You’ve probably heard of diseases caused by parasites, but have you ever heard of Echinococcosis? This lesser-known disease, also known as hydatid disease, is caused by a type of tapeworm that can infect both humans and animals. In this article, we will explore the causes, symptoms, and treatment options available for Echinococcosis, shedding light on this often misunderstood condition. So, get ready to expand your knowledge and learn more about this intriguing disease.
Causes of Echinococcosis
Echinococcosis is caused by the parasitic tapeworms belonging to the Echinococcus genus. There are several ways in which this disease can be transmitted:
Transmission through infected animals
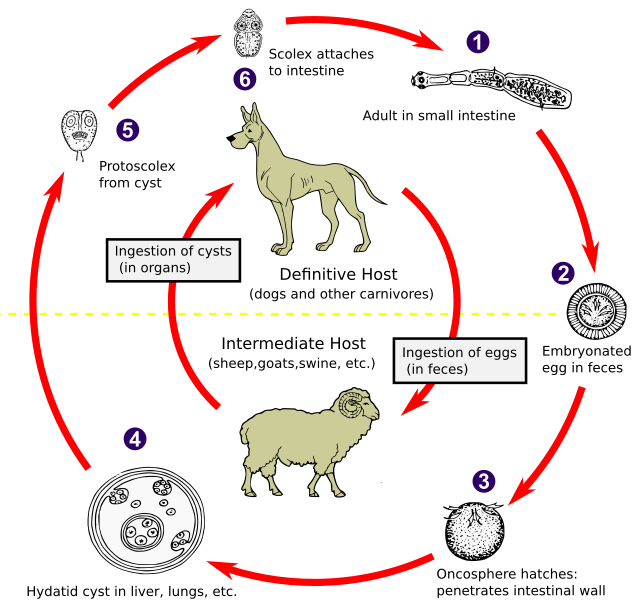
The primary mode of transmission of Echinococcosis is through contact with infected animals. Dogs are known to be the main hosts of these tapeworms, and by ingesting their eggs, humans can become infected. This can occur when you come into contact with contaminated soil, water, or food that has been contaminated with the feces of infected dogs. It is important to note that other animals, such as sheep, goats, and cattle, can also act as intermediate hosts and may transmit the disease to humans.
Ingestion of parasite eggs
Another common mode of transmission is through the ingestion of parasite eggs. These microscopic eggs, which are present in the feces of infected animals, can contaminate the environment and persist for long periods of time. If you accidentally ingest these eggs, for example, through contaminated food or water, you may become infected with Echinococcosis.
Occupational exposure
Certain occupations can put you at a higher risk of contracting Echinococcosis. Individuals working in agriculture, such as farmers, as well as those involved in animal husbandry or veterinary practices, have an increased risk of exposure to the parasite. This can occur through direct contact with infected animals or contaminated environments.
Geographical and environmental factors
The risk of acquiring Echinococcosis also depends on geographical and environmental factors. The disease is more commonly found in rural areas where there is an interaction between animals and humans, such as farming communities. Poor sanitation, lack of access to clean water, and inadequate hygiene practices can further contribute to the spread of the disease.
Symptoms of Echinococcosis
Echinococcosis can cause a wide range of symptoms, depending on the location and size of the cysts. These symptoms can be categorized into the following:
Asymptomatic infection
In many cases, Echinococcosis may remain asymptomatic, meaning there are no apparent symptoms. This can make the diagnosis challenging, as the infection can go unnoticed for a significant period of time. It is important to note that even without symptoms, the parasite can still cause damage to internal organs.
Localized symptoms
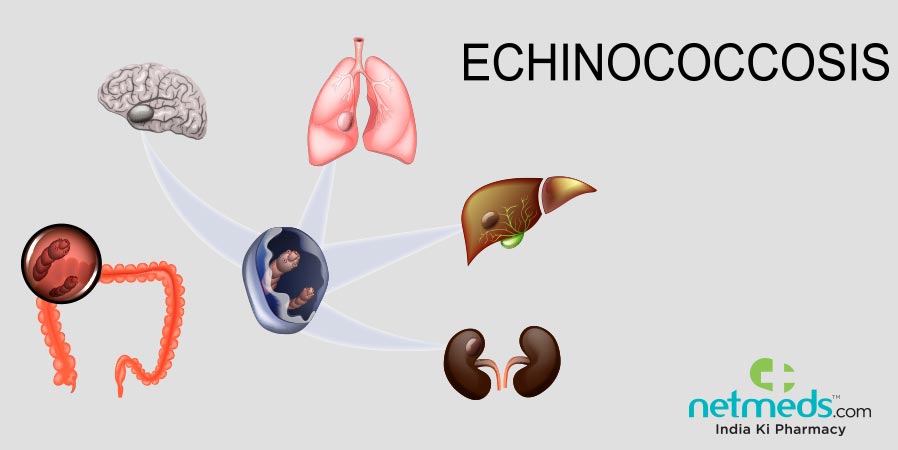
When symptoms do manifest, they are often localized to the site of the cysts. For example, cysts located in the liver can cause abdominal pain, hepatomegaly (enlargement of the liver), and jaundice. Similarly, if the cysts are present in the lungs, you may experience coughing, chest pain, or difficulty breathing.
