In this article, we will explore the fundamentals of Meniere’s Disease, a condition that affects the inner ear and can lead to a variety of troubling symptoms. From sudden episodes of vertigo to hearing loss and tinnitus, Meniere’s Disease can significantly impact one’s quality of life. By understanding the causes, symptoms, and available treatment options, you will gain valuable insights into managing this condition and regaining control over your health. So, let’s embark on this journey together and uncover the intricacies of Meniere’s Disease.

Overview of Meniere’s Disease
What is Meniere’s Disease?
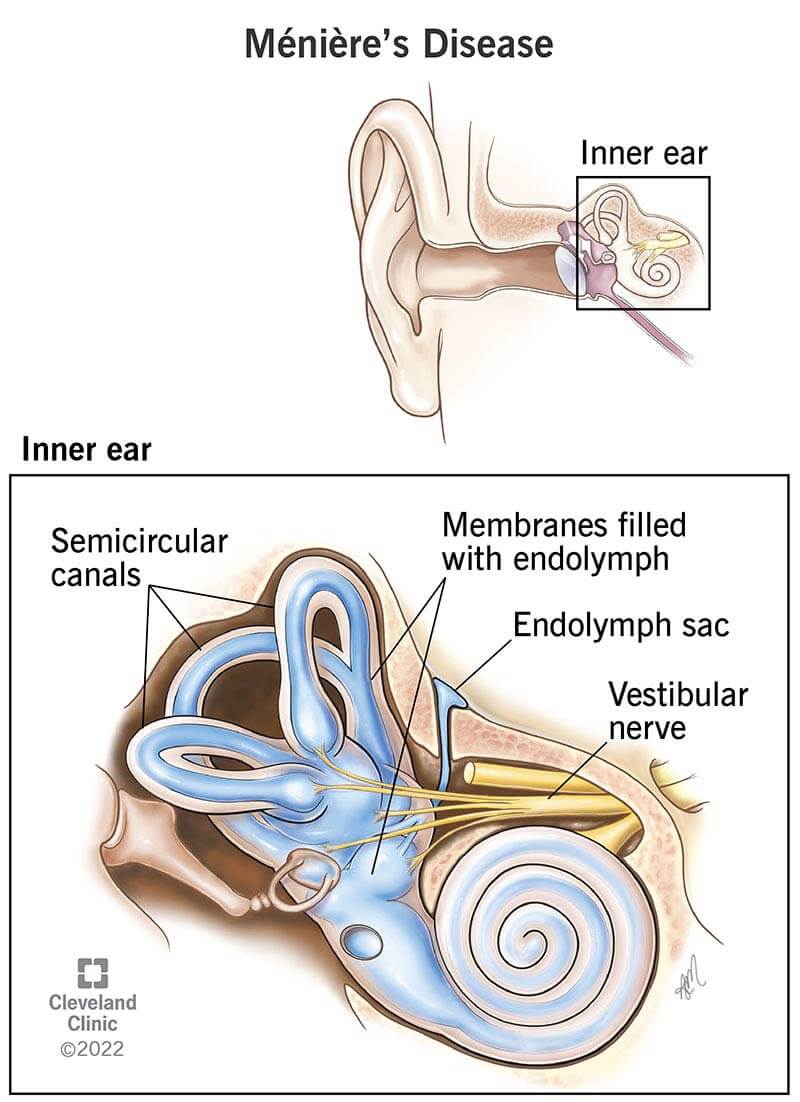
Meniere’s Disease is a chronic condition that affects the inner ear, specifically the balance and hearing mechanisms. It is characterized by a combination of symptoms such as vertigo (a spinning sensation), tinnitus (ringing in the ears), hearing loss, and a feeling of fullness in the affected ear.
Causes of Meniere’s Disease
The exact cause of Meniere’s Disease is still unknown. Researchers believe that it may be a result of a combination of factors including fluid buildup in the inner ear, abnormal immune response, genetic factors, environmental triggers, and age and gender.
