Having a healthy digestive system is essential for overall well-being. In this article, you will learn everything you need to know about GERD, or gastroesophageal reflux disease. From what it is to its causes, symptoms, and treatment options, understanding GERD will empower you to take control of your digestive health. So, let’s dive into the world of GERD and explore how it can affect your daily life.
Overview of GERD
Definition of GERD
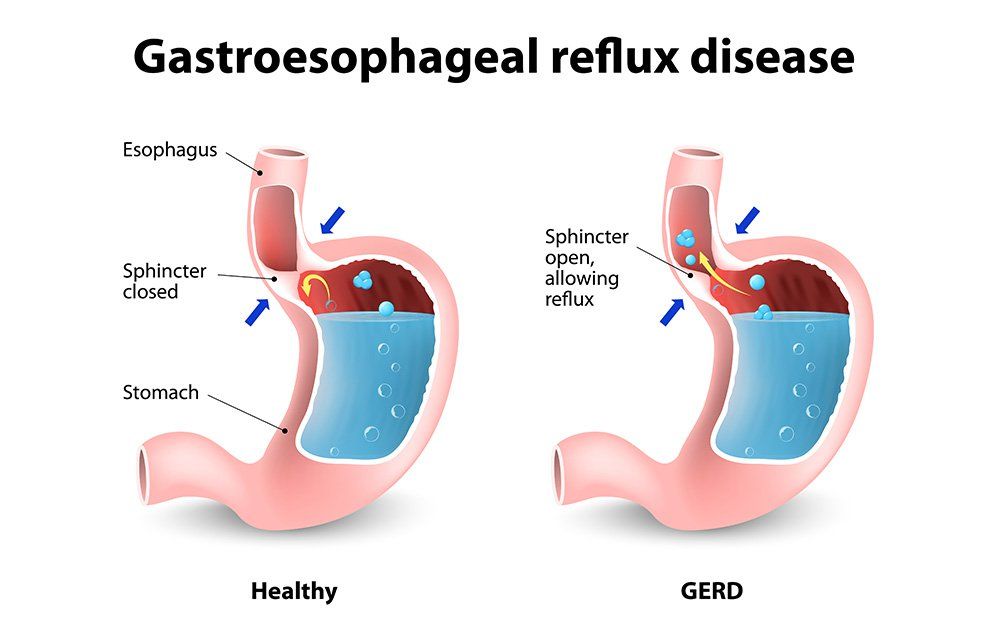
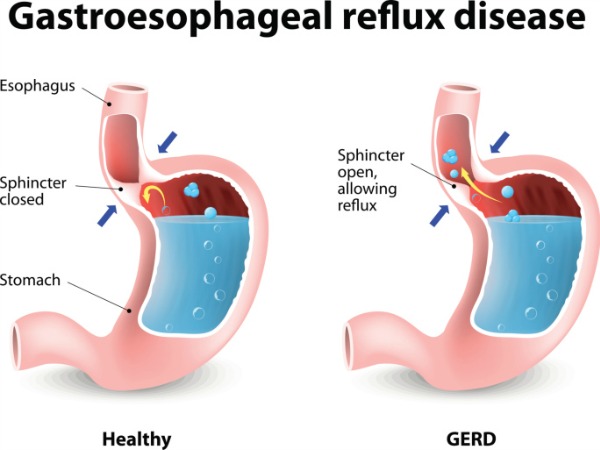
GERD, or gastroesophageal reflux disease, is a chronic digestive disorder characterized by the reflux, or backward flow, of stomach acid and other contents into the esophagus. This occurs when the lower esophageal sphincter (LES), the muscular ring that separates the stomach from the esophagus, becomes weak or relaxes inappropriately. The constant exposure of the esophagus to acid can cause irritation and inflammation, leading to various symptoms.
Prevalence of GERD
GERD is a common condition, affecting millions of people worldwide. In the United States alone, it is estimated that around 20% of the population experiences symptoms of GERD at least once a week. The prevalence of GERD tends to increase with age, with a higher incidence in individuals over the age of 40. It is also more common in men than in women.