Obstruction and compression symptoms
As the cysts grow larger, they can obstruct or compress nearby structures, leading to specific symptoms. For instance, if the cysts are located near the bile ducts, it can result in bile duct obstruction and cause symptoms like jaundice and clay-colored stools. Compression of blood vessels or structures in the lungs can lead to symptoms such as hemoptysis (coughing up blood) or chest pain.
Allergic reactions
In some cases, the presence of the cysts can trigger an allergic reaction. This can manifest as fever, rash, eosinophilia (increase in eosinophil count), or anaphylaxis in severe cases. Allergic reactions are more commonly associated with the rupture of cysts, as the release of cyst contents into the bloodstream can trigger an immune response.
Diagnosis of Echinococcosis
Early and accurate diagnosis of Echinococcosis is crucial for effective treatment. Various diagnostic methods are employed to confirm the presence of the infection:
Clinical evaluation
A thorough clinical evaluation is the first step in diagnosing Echinococcosis. Your healthcare provider will review your medical history, conduct a physical examination, and consider any symptoms or risk factors that may suggest the presence of the disease. However, clinical evaluation alone is not sufficient for a definitive diagnosis.
Imaging techniques
Imaging techniques play a significant role in diagnosing Echinococcosis. Imaging tests such as ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) can help visualize the cysts and determine their location, size, and extent of involvement. These imaging modalities provide valuable information for treatment planning and monitoring disease progression.
Serological tests
Serological tests are blood tests that detect specific antibodies produced by your immune system in response to the Echinococcus tapeworm. These tests, such as enzyme-linked immunosorbent assay (ELISA) or indirect hemagglutination assay (IHA), can aid in confirming the diagnosis and differentiating between different types of Echinococcosis.
Biopsy and histopathological examination
In some cases, a biopsy may be required to definitively diagnose Echinococcosis. This involves obtaining a tissue sample from the affected organ and examining it under a microscope. Biopsy and histopathological examination can provide information about the type of cyst and the extent of tissue damage caused by the parasite.
Types of Echinococcosis
Echinococcosis can manifest in several different forms, depending on the species of the Echinococcus tapeworm and the organs affected. The most common types of Echinococcosis include:
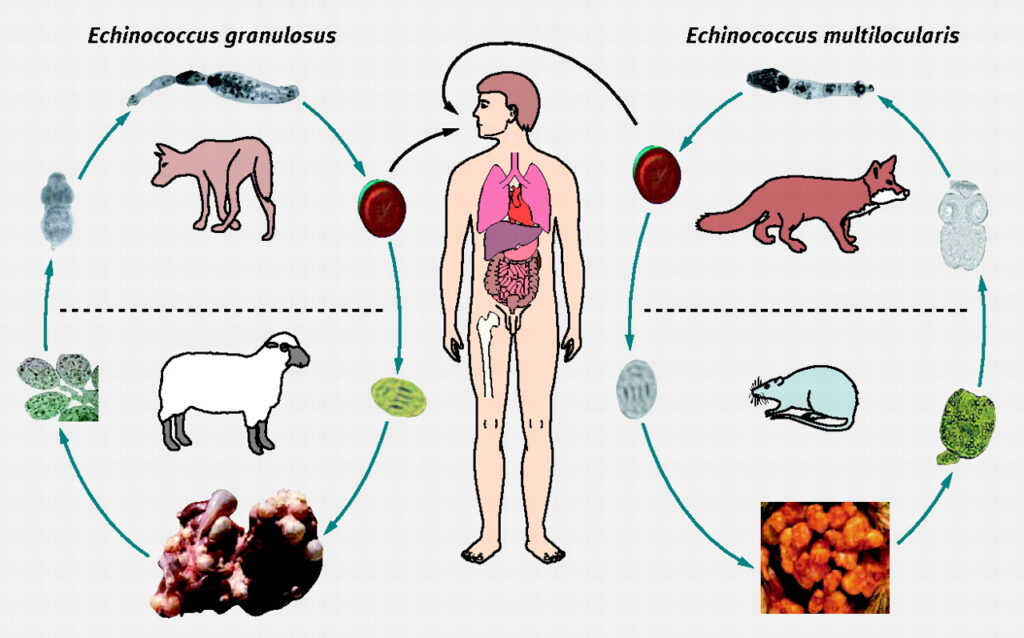
Cystic echinococcosis
Cystic echinococcosis, or hydatid disease, is caused by the Echinococcus granulosus tapeworm. This form of the disease primarily affects the liver and lungs. However, the cysts can potentially affect any organ in the body, including the brain, heart, and bones. Cystic echinococcosis is characterized by the formation of large fluid-filled cysts known as hydatid cysts.
