Have you ever experienced abdominal pain or changes in your bowel habits? If so, you may be suffering from diverticular disease. In this article, we will explore the ins and outs of this condition, shedding light on its causes, symptoms, and potential complications. Understanding diverticular disease is crucial for taking control of your health and making informed decisions about your well-being. So, let’s dive into this article and discover everything you need to know about diverticular disease.

Definition of Diverticular Disease
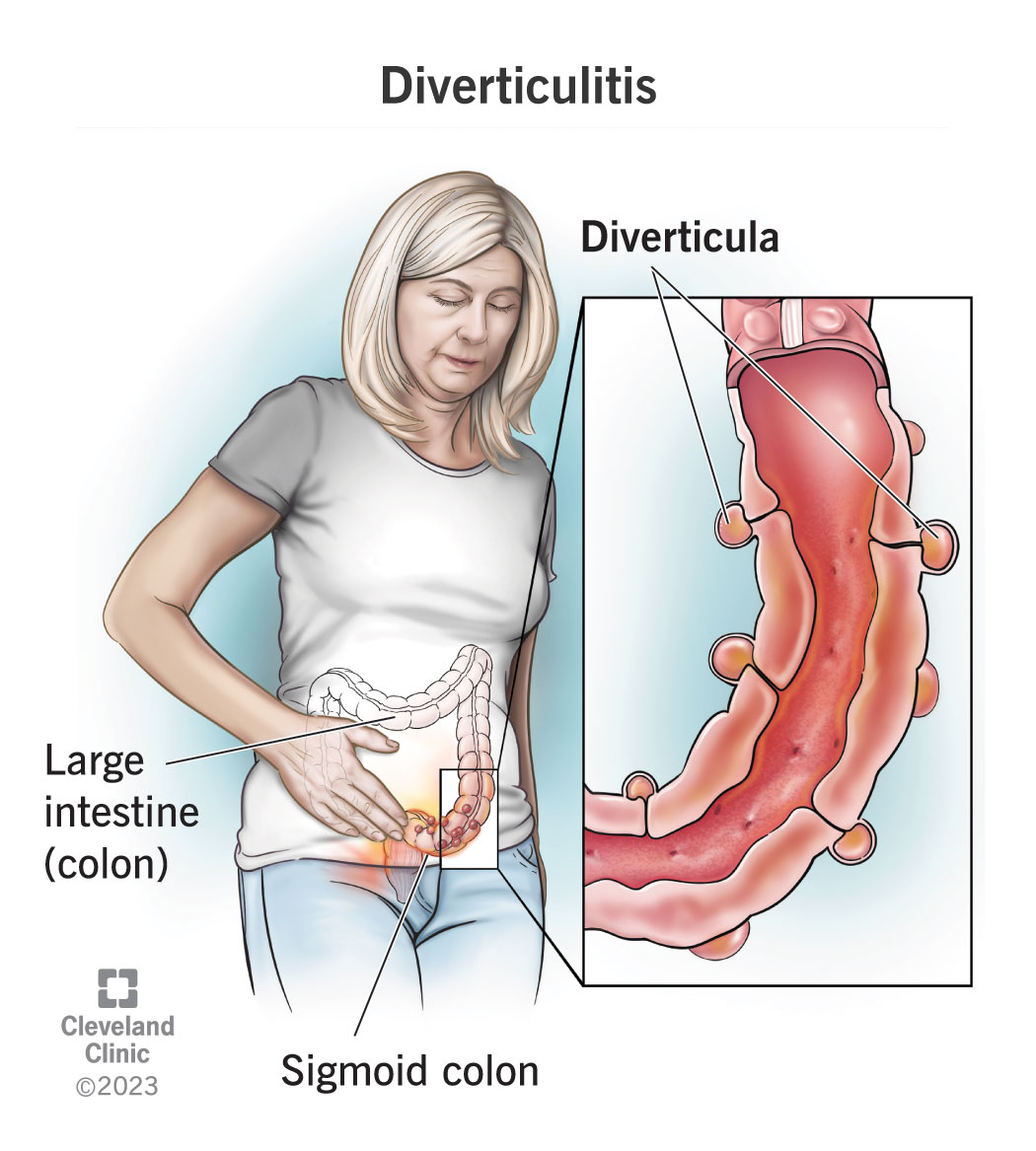
Diverticular disease is a condition that affects the colon, also known as the large intestine. It is characterized by the formation of small, bulging pouches called diverticula along the walls of the colon. These pouches are formed when weak spots in the colon’s muscle wall give way under pressure. While diverticula themselves are relatively harmless, they can become inflamed or infected, leading to various complications.