Causes of GERD
Several factors can contribute to the development of GERD. The weakening of the lower esophageal sphincter (LES) is a primary cause, which can be due to lifestyle factors such as obesity, smoking, and consuming certain foods and beverages. Hiatal hernia, a condition in which a portion of the stomach protrudes into the chest through the diaphragm, can also increase the risk of GERD. Other factors include pregnancy, certain medications, and certain medical conditions such as scleroderma.
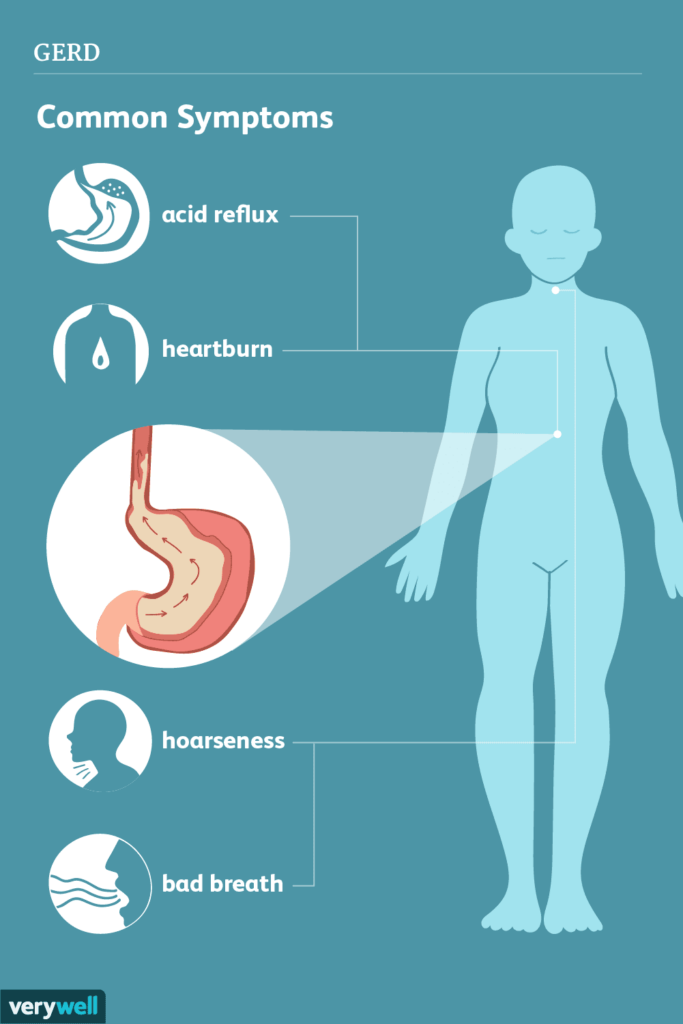
Symptoms of GERD
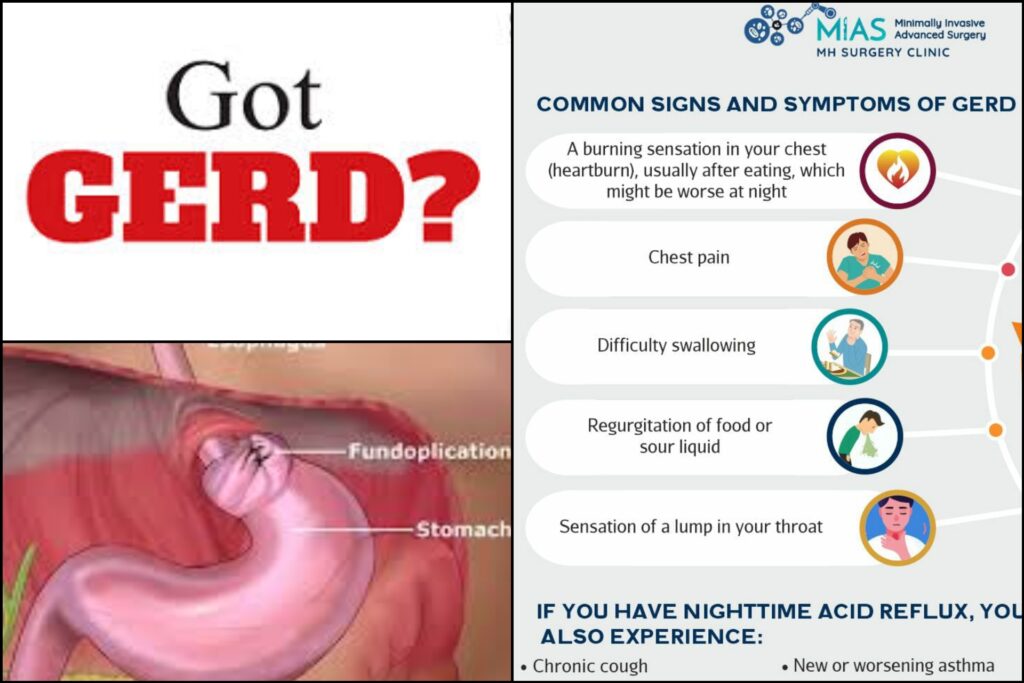
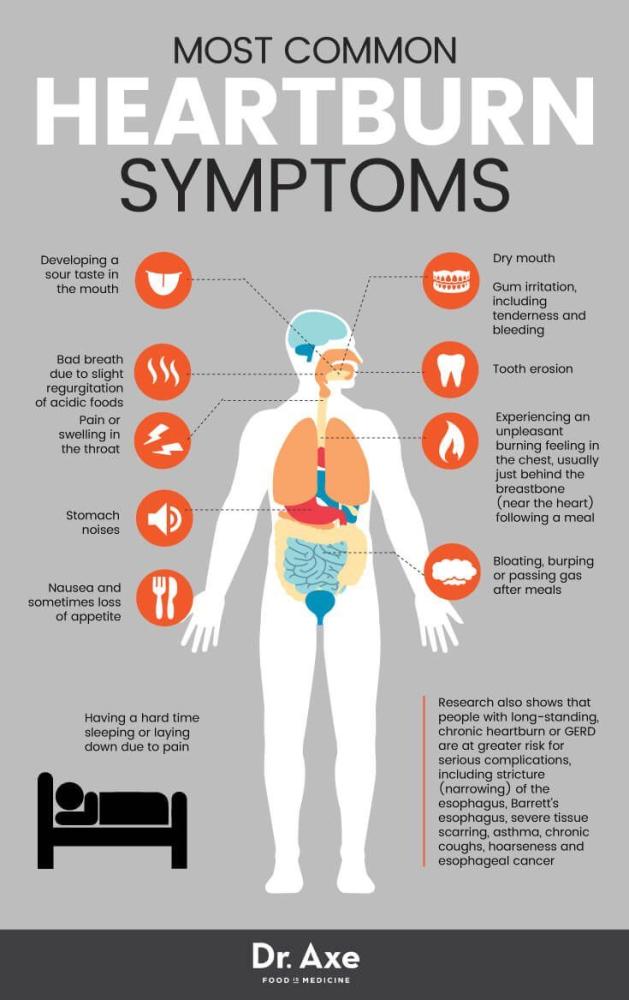
The symptoms of GERD can vary from person to person, but commonly include:
- Heartburn: a burning sensation in the chest, often after eating or when lying down.
- Acid regurgitation: the feeling of acid backing up into the throat or mouth.
- Difficulty swallowing: a sensation of food getting stuck in the throat.
- Chest pain: often mistaken for a heart attack, this pain can radiate to the back, neck, jaw, or arms.
- Chronic cough: a persistent cough, especially at night, that is not related to a respiratory infection.
- Sore throat or hoarseness: irritation of the throat due to acid reflux reaching the upper airways.
Diagnosis of GERD
Medical history and physical examination
To diagnose GERD, your healthcare provider will take a detailed medical history and perform a physical examination. They will ask about your symptoms, their frequency and severity, as well as any factors that may worsen or alleviate them. Additionally, they may inquire about your lifestyle habits, diet, and medication usage. During the physical examination, they will check for any signs of complications, such as inflammation or narrowing of the esophagus.
