucose levels after an overnight fast. A result of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions indicates diabetes.
Another commonly used test is the oral glucose tolerance test (OGTT) which measures blood glucose levels before and two hours after consuming a glucose-rich drink. A result of 200 mg/dL or higher indicates diabetes.
Additionally, the glycated hemoglobin (HbA1c) test can provide information on long-term blood glucose control. An HbA1c level of 6.5% or higher indicates diabetes.
Treatment options
The treatment of diabetes aims to manage blood glucose levels and prevent complications. Treatment options may include:
- Lifestyle modifications: Healthy eating, regular physical activity, and weight management are key components of diabetes management. A balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, along with regular exercise, can help regulate blood glucose levels.
- Medications: In some cases, oral medications or injectable insulin may be prescribed to help manage blood glucose levels.
- Monitoring blood glucose levels: Regular monitoring of blood glucose levels is essential for diabetes management. This helps individuals make informed decisions about food choices, medication adjustments, and lifestyle modifications.
- Education and support: Diabetes education and support programs provide valuable information and resources to help individuals better manage their condition, make healthy choices, and cope with the daily challenges of living with diabetes.
Complications
Untreated or poorly managed diabetes can lead to various complications, affecting various organs and systems in the body. Some of the common complications include:
- Cardiovascular disease: Diabetes increases the risk of developing heart disease, including high blood pressure, heart attacks, and strokes.
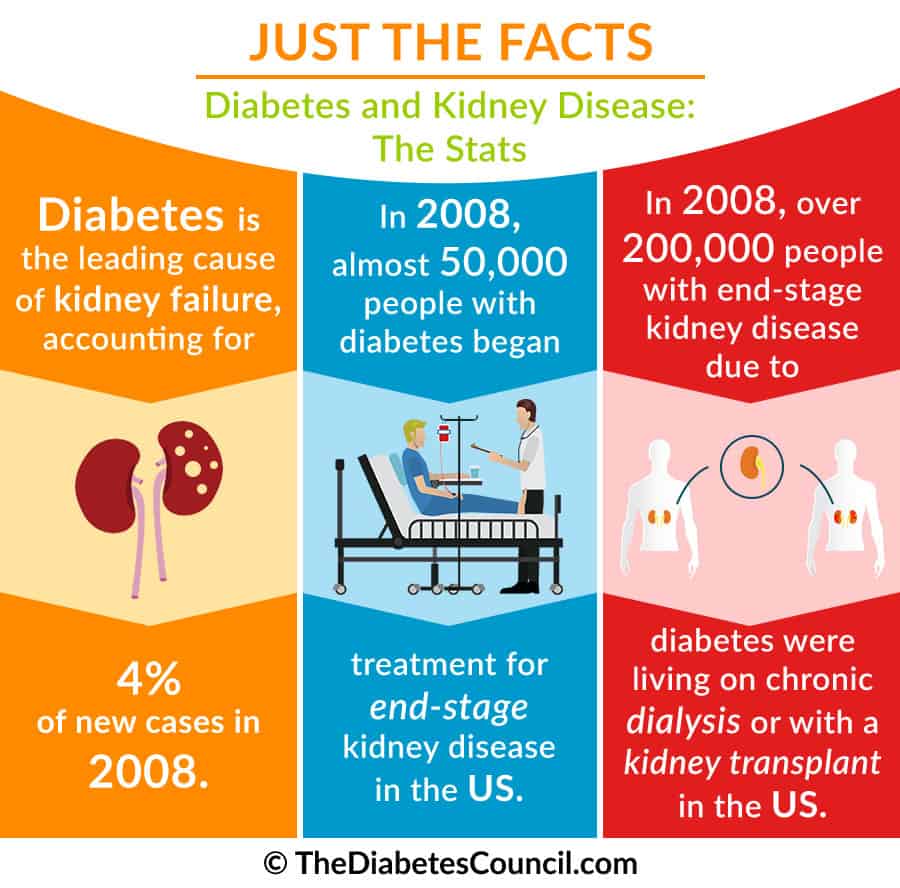
- Kidney disease (Diabetic nephropathy): Diabetes is a leading cause of chronic kidney disease, which can progress to end-stage renal disease (ESRD) and require dialysis or kidney transplantation.
- Eye problems (Diabetic retinopathy): High blood sugar levels can damage the blood vessels in the retina, leading to vision problems and, in severe cases, blindness.
