You’ve heard of heartburn, but do you really know what causes it? In our article “Understanding Gastroesophageal Reflux Disease (GERD)”, we explore the ins and outs of this common condition that affects millions of people worldwide. From understanding the symptoms to learning about potential treatment options, this comprehensive guide will help you gain a better understanding of GERD and how to manage it effectively. So, if you’re tired of that burning sensation in your chest, read on to discover all you need to know about GERD.

What is Gastroesophageal Reflux Disease?
Definition:
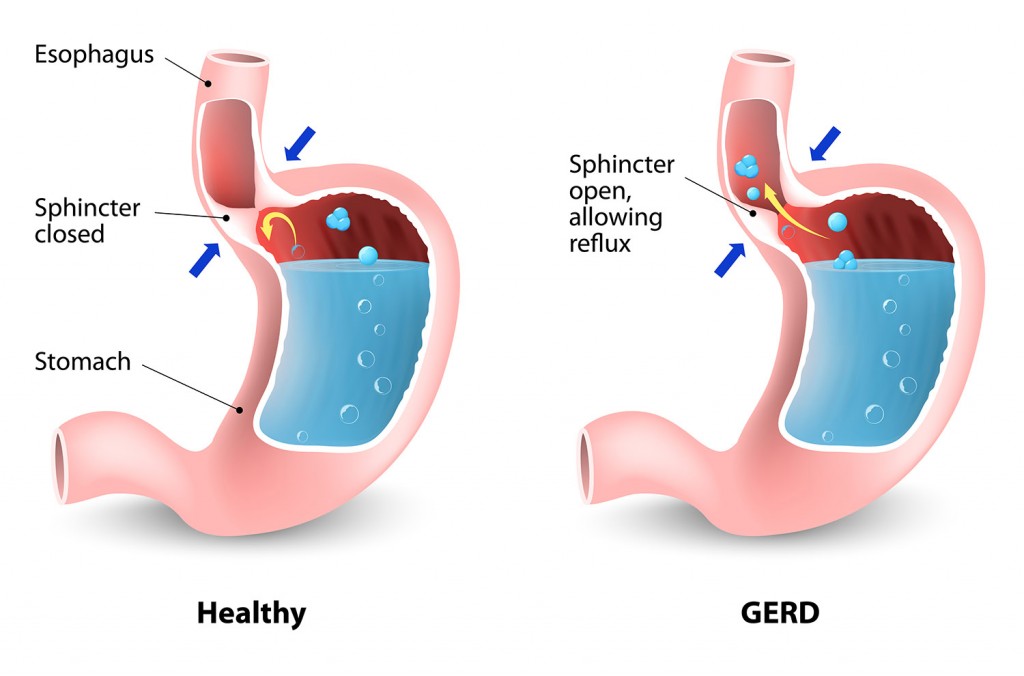
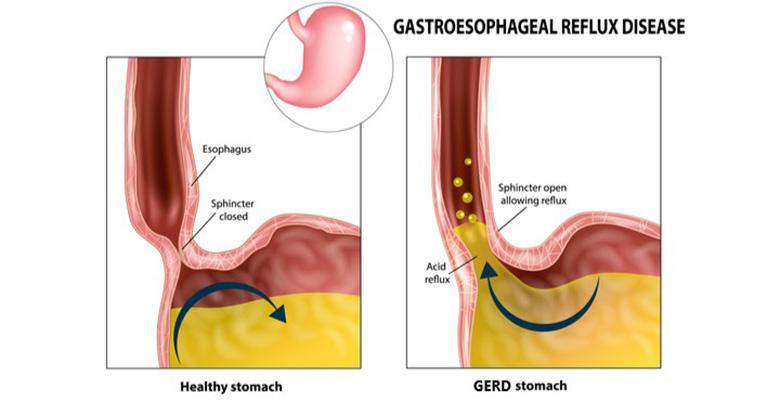
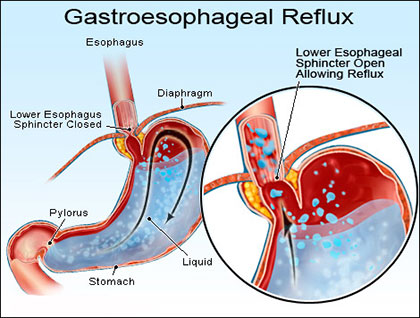
Gastroesophageal reflux disease (GERD) is a chronic condition that occurs when stomach acid flows back into the esophagus, causing irritation and inflammation. The lower esophageal sphincter (LES), a muscular ring that acts as a barrier between the stomach and the esophagus, becomes weak or relaxes inappropriately, allowing stomach acid to escape into the esophagus. This reflux of acid can lead to various symptoms and complications if left untreated.