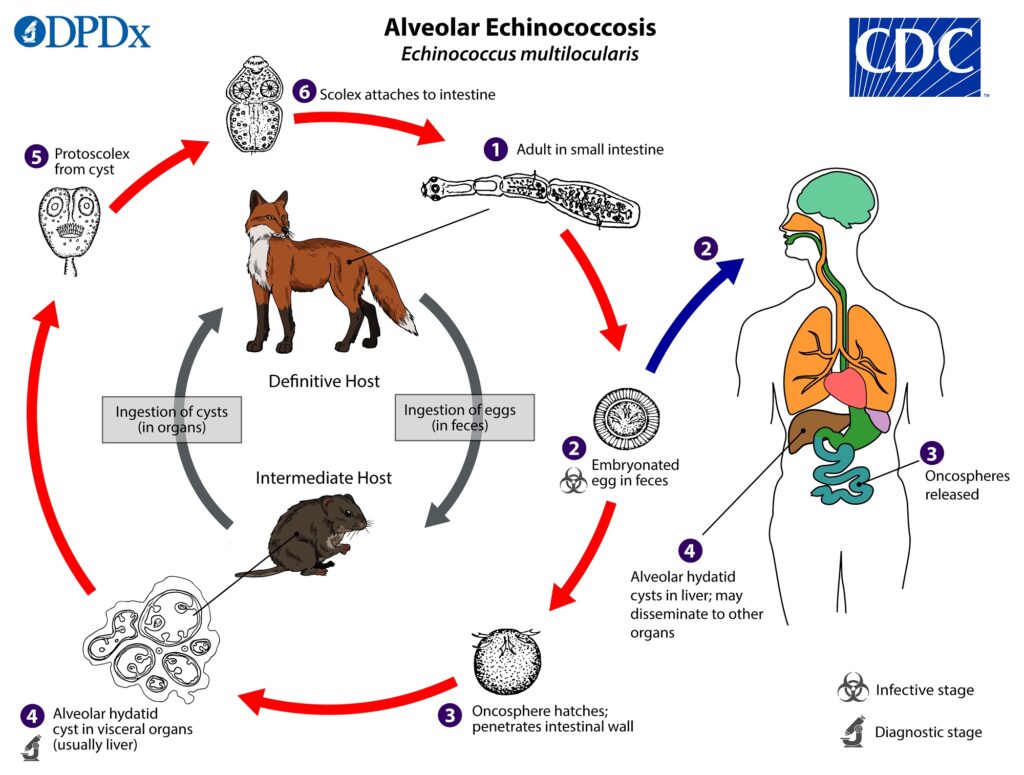
Alveolar echinococcosis
Alveolar echinococcosis is caused by the Echinococcus multilocularis tapeworm. This form of the disease primarily affects the liver, and if left untreated, it can invade adjacent structures and spread throughout the body. Alveolar echinococcosis is characterized by the infiltration of the liver tissue by tumor-like lesions, resembling alveoli.
Polycystic echinococcosis
Polycystic echinococcosis, also known as polycystic hydatid disease, is caused by the Echinococcus vogeli and Echinococcus oligarthrus tapeworms. This form of the disease primarily affects the liver; however, cysts can also be found in the lungs, spleen, and other organs. Polycystic echinococcosis is characterized by the presence of numerous small cysts within the affected organ.