Symptoms of Meniere’s Disease
The symptoms of Meniere’s Disease can vary from person to person, but the most common ones include episodes of vertigo, which can last from minutes to hours, tinnitus, hearing loss or fluctuations in hearing, and a sensation of fullness or pressure in the affected ear.
Diagnosis of Meniere’s Disease
Diagnosing Meniere’s Disease can be challenging as it is based on a combination of symptoms and ruling out other possible causes. A thorough medical history and physical examination, along with hearing tests, electronystagmography (ENG), magnetic resonance imaging (MRI), and other tests may be performed to confirm the diagnosis.
Treatment of Meniere’s Disease
While there is currently no cure for Meniere’s Disease, there are several treatment options available to manage the symptoms and improve quality of life. These include lifestyle and dietary changes, medications, physical therapy, injections and pressure treatments, and in some cases, surgery. The treatment plan is usually tailored to each individual’s specific needs and symptoms.
Understanding the Symptoms
Vertigo
One of the most prominent symptoms of Meniere’s Disease is vertigo, which is a sensation of spinning or whirling. During a vertigo episode, you may feel like the room is spinning around you or that you are spinning in space. This dizziness can be accompanied by nausea, vomiting, sweating, and a feeling of unsteadiness. Vertigo attacks can vary in frequency and duration, making it challenging to perform daily activities.
Tinnitus
Tinnitus, or ringing in the ears, is another common symptom of Meniere’s Disease. This persistent sound can vary in intensity and pitch, and it may be present in one or both ears. Tinnitus can be continuous or intermittent and may worsen during episodes of vertigo or hearing loss. It can significantly impact a person’s quality of life, causing stress, anxiety, and difficulty concentrating.
Hearing Loss
Hearing loss or fluctuations in hearing is another key symptom of Meniere’s Disease. This hearing impairment may affect one or both ears and can range from mild to severe. People with Meniere’s Disease often experience a gradual or sudden decrease in hearing, which can be accompanied by a feeling of fullness or pressure in the affected ear. The extent of hearing loss can vary from person to person and can significantly impact communication and social interactions.

Causes and Risk Factors
Fluctuating Fluid Buildup in the Inner Ear
One of the leading theories behind Meniere’s Disease is the fluctuating fluid buildup in the inner ear, also known as endolymphatic hydrops. This excess fluid disrupts the delicate balance of the inner ear, leading to the characteristic symptoms of Meniere’s Disease. The exact cause of this fluid buildup is still unknown, but it is believed to be related to abnormalities in the fluid-regulating mechanisms of the inner ear.
Abnormal Immune Response
Some researchers suggest that Meniere’s Disease may be related to abnormal immune responses. It is hypothesized that the immune system may mistakenly attack the structures of the inner ear, leading to inflammation and damage. This immune response could be triggered by infections, allergies, or autoimmune disorders.
Genetic Factors
There is evidence to suggest that genetic factors may play a role in the development of Meniere’s Disease. Studies have shown that individuals with a family history of the condition are at a higher risk of developing it themselves. However, the specific genes involved and the inheritance patterns are not yet fully understood.
Environmental Factors
Various environmental factors have been proposed as potential triggers for Meniere’s Disease. These include exposure to loud noises, head trauma, viral infections, and certain medications. While these factors may not directly cause the condition, they can contribute to the onset or exacerbation of symptoms in individuals predisposed to Meniere’s Disease.
Age and Gender
Meniere’s Disease can affect individuals of any age, but it is more common in adults aged 40 to 60. It is also observed that women are slightly more likely to develop Meniere’s Disease compared to men. Hormonal changes, such as those that occur during pregnancy or menopause, may contribute to the higher prevalence in women.
Diagnosing Meniere’s Disease
Medical History and Physical Examination
The first step in diagnosing Meniere’s Disease is a thorough medical history and physical examination. Your doctor will ask about your symptoms, their frequency and duration, any triggers or patterns, and any previous ear-related conditions or treatments. The physical examination may include checking your balance, assessing your ear canals, and examining your eardrums for any abnormalities.