Upper endoscopy
An upper endoscopy, also known as an esophagogastroduodenoscopy (EGD), is a procedure that allows a healthcare provider to visually examine the lining of the esophagus, stomach, and duodenum using a flexible, lighted tube called an endoscope. This procedure is typically performed under sedation. Upper endoscopy can help identify any inflammation, abnormal tissue growth, or strictures in the esophagus, as well as assess the integrity of the LES and the presence of a hiatal hernia.
Esophageal pH monitoring
Esophageal pH monitoring is a test that measures the amount of acid in the esophagus over a 24-hour period. A thin, flexible tube with a pH sensor is inserted through the nose and positioned in the lower esophagus. The sensor detects changes in acidity and records them on a small device worn on a belt. This test is crucial in confirming the diagnosis of GERD, as it provides objective evidence of acid reflux.
Barium swallow test
A barium swallow test, also known as an upper GI series, involves drinking a chalky liquid containing barium, a contrast material that can be visualized on X-rays. As the barium flows down the esophagus, X-ray images are taken to evaluate its movement and identify any abnormalities. This test can help detect strictures, hiatal hernias, and other structural issues that may contribute to GERD.
Esophageal manometry
Esophageal manometry is a procedure that measures the strength and coordination of the muscles in the esophagus. A thin, flexible tube with pressure sensors is passed through the nose or mouth and into the esophagus. The sensors detect the contractions of the esophageal muscles as you swallow. This test helps determine if the muscles are functioning properly and can aid in diagnosing conditions such as achalasia, which can mimic GERD symptoms.
Treatment options for GERD
Lifestyle changes
Lifestyle modifications are often the first line of treatment for mild to moderate cases of GERD. These may include:
- Weight loss: Losing excess weight can reduce pressure on the stomach and improve symptoms.
- Elevating the head of the bed: Raising the head of the bed by 6 to 8 inches can prevent stomach acid from flowing back into the esophagus during sleep.
- Avoiding trigger foods: Certain foods and beverages, such as spicy foods, citrus fruits, caffeine, and alcohol, can trigger symptoms. Identifying and avoiding these triggers can help manage GERD.
- Eating smaller meals: Consuming smaller, more frequent meals can prevent overloading the stomach and minimize acid reflux.
- Quitting smoking: Smoking weakens the LES and can worsen GERD symptoms. Quitting smoking can improve symptoms and overall health.
Medications
Medications may be recommended to control symptoms and reduce the production of stomach acid. Commonly prescribed medications for GERD include:
- Proton pump inhibitors (PPIs): These medications, such as omeprazole and pantoprazole, reduce stomach acid production and promote healing of the esophagus.
- H2 blockers: H2 blockers, such as ranitidine and famotidine, decrease the amount of acid produced by the stomach.
- Antacids: Over-the-counter antacids, like Tums and Rolaids, provide temporary relief by neutralizing stomach acid.
It is important to consult with a healthcare provider before starting any medication, as they can assess your specific condition and recommend the most appropriate treatment.
Surgical interventions
If lifestyle changes and medications do not provide sufficient relief, surgical interventions may be considered. The most common surgical procedure for GERD is laparoscopic fundoplication, where the upper part of the stomach is wrapped around the LES to strengthen it and prevent acid reflux. Surgical interventions are typically reserved for severe cases of GERD or when other treatment options have been unsuccessful.
Complications of untreated GERD
Esophagitis
Untreated GERD can lead to esophagitis, which is inflammation of the esophagus. Continuous exposure to stomach acid irritates the lining of the esophagus, causing redness, swelling, and sometimes ulceration. Esophagitis can result in pain, difficulty swallowing, and bleeding.
Esophageal strictures
Repeated episodes of acid reflux can cause the esophagus to narrow, forming strictures. These narrowed areas can make swallowing difficult and painful. Severe strictures may require dilation through an endoscopic procedure to improve swallowing function.