Unilocular hydatid disease
Unilocular hydatid disease is another form of cystic echinococcosis that primarily affects the liver. It is caused by the Echinococcus vogeli tapeworm. Unlike the typical hydatid cysts seen in cystic echinococcosis, unilocular hydatid disease is characterized by the presence of a single chamber within the cyst.
Multilocular hydatid disease
Multilocular hydatid disease is an advanced form of alveolar echinococcosis. It is characterized by the infiltration of the liver tissue by tumor-like lesions that resemble a multilocular mass. Unlike alveolar echinococcosis, multilocular hydatid disease does not involve the formation of cysts but has a similar pattern of tissue destruction and invasion.
Complications of Echinococcosis
Echinococcosis can lead to various complications, especially when left untreated or poorly managed. These complications can significantly impact an individual’s health and well-being:
Rupture of cysts
One of the most serious complications of Echinococcosis is the rupture of cysts. This can occur spontaneously or as a result of trauma or surgical manipulation. When a cyst ruptures, the contents, including the parasite, are released into the body, leading to an acute immune response. This can cause anaphylaxis, severe inflammation, and potentially life-threatening complications.
Secondary bacterial infections
Infection of the cysts with bacteria is another complication of Echinococcosis. When the cysts rupture or become infected, bacteria can enter the cysts and cause secondary bacterial infections. These infections can lead to the formation of abscesses, which are collections of pus, and can result in severe localized symptoms and general infection.
Dissemination to other organs
If left untreated, Echinococcosis can spread to other organs and tissues. This can occur through the dissemination of the parasite via the bloodstream or lymphatic system. When the tapeworm larvae reach other organs, they can form new cysts, leading to the involvement of multiple organs and further complicating the management of the disease.
Cancerous transformation (in alveolar echinococcosis)
In cases of alveolar echinococcosis, the slow-growing tumor-like lesions can undergo cancerous transformation. This can result in the development of invasive malignant tumors and metastasis to other organs. The cancerous transformation significantly worsens the prognosis and treatment outcomes for individuals with alveolar echinococcosis.
Treatment Options for Echinococcosis
The treatment of Echinococcosis depends on several factors, such as the type and location of the cysts, the extent of organ involvement, and the overall health of the individual. Treatment options may include:
Surgery
Surgical removal of the cysts is the primary treatment for Echinococcosis. It aims to completely remove the cysts while minimizing damage to surrounding tissues. The surgical approach will depend on the type and location of the cysts. In some cases, it may be possible to remove the cysts laparoscopically, which involves making small incisions and using specialized instruments for removal.
Medical treatments
In addition to surgery, medication may be prescribed to treat Echinococcosis. Albendazole and mebendazole are the most commonly used drugs. These medications work by inhibiting the growth and reproduction of the parasite. Medical treatment is often used in combination with surgery to reduce the risk of recurrence and manage any residual infection.
Percutaneous treatments
Percutaneous treatments, such as percutaneous aspiration, injection, and reaspiration (PAIR), may be an option for certain types and sizes of cysts. This minimally invasive procedure involves puncturing the cyst under imaging guidance, aspirating the cyst contents, and injecting a scolicidal agent to kill any remaining parasites. Percutaneous treatments are typically used for smaller cysts or as an adjunct to other treatments.
Monitoring and follow-up
After treatment, regular monitoring and follow-up are essential to ensure the effectiveness of the chosen treatment approach. Imaging tests, such as ultrasound or CT scans, may be performed periodically to evaluate the status of the cysts and assess any potential recurrence or complications. Additionally, laboratory tests, including serological tests, may be used to monitor the response to treatment and detect any residual infection.

Prevention and Control of Echinococcosis
Prevention and control measures play a crucial role in reducing the burden of Echinococcosis. Here are some key strategies:
Promotion of good hygiene practices
Practicing good hygiene is essential in preventing the transmission of Echinococcosis. This includes washing hands thoroughly with soap and water, especially after contact with animals or contaminated environments. Avoiding the consumption of raw or undercooked food, particularly organs from infected animals, can also help reduce the risk of infection.
Regular deworming of dogs
As dogs are the primary hosts for Echinococcus tapeworms, regular deworming is crucial in preventing the spread of the disease. Administering anthelmintic medications to dogs helps eliminate any tapeworms they may be harboring, reducing the risk of contamination of the environment and transmission to humans.
Avoidance of contact with stray dogs
Avoiding contact with stray dogs can reduce the risk of exposure to Echinococcus tapeworms. Stray dogs are more likely to be infected with the parasite and can contribute to the contamination of the environment. If you encounter a stray dog, it is important to maintain a safe distance and avoid contact with its feces or urine.