Diverticula formation
Diverticula form when high pressure inside the colon pushes against weak spots in the colon’s muscle layers. Over time, this pressure can cause small bulges to develop in the colon’s wall, resulting in diverticula. These diverticula are most commonly found in the lower part of the colon, known as the sigmoid colon.
Types of diverticula
There are two main types of diverticula: true diverticula and false diverticula. True diverticula involve all layers of the colon wall, while false diverticula only involve the outermost layer. Most diverticula in the colon are actually false diverticula.
Symptoms of diverticular disease
Diverticular disease can vary in severity and presentation, but some common symptoms include:
- Abdominal pain, particularly in the lower left side
- Bloating and flatulence
- Changes in bowel habits, such as constipation or diarrhea
- Rectal bleeding
- Fever and chills (indicating infection)
- Nausea and vomiting (indicating inflammation or obstruction)
It’s important to note that not everyone with diverticula will experience symptoms. In fact, many people may have diverticula without even realizing it, a condition known as diverticulosis.
Causes and Risk Factors
While the exact cause of diverticular disease is unknown, several factors have been identified as potential contributors to its development. These include:
Age
Diverticular disease is more common in older individuals, typically appearing after the age of 40. The risk increases with age, with the majority of cases being diagnosed in individuals over 60.
Diet
A low-fiber diet is believed to play a significant role in the development of diverticular disease. The consumption of processed foods, refined grains, and insufficient intake of fruits, vegetables, and whole grains can lead to reduced stool bulk and increased pressure in the colon.
Lifestyle factors
Certain lifestyle factors, such as sedentary behavior and obesity, have been associated with an increased risk of developing diverticular disease. Lack of physical activity can contribute to sluggish bowel movements and increased strain on the colon.
Genetic factors
There is evidence to suggest that genetics may play a role in the development of diverticular disease. If you have a family history of the condition, you may be at a higher risk of developing it yourself.

Diagnosis
Diagnosing diverticular disease involves a combination of medical history assessment, physical examination, and diagnostic tests. Common diagnostic procedures include:
Medical history and physical examination
Your doctor will start by asking about your symptoms, medical history, and any risk factors you may have. They may also perform a physical examination, such as gently pressing on your abdomen to check for tenderness or abnormal masses.
Colonoscopy
Colonoscopy involves inserting a flexible tube with a camera into the rectum and advancing it through the entire colon. This procedure allows your doctor to visualize the colon’s lining and can help identify any diverticula, inflammation, or other abnormalities.
Barium enema
During a barium enema, a liquid contrast called barium is inserted through the rectum and into the colon. X-rays are then taken to identify diverticula and evaluate the overall condition of the colon.
CT scan
A computed tomography (CT) scan may be ordered to obtain detailed cross-sectional images of the abdomen and pelvis. This imaging technique can help identify diverticula, assess inflammation, and detect complications such as abscesses or perforations.
Treatment Options
Treatment options for diverticular disease depend on the severity of symptoms and the presence of complications. The main treatment approaches include:
Dietary changes
Increasing fiber intake is a key component in managing diverticular disease. Fiber helps add bulk to the stool, making it easier to pass through the colon. This can help reduce the risk of diverticula becoming inflamed or infected. Foods rich in fiber include fruits, vegetables, whole grains, and legumes.
Medication
In some cases, your doctor may prescribe medications to manage symptoms or prevent complications. This may include pain relievers for abdominal discomfort, antibiotics for infections, and medications to regulate bowel movements.
Surgery
Surgery may be necessary if complications arise or if conservative treatment measures fail to provide relief. Depending on the specific case, surgical options range from removing the affected portion of the colon to creating a colostomy.