- Nerve damage (Diabetic neuropathy): Diabetes can cause nerve damage, leading to symptoms such as numbness, tingling, or pain in the hands and feet.
- Foot complications: Diabetes can impair blood flow and nerve function in the feet, increasing the risk of foot ulcers, infections, and, in severe cases, the need for amputation.
- Increased susceptibility to infections: High blood sugar levels can weaken the immune system, making individuals more susceptible to infections, particularly urinary tract infections, skin infections, and gum disease.
The Connection between Diabetes and Acute Renal Failure
Introduction
The link between diabetes and Acute Renal Failure is significant, as diabetes is considered one of the leading causes of kidney disease. Diabetic nephropathy, a specific type of kidney damage caused by diabetes, can progress to Acute Renal Failure if not properly managed.
Prevalence of acute renal failure in diabetic patients
Diabetic patients have a higher risk of developing Acute Renal Failure compared to the general population. Research shows that individuals with diabetes are more likely to experience acute kidney injury, particularly those with uncontrolled blood glucose levels or long-standing diabetes.
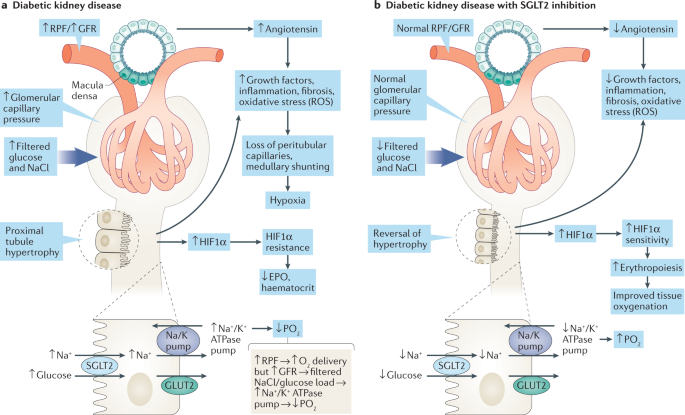
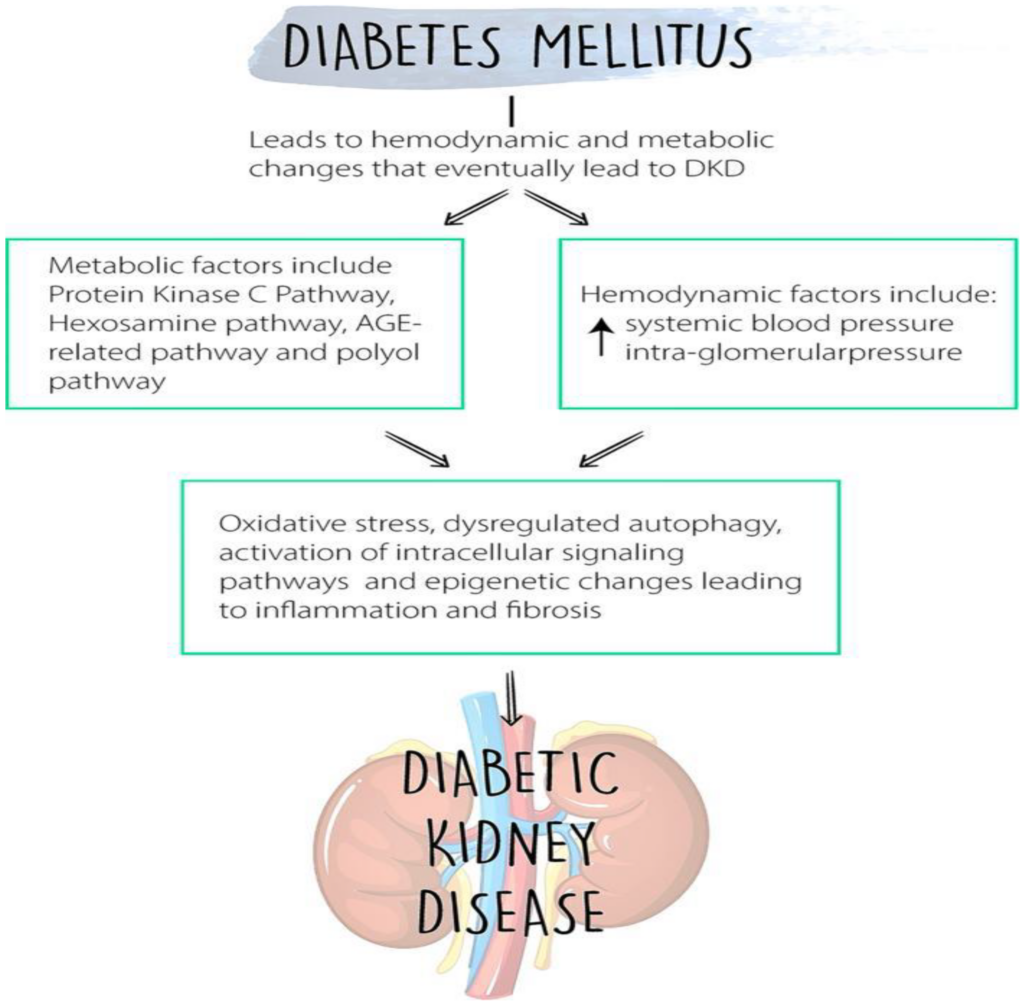
Understanding the pathophysiology
The pathophysiology, or the underlying mechanisms, of diabetes-related Acute Renal Failure involve complex interactions between various factors. Chronic high blood glucose levels in diabetes can lead to damage to the small blood vessels in the kidneys, impairing their function. This, coupled with underlying inflammation and oxidative stress, increases the risk of developing acute kidney injury.
Common risk factors for both conditions
Diabetes and Acute Renal Failure share several common risk factors. For instance, uncontrolled blood sugar levels, poor blood pressure control, and the presence of additional health conditions like obesity, cardiovascular disease, and chronic kidney disease can increase the risk of both diabetes-related kidney damage and Acute Renal Failure.
Impact of diabetes on renal function