Barrett’s esophagus
Barrett’s esophagus is a condition in which the normal cells lining the esophagus are replaced with abnormal cells resembling those found in the intestine. It is considered a precancerous condition, as it significantly increases the risk of developing esophageal adenocarcinoma, a type of cancer.
Esophageal cancer
Long-standing GERD, especially when left untreated, can increase the risk of developing esophageal cancer. Esophageal adenocarcinoma, as mentioned above, is one type of cancer that can arise as a result of chronic acid reflux.
Diet and GERD
Avoiding trigger foods
Certain foods and beverages can trigger or exacerbate GERD symptoms. It is important to identify and avoid these trigger foods, which may vary from person to person. Common trigger foods include:
- Citrus fruits and juices: Oranges, grapefruits, and other citrus fruits can increase acid production and worsen reflux symptoms.
- Tomatoes and tomato-based products: The high acidity of tomatoes can irritate the esophagus and trigger symptoms.
- Chocolate and mint: These can relax the lower esophageal sphincter (LES) and increase the risk of acid reflux.
- Fried and fatty foods: These can slow down digestion, leading to increased acid production and greater risk of reflux.
Eating smaller meals
Consuming large meals can lead to increased stomach pressure, which can force stomach contents into the esophagus. Eating smaller, more frequent meals can help prevent excessive pressure on the LES and minimize acid reflux.
Elevating the head of the bed
Raising the head of the bed by 6 to 8 inches can prevent stomach acid from flowing back into the esophagus during sleep. This can be achieved by using bed risers or placing a wedge-shaped pillow under the upper body.
Limiting alcohol and caffeine
Alcohol and caffeine can relax the LES and stimulate stomach acid production, making reflux more likely. It is advisable to limit or avoid these beverages, especially close to bedtime, to help manage GERD symptoms.
Foods to avoid with GERD
Citrus fruits and juices
As mentioned earlier, citrus fruits and juices can increase acid production and worsen reflux symptoms. Oranges, grapefruits, lemons, and limes should be avoided or consumed in moderation by individuals with GERD.
Tomatoes and tomato-based products
Tomatoes are highly acidic and can irritate the esophagus. This includes fresh tomatoes, tomato sauces, pastes, and ketchup. It is advisable to choose alternative sauces and toppings for dishes to minimize acid reflux.
Chocolate and mint
Chocolate and mint can relax the lower esophageal sphincter (LES), allowing stomach acid to flow back into the esophagus. Individuals with GERD should be cautious with chocolate desserts, mint-flavored candies, and mint teas.
Fried and fatty foods
Fried and fatty foods are more difficult to digest, leading to increased acid production and higher risk of acid reflux. It is recommended to avoid fried foods, fatty cuts of meat, rich desserts, and high-fat dairy products.
Managing GERD during pregnancy
Hormonal changes and GERD
Pregnancy hormones, such as progesterone, can relax the muscles, including the LES, contributing to acid reflux. The growing uterus can also push the stomach upward, further increasing the risk of GERD during pregnancy.
Safe medications during pregnancy
Not all medications used to treat GERD are safe during pregnancy. It is essential to consult with a healthcare provider before taking any medication to ensure its safety for both the mother and the baby. Antacids containing calcium carbonate or magnesium hydroxide are generally considered safe and can provide temporary relief from heartburn. H2 blockers may also be prescribed, but proton pump inhibitors (PPIs) should be used with caution and only when the benefits outweigh the risks.
Dietary modifications for pregnant women
Pregnant women with GERD can make dietary modifications to manage their symptoms. This includes eating smaller, more frequent meals, avoiding trigger foods, and refraining from lying down immediately after eating. Elevating the head of the bed and wearing loose-fitting clothing can also help reduce reflux episodes.
GERD in infants and children
Causes of GERD in infants and children
GERD in infants and children can be caused by several factors, including:
- Immature lower esophageal sphincter (LES): The LES may not function properly in infants, allowing stomach contents to reflux back into the esophagus.
- Hiatal hernia: Infants and children with hiatal hernia may be more prone to GERD as the stomach can herniate through the diaphragm, causing reflux.