Causes of GERD:
Several factors can contribute to the development of GERD. It is commonly caused by a dysfunction of the lower esophageal sphincter, allowing acid to reflux. Other factors that can increase the risk of GERD include obesity, hiatal hernia, pregnancy, certain medications such as NSAIDs and calcium channel blockers, smoking, and consuming certain types of food and beverages.
Symptoms:
The symptoms of GERD can vary from person to person, but common symptoms include heartburn, regurgitation of stomach acid or food, chest pain, difficulty swallowing (dysphagia), a chronic cough, hoarseness, sore throat, and a sensation of a lump in the throat. These symptoms can significantly impact a person’s quality of life and may occur intermittently or persistently.
Diagnosis of GERD
Medical History:
When diagnosing GERD, your healthcare provider will begin by taking a detailed medical history, including a discussion of your symptoms, their frequency, and their impact on your daily life. It is important to mention any medications you are currently taking and any other medical conditions you may have.
Physical Examination:
A physical examination may be performed to assess for any signs of complications or underlying conditions that may contribute to GERD. Your healthcare provider may also examine your abdomen and chest to check for any signs of inflammation or discomfort.
Tests and Procedures:
In some cases, additional tests and procedures may be necessary to confirm the diagnosis of GERD and evaluate its severity. These tests may include:
- Esophageal pH monitoring: A probe is placed in the esophagus to measure acid levels over a 24-hour period.
- Upper endoscopy: A thin, flexible tube with a camera is inserted through the mouth and into the esophagus to examine the lining for signs of inflammation or damage.
- Esophageal manometry: This test measures the pressure and coordination of the muscles in the esophagus.
- Barium swallow: You will swallow a contrast liquid, which will help visualize the esophagus and detect any abnormalities.
- X-rays: These may be used to evaluate the esophagus and surrounding structures.
Treatment Options for GERD
Lifestyle Changes:
The first-line treatment for GERD often involves making certain lifestyle changes to reduce symptoms and improve overall esophageal health. These changes may include:
- Elevating the head of the bed to prevent acid reflux during sleep.
- Avoiding trigger foods and beverages that can worsen symptoms.
- Eating smaller, more frequent meals to reduce pressure on the LES.
- Avoiding lying down immediately after meals.
- Losing weight if overweight or obese.
- Quitting smoking, as it can worsen symptoms of GERD.
Medications:
Medications may be prescribed to reduce symptoms and suppress the production of stomach acid. Commonly used medications for GERD include:
- Antacids: Over-the-counter antacids can provide temporary relief by neutralizing stomach acid.
- H2 blockers: These medications reduce the production of stomach acid and can provide longer-lasting relief.
- Proton pump inhibitors (PPIs): PPIs are potent acid reducers and are often prescribed for more severe cases of GERD. They can help heal the esophagus and prevent further damage.
- Prokinetics: These medications help improve the movement of the digestive tract, reducing the amount of acid that refluxes into the esophagus.
Surgical Intervention:
When lifestyle changes and medications are not effective in managing GERD, surgical intervention may be considered. The most common surgical procedure for GERD is laparoscopic fundoplication, where the upper part of the stomach is wrapped around the LES to strengthen it and prevent acid reflux. Other procedures, such as magnetic sphincter augmentation (LINX) and endoscopic treatments, may also be options for certain individuals.
Complications of GERD
Esophagitis:
Untreated or poorly managed GERD can lead to the development of esophagitis, which is inflammation of the esophagus. This inflammation can cause pain, difficulty swallowing, and the formation of open sores or ulcers in the esophageal lining.
Barrett’s Esophagus:
Barrett’s esophagus is a condition that can develop as a result of long-term untreated GERD. It occurs when the lining of the esophagus changes to resemble the lining of the intestines, increasing the risk of esophageal cancer.
Stricture:
Repeated exposure to stomach acid can cause scar tissue to form in the esophagus, resulting in narrowing or strictures. These strictures can make swallowing difficult and may require treatment or dilation procedures to relieve the blockage.
Respiratory Issues:
In some individuals, the reflux of stomach acid can reach the throat and even the lungs, leading to respiratory symptoms such as chronic cough, asthma, or recurrent pneumonia. It is important to address these respiratory issues as they can significantly impact a person’s quality of life.