Diabetes can have a significant impact on renal function. Over time, persistent high blood glucose levels can damage the blood vessels and small filtering units (glomeruli) in the kidneys, impairing their ability to filter waste products effectively. This can result in a progressive decline in kidney function and the development of diabetic nephropathy, which can ultimately progress to Acute Renal Failure.
Mechanisms linking diabetes and acute renal failure
Multiple interrelated mechanisms contribute to the connection between diabetes and Acute Renal Failure. These mechanisms include:
- Inflammation and oxidative stress: Chronic inflammation and oxidative stress in diabetes can contribute to kidney damage and inflammation, further exacerbating Acute Renal Failure.
- Hemodynamic changes: Diabetes can cause alterations in blood flow to the kidneys, leading to vasoconstriction (narrowing of blood vessels) and impaired filtration.
- Proteinuria and tubulointerstitial fibrosis: Diabetes-related kidney damage can result in the leakage of proteins into the urine (proteinuria) and the development of fibrous tissue within the kidney (tubulointerstitial fibrosis). These changes can impair renal function and contribute to Acute Renal Failure.
Understanding these mechanisms and their intricate relationship is crucial for the prevention and management of Acute Renal Failure in diabetic individuals.
Pathophysiology of Acute Renal Failure in Diabetes
Normal renal function
To understand the pathophysiology of Acute Renal Failure in diabetes, it is important to first understand the normal functioning of the kidneys. The kidneys play a vital role in maintaining fluid and electrolyte balance, filtering waste products from the blood, and producing urine. They consist of millions of tiny units called nephrons, which filter the blood and reabsorb essential substances.
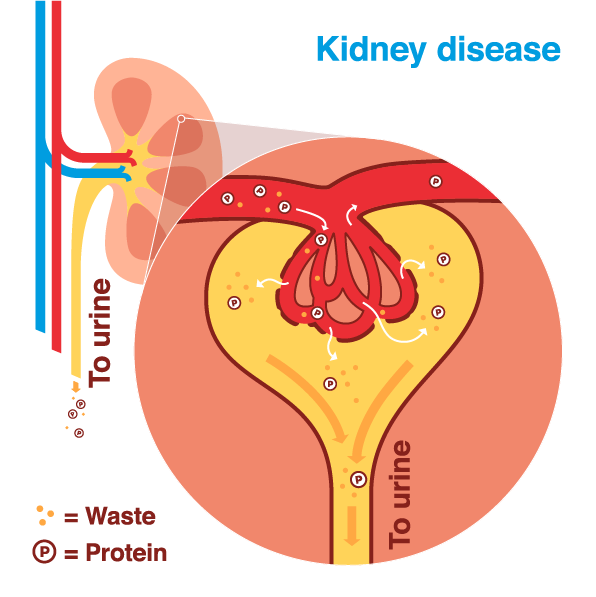
Diabetic nephropathy
Diabetic nephropathy is a specific type of kidney damage that occurs as a result of diabetes. It is characterized by the progressive deterioration of the glomeruli, the tiny blood vessels within the kidneys that filter waste products. Over time, the kidneys become less efficient at filtering waste, leading to proteinuria, and an increased excretion of proteins in the urine. This protein leakage can further damage the kidneys and contribute to the development of Acute Renal Failure.