Hearing Tests
Hearing tests are crucial in the diagnosis of Meniere’s Disease. Audiometry, a common hearing test, measures your ability to hear different frequencies and volumes. This test helps determine the extent of hearing loss or fluctuations in hearing. Tympanometry, another test, measures the movement of your eardrums in response to changes in air pressure, providing valuable information about the condition of your middle ear.
Electronystagmography (ENG)
Electronystagmography (ENG) is a test that measures the movements of your eyes to assess the functionality of your balance system. During the test, you may be asked to track a moving object with your eyes or to lie down and turn your head in different directions. ENG helps identify any abnormal eye movements that can indicate a problem with your inner ear.
Magnetic Resonance Imaging (MRI)
In some cases, an MRI may be recommended to rule out other possible causes of your symptoms. An MRI uses powerful magnets and radio waves to create detailed images of your inner ear and surrounding structures. This imaging test can help detect any structural abnormalities or tumors that may be responsible for your symptoms.
Other Tests
Additional tests may be performed to further evaluate your condition and rule out other potential causes. These tests may include blood tests to check for underlying medical conditions, balance function tests to assess your balance abilities, and vestibular evoked myogenic potentials (VEMP) tests to evaluate the functionality of specific inner ear muscles.
Treatment Options for Meniere’s Disease
Lifestyle and Dietary Changes
Making certain lifestyle and dietary changes can help manage the symptoms of Meniere’s Disease. It is advised to limit salt intake as excess sodium can contribute to fluid retention in the body, including the inner ear. Additionally, reducing caffeine and alcohol consumption, managing stress levels, and getting adequate rest can help minimize the frequency and severity of Meniere’s Disease episodes.
Medications
Medications are frequently prescribed to alleviate the symptoms associated with Meniere’s Disease. Medications such as diuretics may be prescribed to reduce fluid buildup in the inner ear, reducing the frequency and intensity of vertigo episodes. Anti-nausea medications and motion sickness drugs can provide relief during vertigo attacks. In some cases, medications that suppress the immune system may be prescribed to manage symptoms.
Physical Therapy
Physical therapy exercises can be helpful in managing balance problems associated with Meniere’s Disease. These exercises focus on improving strength, coordination, and stability, helping individuals regain their balance and reduce the impact of vertigo on their daily activities. A physical therapist can provide a customized exercise regimen based on your specific needs.
Injections and Pressure Treatments
In certain cases, injections of medications into the middle ear or inner ear can be beneficial for managing Meniere’s Disease symptoms. These injections, such as corticosteroids or gentamicin, aim to reduce inflammation in the inner ear or damage specific cells responsible for balance. Pressure treatments, such as endolymphatic sac decompression or labyrinthectomy, may also be considered in severe cases.
Surgery
Surgery is typically the last resort for individuals with severe and debilitating Meniere’s Disease symptoms. Surgical options may include endolymphatic sac surgery to improve fluid drainage, labyrinthectomy to remove the balance and hearing mechanisms, or vestibular nerve sectioning to sever the connection between the inner ear and brain. These surgeries aim to alleviate symptoms and improve quality of life.
Managing Symptoms and Preventing Attacks
Stress and Anxiety Management
Stress and anxiety can worsen the symptoms of Meniere’s Disease and trigger episodes. Implementing stress management techniques such as deep breathing, meditation, yoga, or engaging in hobbies can help reduce stress levels and promote overall well-being. Seeking support from loved ones and joining support groups can also provide emotional support during challenging times.
Hydration and Balanced Diet
Maintaining proper hydration and adopting a balanced diet can play a significant role in managing Meniere’s Disease symptoms. Drinking an adequate amount of water helps regulate the fluid balance in the body, including the inner ear. A diet rich in fruits, vegetables, lean proteins, and whole grains provides the necessary nutrients for overall health and well-being. Limiting the consumption of processed foods and sugary drinks can also be beneficial.
Limitation of Salt and Caffeine
Reducing salt intake is commonly recommended for individuals with Meniere’s Disease, as excessive sodium can contribute to fluid retention and worsen symptoms. Avoiding high-sodium foods such as processed meats, canned soups, and salty snacks can help manage fluid buildup in the inner ear. Similarly, reducing caffeine intake, found in coffee, tea, chocolate, and some medications, can help minimize the risk of triggering vertigo episodes.