Complications of Diverticular Disease
If left untreated, diverticular disease can lead to various complications, including:
Diverticulitis
Diverticulitis occurs when diverticula become infected or inflamed. Symptoms of diverticulitis may include severe abdominal pain, fever, nausea, and changes in bowel habits. Prompt medical attention is crucial, as untreated diverticulitis can lead to serious complications.
Abscess
An abscess is a localized collection of pus that can develop when diverticula become infected. Abscesses can cause significant pain, fever, and general malaise. They may require drainage through a procedure performed by a healthcare professional.
Perforation
In rare cases, diverticula can rupture, leading to perforation of the colon. This is a medical emergency that requires immediate intervention. Peritonitis, an infection of the lining of the abdomen, can develop as a result of a perforation.
Bleeding
Diverticular bleeding occurs when blood vessels near diverticula rupture. This can lead to bright red blood in the stool or rectal bleeding. While most cases of diverticular bleeding resolve on their own, severe bleeding may require medical intervention.
Prevention
While diverticular disease cannot always be prevented, certain lifestyle modifications can help reduce the risk of developing complications. These include:
High-fiber diet
A diet rich in fiber can help prevent diverticula from becoming inflamed or infected. Aim to include plenty of fruits, vegetables, whole grains, and legumes in your daily meals.
Adequate hydration
Staying well-hydrated is important to maintain healthy bowel function. Ensure you drink enough fluids throughout the day, particularly water and other non-caffeinated beverages.
Regular exercise
Engaging in regular physical activity can help regulate bowel movements and reduce the risk of constipation. Aim for at least 30 minutes of exercise most days of the week.
Quitting smoking
Smoking has been associated with an increased risk of developing diverticular disease and complications. If you smoke, quitting can significantly improve your overall health and reduce the risk of various diseases.
Lifestyle Modifications for Diverticular Disease
Besides the preventative measures mentioned above, there are several lifestyle modifications that can help manage symptoms and reduce the risk of flare-ups:
Exercise
Regular exercise not only promotes overall health but can also help regulate bowel movements and alleviate constipation. Incorporating activities such as walking, swimming, or cycling into your routine can provide numerous benefits.
Stress reduction
Stress can worsen symptoms of diverticular disease and trigger flare-ups. Finding effective stress management techniques, such as practicing mindfulness or engaging in relaxation exercises, can help reduce the impact of stress on your digestive system.
Smoking cessation
As mentioned earlier, smoking is a risk factor for diverticular disease. If you smoke, quitting can significantly improve your condition and reduce the risk of complications.
Weight management
Maintaining a healthy weight can help prevent the onset of diverticular disease and reduce symptoms. Adopting a balanced diet and engaging in regular physical activity can aid in weight management.
Frequently Asked Questions
What is the difference between diverticulosis and diverticulitis?
Diverticulosis refers to the presence of diverticula in the colon without any inflammation or infection. It is usually asymptomatic. On the other hand, diverticulitis occurs when diverticula become inflamed or infected, leading to symptoms such as abdominal pain, fever, and changes in bowel habits.
Can diverticular disease lead to colorectal cancer?
There is no direct link between diverticular disease and colorectal cancer. However, diverticular disease and colorectal cancer can coexist. It is essential to undergo regular colonoscopies to screen for and detect any signs of colorectal cancer.
How is diverticular disease managed during flare-ups?
During flare-ups of diverticular disease, your doctor may recommend a combination of antibiotics, dietary modifications (such as a clear liquid or low-residue diet), and pain management. In severe cases, hospitalization may be required for intravenous antibiotics and other supportive measures.

Conclusion
Diverticular disease is a common condition characterized by the development of diverticula in the colon. While often asymptomatic, it can lead to complications such as diverticulitis, abscesses, perforation, and bleeding. Lifestyle modifications, including dietary changes, regular exercise, stress reduction, and smoking cessation, can play a significant role in preventing symptoms and reducing the risk of flare-ups. Early diagnosis and appropriate treatment are essential to managing diverticular disease. If you experience any concerning symptoms, it is important to consult with your healthcare provider for a proper evaluation and guidance.