Hemodynamic changes
In diabetes, there are significant changes in the hemodynamics, or blood flow dynamics, within the kidneys. Chronic high blood glucose levels can lead to the narrowing of blood vessels (vasoconstriction) and increased resistance to blood flow. This constriction reduces blood flow to the kidneys, impairing their ability to filter waste products effectively. Reduced blood flow also triggers the release of various hormones and vasoactive substances that further contribute to kidney damage.
Inflammation and oxidative stress
Diabetes is associated with chronic low-grade inflammation and increased oxidative stress in the body. Inflammation can lead to kidney damage by promoting the infiltration of immune cells and the release of pro-inflammatory factors that contribute to tissue injury. Oxidative stress, caused by an imbalance between reactive oxygen species (free radicals) and antioxidants, can further exacerbate kidney damage by inducing cellular damage and inflammation.
Proteinuria and tubulointerstitial fibrosis
The leakage of proteins into the urine, known as proteinuria, is a hallmark of both diabetic nephropathy and Acute Renal Failure. Excessive protein excretion further damages the glomeruli and impairs renal function. Additionally, the presence of high levels of proteins in the urine can lead to the deposition of fibrous tissue within the kidney, known as tubulointerstitial fibrosis. This fibrosis further impairs renal function and can contribute to the progression of Acute Renal Failure in diabetic individuals.
Understanding the pathophysiology of Acute Renal Failure in diabetes is essential for identifying potential therapeutic targets and developing more effective preventative and treatment strategies.
Clinical Presentation of Acute Renal Failure in Diabetes
Asymptomatic stage
In the early stages of Acute Renal Failure in diabetic individuals, there may be little to no noticeable symptoms. This asymptomatic stage can make early detection challenging, as individuals may not realize that their kidneys are being affected. Regular monitoring of kidney function is crucial for identifying any changes in renal function and preventing the progression to advanced stages.
Manifestations in advanced stages
As Acute Renal Failure progresses, symptoms become more apparent. Individuals may experience symptoms similar to those of non-diabetic patients with acute kidney injury. These symptoms include decreased urine output, swelling in the extremities, fatigue, shortness of breath, nausea, and confusion. At this stage, the kidney function is severely compromised, and immediate medical attention is necessary.
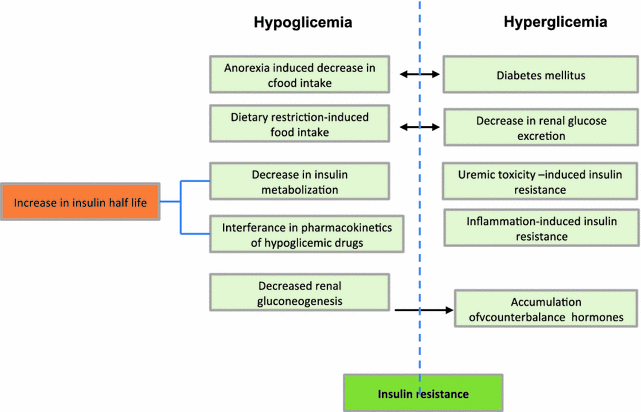
Specific symptoms in diabetic individuals
In addition to the common symptoms of Acute Renal Failure, diabetic individuals may experience symptoms specific to their underlying condition. For example, they may have difficulty managing blood glucose levels, which can contribute to hyperglycemia or hypoglycemia. They may also have challenges with medication adherence or insulin administration due to feeling unwell, further complicating blood glucose control.