Avoiding Triggers
Identifying and avoiding triggers that worsen Meniere’s Disease symptoms can help prevent or minimize the occurrence of attacks. Each individual may have unique triggers, but some common ones include sudden head movements, intense physical exertion, exposure to loud noises, bright or flickering lights, and certain medications. By recognizing and avoiding these triggers, you can reduce the frequency and severity of Meniere’s Disease episodes.
Regular Exercise
Regular exercise can contribute to overall well-being and help manage Meniere’s Disease symptoms. Engaging in low-impact exercises such as walking, swimming, or cycling can improve cardiovascular health and promote balance. It is important to choose exercises that do not trigger vertigo or exacerbate symptoms. Consult with a healthcare professional or physical therapist to develop an exercise routine that suits your specific needs and limitations.

Coping with Emotional and Psychological Impact
Impact on Mental Health
Living with Meniere’s Disease can have a significant emotional and psychological impact. The unpredictable nature of the condition, the impact on daily activities, and the potential for isolation can lead to feelings of frustration, anxiety, and depression. It is essential to acknowledge and address these emotional challenges. Seeking support from loved ones, joining support groups, and attending therapy can provide a safe space for expressing emotions and finding coping strategies.
Supportive Therapies and Counseling
Supportive therapies and counseling can be beneficial for individuals with Meniere’s Disease who are experiencing emotional and psychological distress. Cognitive-behavioral therapy (CBT) can help individuals develop coping mechanisms to manage stress, anxiety, and depression. Additionally, counseling can provide a supportive environment to discuss the challenges of living with Meniere’s Disease and develop strategies to improve emotional well-being.
Living with Meniere’s Disease
Adaptive Techniques
Living with Meniere’s Disease may require adopting adaptive techniques to manage the symptoms and minimize their impact on daily activities. These techniques may include using assistive devices for hearing loss, such as hearing aids or cochlear implants. Implementing changes to the home environment, such as installing handrails and adding non-slip surfaces, can enhance safety and reduce the risk of falls during vertigo episodes.
Assistive Devices
Assistive devices can aid individuals with Meniere’s Disease in managing their symptoms effectively. Devices such as vibrating alarms or signaling systems can help alert individuals during vertigo episodes or when hearing loss occurs. Additionally, devices that provide sound therapy, such as white noise machines or hearing aid accessories, can alleviate the impact of tinnitus and improve quality of sleep.
Educating Family and Friends
Educating family, friends, and coworkers about Meniere’s Disease is crucial for creating a supportive and understanding environment. Explaining the symptoms, triggers, and challenges associated with Meniere’s Disease can help others comprehend the impact it has on daily life. Encourage loved ones to attend doctor appointments or support group meetings to gain further insight and foster empathy for your condition.

Research and Advances in Meniere’s Disease
Current Studies and Research Findings
Research on Meniere’s Disease is ongoing to better understand its causes, progression, and potential treatment strategies. Current studies are focused on investigating genetic factors, immune system involvement, and the role of inflammation in the development of the disease. In addition, researchers are exploring the potential benefits of novel drug therapies and advanced surgical techniques to improve outcomes for individuals with Meniere’s Disease.
New Treatment Developments
Alongside ongoing research, new treatment developments are being explored to provide relief and improve the quality of life for individuals with Meniere’s Disease. These developments include the use of intratympanic injections of medications directly into the middle ear, the application of regenerative therapies to repair inner ear damage, and the advancement of vestibular implants to restore balance function. While these treatments are still in the experimental stage, they offer hope for future advancements in managing Meniere’s Disease.
Conclusion
Meniere’s Disease is a complex condition that can significantly impact an individual’s quality of life. While there is no cure, understanding the symptoms, causes, and various treatment options can help individuals manage their condition effectively. From lifestyle changes to therapeutic interventions, and from coping strategies to advances in research, there are resources available to support those living with Meniere’s Disease. By working closely with healthcare professionals, adapting to new techniques, and seeking support from loved ones, individuals can lead fulfilling lives despite the challenges posed by this chronic condition.