Proper disposal of animal waste
Proper disposal of animal waste, particularly from infected animals, is essential in preventing the spread of Echinococcosis. Ensuring that waste is disposed of in a way that minimizes environmental contamination, such as burying it or using specialized waste management systems, helps reduce the risk of transmission.
Epidemiology of Echinococcosis
Echinococcosis is a global health concern, with a significant impact on various populations. The disease is endemic in many parts of the world, particularly in rural and agricultural communities. The distribution of Echinococcosis is influenced by various factors, including geographical, environmental, and socio-economic conditions.
Global distribution
Echinococcosis is found in both developed and developing countries. It is prevalent in regions where there is close contact between humans and animals, such as Africa, Asia, Europe, and parts of South America. The disease is particularly common in areas with a large population of livestock, as they serve as intermediate hosts for the tapeworms.
High-risk populations
Certain populations are at a higher risk of contracting Echinococcosis. Individuals engaged in livestock farming, herding, or veterinary practices are at an increased risk due to their close contact with infected animals. Additionally, individuals living in rural and remote areas with poor sanitation and limited access to healthcare are more vulnerable to the disease.
Economic and social impact
Echinococcosis poses a significant economic and social burden on affected communities. The disease affects agricultural productivity, as infected animals may have reduced weight gain or decreased milk production. It also impacts the livelihood of individuals engaged in farming and animal husbandry. Additionally, the cost of healthcare, including diagnosis and treatment, can be a significant financial burden for affected individuals and their families.
Public Health Strategies for Echinococcosis
To combat Echinococcosis effectively, public health strategies are essential. These strategies encompass various approaches to prevent, detect, and control the disease:
Surveillance and reporting systems
Robust surveillance and reporting systems are crucial in monitoring the occurrence and distribution of Echinococcosis. This involves collecting data on cases, identifying high-risk areas, and tracking any changes in disease patterns. Prompt reporting of cases helps authorities implement timely interventions and allocate resources effectively.
Education and awareness campaigns
Educating communities about the causes, modes of transmission, and prevention of Echinococcosis is vital to raising awareness and promoting behavior change. Public health campaigns, educational materials, and community engagement initiatives can provide information on the disease, its impact, and the importance of adopting preventive measures. By increasing knowledge and understanding, individuals can take appropriate actions to protect themselves and their communities.
Research and innovation
Ongoing research and innovation are critical in advancing our understanding of Echinococcosis and developing new tools and strategies for prevention, diagnosis, and treatment. This includes studying the epidemiology and risk factors of the disease, exploring new diagnostic methods, and investigating potential therapies or vaccines.
Collaboration and international cooperation
Addressing the complex challenges posed by Echinococcosis requires collaboration and international cooperation. Cooperation between countries, organizations, and health agencies facilitates the exchange of knowledge, resources, and best practices. This fosters more effective prevention and control strategies, ultimately reducing the global burden of Echinococcosis.
Conclusion
Echinococcosis is a parasitic disease caused by tapeworms of the Echinococcus genus. It can be transmitted through contact with infected animals, ingestion of parasite eggs, occupational exposure, and various geographical and environmental factors. The disease can manifest with a wide range of symptoms, from asymptomatic infection to localized symptoms and complications such as cyst rupture and secondary bacterial infections.
Diagnosis of Echinococcosis involves clinical evaluation, imaging techniques, serological tests, and biopsy. Different types of Echinococcosis exist, including cystic echinococcosis, alveolar echinococcosis, polycystic echinococcosis, unilocular hydatid disease, and multilocular hydatid disease. The disease can result in various complications, including cyst rupture, secondary infections, dissemination to other organs, and cancerous transformation in alveolar echinococcosis.
Treatment options for Echinococcosis include surgery, medical treatments, percutaneous treatments, and monitoring. Prevention and control measures consist of promoting good hygiene practices, regular deworming of dogs, avoidance of contact with stray dogs, and proper disposal of animal waste. Echinococcosis has a global distribution and affects high-risk populations, with significant economic and social impacts. Public health strategies are crucial in tackling Echinococcosis, focusing on surveillance, education, research, and collaboration.
By increasing awareness, implementing preventive measures, and advancing research and interventions, we can work towards reducing the burden of Echinococcosis and improving the health and well-being of affected individuals and communities worldwide.