Differences from acute renal failure without diabetes
While the clinical presentation of Acute Renal Failure may be similar in individuals with or without diabetes, the underlying pathophysiology and management approach can differ. Diabetic individuals may have other comorbidities, such as cardiovascular disease or peripheral neuropathy, which need to be considered in their overall care. Additionally, their response to certain medications or interventions may be influenced by their diabetes and kidney function.
Diagnosis of Acute Renal Failure in Diabetes
Medical history and physical examination
Diagnosing Acute Renal Failure in diabetes involves a comprehensive evaluation of the individual’s medical history, including any known risk factors or underlying conditions. The healthcare provider will also conduct a physical examination, looking for signs of fluid overload, high blood pressure, or other relevant findings. These initial assessments can provide valuable clues to guide diagnostic procedures.
Laboratory tests
Laboratory tests play a crucial role in diagnosing Acute Renal Failure in diabetes. Blood tests can measure creatinine levels, a waste product normally cleared by the kidneys, and estimate the glomerular filtration rate (GFR), which reflects kidney function. Elevated creatinine levels and a decreased GFR indicate impaired kidney function.
Urine tests are also used to assess kidney function and identify abnormalities. These tests may include measuring the amount of protein in the urine (proteinuria), which is a common sign of kidney damage.
Biopsy and imaging studies
In some cases, a kidney biopsy may be necessary to determine the underlying cause of Acute Renal Failure and guide treatment decisions. A kidney biopsy involves obtaining a small sample of kidney tissue for microscopic examination. This can provide valuable information about the extent and nature of kidney damage, such as diabetic nephropathy or other specific conditions.
Imaging studies, such as ultrasound, may also be used to assess the structure and function of the kidneys. These studies can help identify any structural abnormalities or obstructions that may be contributing to kidney dysfunction.
Distinguishing between different causes of renal dysfunction
Diagnosing Acute Renal Failure in diabetes requires distinguishing it from other potential causes of renal dysfunction, such as acute kidney injury due to infections or medication toxicity. A thorough assessment of medical history, laboratory tests, and imaging studies can help determine the underlying cause and guide appropriate treatment strategies.
Management of Acute Renal Failure in Diabetes
Controlling blood glucose levels
One of the key aspects of managing Acute Renal Failure in diabetes is achieving and maintaining optimal blood glucose control. Tight glycemic control can help minimize further kidney damage and improve overall outcomes. This may involve adjustments to insulin or medication dosages, frequent monitoring of blood glucose levels, and adherence to a well-balanced diet.
Addressing underlying causes
Managing Acute Renal Failure in diabetes requires identifying and addressing the underlying causes of kidney dysfunction. This may involve treating infections, reducing inflammation, managing blood pressure levels, or addressing any obstructions in the urinary tract.
Medications to preserve renal function
Certain medications may be prescribed to help preserve renal function and slow the progression of kidney damage. These medications may include angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which can help lower blood pressure and reduce proteinuria. Other medications, such as diuretics or erythropoiesis-stimulating agents, may be utilized to manage fluid balance and anemia.
Dietary modifications
Dietary modifications are often an important component of managing Acute Renal Failure in diabetes. A dietitian may work closely with the individual to develop a meal plan tailored to their specific needs. This may involve reducing sodium intake, limiting protein consumption, and monitoring phosphorus and potassium levels. Adequate fluid intake is essential to prevent dehydration but may need to be adjusted based on individual circumstances.
Lifestyle changes
Encouraging lifestyle changes, such as quitting smoking, increasing physical activity, and maintaining a healthy weight, can have a positive impact on kidney function and overall health. These changes may also help control other risk factors, such as high blood pressure or high cholesterol levels.
Monitoring and follow-up care
Regular monitoring of kidney function through blood tests, urine tests, and blood pressure measurements is essential in the management of Acute Renal Failure in diabetes. These monitoring protocols can help healthcare providers evaluate the effectiveness of treatment strategies and make any necessary adjustments. Regular follow-up visits with healthcare providers allow for ongoing assessment and optimization of care.
Complications and Prognosis
Long-term complications of acute renal failure
Acute Renal Failure can have long-term consequences on the overall health and well-being of individuals, particularly if not promptly and adequately managed. Some potential long-term complications include the development of chronic kidney disease, cardiovascular disease, and an increased risk of future episodes of Acute Renal Failure. The impact and severity of these complications may vary depending on various factors, such as the underlying cause, the extent of kidney damage, and the overall management approach.