Diet and GERD
Foods to Avoid:
Certain foods and beverages can trigger or worsen GERD symptoms. It is advised to avoid or limit the intake of the following:
- Spicy and fatty foods
- Citrus fruits and juices
- Tomatoes and tomato-based products
- Chocolate
- Carbonated beverages
- Coffee and tea (caffeinated and decaffeinated)
- Alcohol
- Peppermint and spearmint
Foods to Eat:
While individual food triggers can vary, the following foods are generally considered more tolerable for individuals with GERD:
- Lean proteins, such as chicken, fish, and tofu
- Whole grains, including oats, brown rice, and quinoa
- Non-citrus fruits, such as bananas, melons, and apples
- Vegetables, except for highly acidic options like tomatoes and onions
- Low-fat dairy products, such as skim milk and yogurt
- Healthy fats, such as olive oil and avocado
Tips for Managing GERD Symptoms
Elevating the head of the bed:
By using additional pillows or raising the head of the bed by a few inches, gravity can help prevent stomach acid from flowing back into the esophagus during sleep.
Avoiding Triggers:
Identify and avoid trigger foods and beverages that worsen your GERD symptoms. Keeping a food diary can help you identify patterns and make necessary changes to your diet.
Eating Small, Frequent Meals:
Instead of consuming large, heavy meals, opt for smaller, more frequent meals throughout the day. This can help reduce pressure on the LES and minimize the likelihood of acid reflux.
Natural Remedies for GERD
Ginger:
Ginger has long been used for its digestive properties and can help alleviate symptoms of GERD. It can be consumed as ginger tea, added to meals, or taken as a supplement.
Aloe Vera Juice:
Aloe vera juice has a soothing effect on the digestive system and can help reduce irritation and inflammation in the esophagus. It is important to choose pure, organic aloe vera juice and consult with a healthcare provider before incorporating it into your routine.
Apple Cider Vinegar:
Although it may seem counterintuitive, apple cider vinegar can help balance stomach acid levels and improve digestion. However, it should be consumed in small amounts and diluted with water to prevent further acid reflux.
Preventing GERD
Maintaining a Healthy Weight:
Excess weight can put pressure on the abdomen, pushing stomach contents back into the esophagus. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce the risk of GERD.
Avoiding Triggering Foods and Beverages:
As mentioned earlier, it is important to identify and avoid trigger foods and beverages that worsen your GERD symptoms. By eliminating or reducing these triggers, you can decrease the frequency and severity of acid reflux episodes.
Quitting Smoking:
Smoking weakens the lower esophageal sphincter and can irritate the lining of the esophagus, making it more susceptible to acid reflux. Quitting smoking can improve GERD symptoms and overall health.
GERD in Infants and Children
Symptoms:
Infants and children may also experience GERD, with symptoms including frequent spitting up, vomiting, irritability during or after feedings, difficulty gaining weight, and respiratory issues such as coughing or wheezing.
Diagnosis:
Diagnosing GERD in infants and children often involves a thorough medical history, physical examination, and in some cases, reflux testing. Your pediatrician may also assess for any underlying conditions that may contribute to your child’s symptoms.
Treatment:
Treatment options for GERD in infants and children may include lifestyle modifications, such as feeding changes and positioning techniques, medication to reduce stomach acid, and in rare cases, surgery. It is important to consult with a pediatrician to develop an appropriate treatment plan tailored to your child’s needs.
FAQs about GERD
What is the difference between GERD and acid reflux?
GERD and acid reflux are closely related, but there is a distinction between the two. Acid reflux refers to the occasional backflow of stomach acid into the esophagus, causing temporary symptoms such as heartburn. GERD, on the other hand, is a chronic condition characterized by frequent acid reflux episodes, often resulting in persistent symptoms and potential complications.
Is GERD a chronic condition?
Yes, GERD is considered a chronic condition. It is a long-term condition that requires ongoing management to control symptoms and prevent complications. With proper treatment and lifestyle changes, individuals with GERD can lead a comfortable and healthy life.
Can GERD lead to esophageal cancer?
Although the risk is relatively low, untreated GERD, especially in the presence of Barrett’s esophagus, can increase the risk of developing esophageal cancer. Regular monitoring and appropriate management of GERD symptoms are crucial to minimize this risk. It is important to consult with a healthcare provider for proper diagnosis, treatment, and follow-up care.
In conclusion, Gastroesophageal Reflux Disease (GERD) is a chronic condition characterized by the backflow of stomach acid into the esophagus, leading to various symptoms and potential complications if left untreated. Diagnosis involves a medical history, physical examination, and sometimes additional tests. Treatment options range from lifestyle changes and medications to surgical intervention. Managing GERD symptoms can be achieved through diet modifications, natural remedies, and certain lifestyle practices. By understanding the causes, symptoms, and treatment options, individuals with GERD can effectively manage their condition and improve their quality of life.