Outcomes in diabetic patients
Diabetic individuals with Acute Renal Failure may experience different outcomes compared to individuals without diabetes. The presence of diabetes can complicate kidney function and impact the overall prognosis. Additionally, the management of diabetes, particularly blood glucose control, can influence outcomes and the progression of kidney damage. However, with appropriate management and timely interventions, many individuals with diabetes-related Acute Renal Failure can achieve successful outcomes and prevent further complications.
Prognostic factors
Several factors may influence the prognosis of Acute Renal Failure in diabetes. These factors may include the severity of kidney dysfunction, the presence of other health conditions, the response to treatment, and the overall management of diabetes and blood pressure. Early detection, prompt treatment, and adherence to recommended lifestyle modifications and medications can positively impact the prognosis.
Prevention and early intervention
Preventing Acute Renal Failure in diabetic individuals involves managing diabetes and its associated risk factors effectively. Optimal blood glucose control, regular monitoring of kidney function, maintaining a healthy weight, and managing blood pressure levels are crucial in preventing the progression of kidney damage. Early intervention and prompt treatment of kidney-related complications can also help minimize the risk of Acute Renal Failure and improve outcomes.
Preventive Measures for Diabetic Patients
Optimal glycemic control
Achieving and maintaining optimal blood glucose control is imperative in preventing kidney damage and Acute Renal Failure in diabetic individuals. This involves regular monitoring of blood glucose levels, adhering to prescribed medication regimens, and following a well-balanced diet. Diabetes management should be personalized and tailored to individual needs, taking into account other medical conditions and lifestyle factors.
Regular monitoring of kidney function
Regular monitoring of kidney function is essential in diabetic individuals to detect any early signs of kidney damage. This may involve routine blood tests to measure creatinine levels, urine tests to assess proteinuria, and blood pressure measurements. Monitoring protocols should be individualized based on the individual’s specific needs and risk factors.
Blood pressure management
Maintaining optimal blood pressure levels is crucial in preventing kidney damage and Acute Renal Failure in diabetes. Individuals with diabetes should aim for blood pressure levels below 130/80 mmHg, as recommended by professional guidelines. Medications, lifestyle modifications such as healthy eating and physical activity, and regular blood pressure monitoring are important components of blood pressure management.
Avoidance of nephrotoxic agents
Nephrotoxic agents, such as certain medications or substances, can worsen kidney function and increase the risk of Acute Renal Failure. Diabetic individuals should be cautious and avoid medications or substances that can harm the kidneys. This may involve working closely with healthcare providers to review medication regimens and discuss potential risks and alternatives.
Smoking cessation
Smoking is a significant risk factor for kidney disease and can exacerbate the damage caused by diabetes. Diabetic individuals who smoke should make every effort to quit smoking to reduce their risk of kidney damage and Acute Renal Failure. Supportive resources, such as smoking cessation programs or medications, can be utilized to aid in smoking cessation efforts.
Healthy lifestyle practices
Adopting and maintaining a healthy lifestyle is important for overall health and kidney protection in diabetes. This may include regular physical activity, following a balanced diet rich in fruits, vegetables, and whole grains, managing stress, and getting adequate sleep. These practices can support optimal blood glucose control, promote cardiovascular health, and reduce the risk of kidney damage and Acute Renal Failure.
Acute Renal Failure is a serious condition that can have devastating consequences if not promptly diagnosed and managed. The link between diabetes and Acute Renal Failure highlights the importance of optimal diabetes management, regular monitoring of kidney function, and early intervention to prevent or minimize kidney damage. By understanding the underlying pathophysiology, risk factors, symptoms, and management strategies, individuals with diabetes can take proactive steps to protect their kidneys and improve their overall health. Regular communication and collaboration with healthcare providers are essential in optimizing care and preventing the progression of kidney disease.
Watch This Video Below
Related Terms About The Link Between Diabetes and Acute Renal Failure
Acute Renal Failure In Diabetes, Can Diabetes Cause Aki, Diabetes And Acute Renal Failure, Diabetes Mellitus Kidney Failure Treatment, Diabetes Related To Kidney Failure, Diabetes With Acute Renal Failure, Does Diabetes Cause Acute Kidney Injury, How Does Diabetes Cause Aki, Relationship Between Diabetes And Kidney Failure, Why Do Kidneys Fail With Diabetes