- Obesity: Excess weight can increase pressure on the stomach and trigger reflux in children.
Diagnosing GERD in infants and children
Diagnosing GERD in infants and children can be challenging due to their limited ability to communicate their symptoms. Healthcare providers may rely on the following indicators to make a diagnosis:
- Frequent vomiting or regurgitation
- Poor weight gain or failure to thrive
- Recurrent respiratory symptoms, such as coughing, wheezing, or recurrent pneumonia
- Irritability during or after feeding
- Refusal to eat or difficulty swallowing
In some cases, additional diagnostic tests, such as an upper GI series or esophageal pH monitoring, may be recommended to confirm the diagnosis.
Treatment options for pediatric GERD
The treatment of GERD in infants and children is typically focused on lifestyle modifications and medication if necessary. Lifestyle changes may include adjusting feeding habits, such as smaller, more frequent meals, burping during feedings, and maintaining an upright position after meals. Medications, such as proton pump inhibitors or H2 blockers, may be prescribed for more severe cases or when lifestyle modifications are insufficient. Regular monitoring and follow-up with a pediatrician are crucial to ensure appropriate management of pediatric GERD.
GERD and obesity
Link between obesity and GERD
There is a strong association between obesity and GERD. Excess weight, particularly around the abdomen, increases the pressure on the stomach, promoting reflux of stomach acid into the esophagus. Obesity can also contribute to the weakening of the lower esophageal sphincter (LES), allowing acid to flow backward more easily. Studies have shown that weight loss can significantly improve GERD symptoms and reduce the need for medication.
Weight loss strategies for managing GERD
Losing weight can be an effective strategy in managing GERD symptoms for individuals who are overweight or obese. Here are some weight loss strategies that can help:
- Balanced diet: Following a healthy, balanced diet that is low in fat, high in fiber, and includes a variety of fruits, vegetables, whole grains, and lean proteins can support weight loss.
- Regular exercise: Engaging in regular physical activity, such as walking, jogging, or swimming, can aid in weight loss and improve overall health.
- Portion control: Practicing portion control and mindful eating can help prevent overeating and promote weight loss.
It is important to consult with a healthcare provider or a registered dietitian before starting any weight loss program to ensure it is safe and tailored to individual needs.
Natural remedies and alternative treatments for GERD
Herbal supplements
Certain herbal supplements are believed to have beneficial effects on GERD symptoms. These include:
- Ginger: Ginger has anti-inflammatory properties and can help soothe the digestive system. Consuming ginger tea or adding fresh ginger to meals may provide relief from GERD symptoms.
- Licorice: Deglycyrrhizinated licorice (DGL) is a form of licorice that has been processed to remove a compound that can raise blood pressure. DGL may help reduce inflammation and protect the esophageal lining.
It is important to note that herbal supplements can interact with medications or have side effects, so it is advisable to consult with a healthcare provider before incorporating them into a treatment plan.
Acupuncture
Acupuncture is an alternative treatment that involves the insertion of thin needles into specific points on the body. It is believed to help restore the balance of energy in the body and may provide relief from GERD symptoms for some individuals. However, more research is needed to fully understand the effectiveness of acupuncture for GERD.
Probiotics
Probiotics are beneficial bacteria that can support a healthy digestive system. Some studies suggest that certain strains of probiotics may help reduce GERD symptoms by improving gut health. Probiotics can be found in yogurt, fermented foods, and dietary supplements. However, more research is needed to determine the specific strains and dosages that are effective for GERD.
Relaxation techniques
Stress and anxiety can worsen GERD symptoms. Engaging in relaxation techniques such as deep breathing exercises, meditation, or yoga can help reduce stress and promote overall well-being. These techniques may indirectly alleviate GERD symptoms by reducing anxiety levels and improving digestion.
While natural remedies and alternative treatments can be explored in conjunction with conventional medical treatment, it is essential to consult with a healthcare provider before trying any new approach to ensure it is safe and suitable for individual circumstances.
In conclusion, GERD is a common digestive disorder characterized by the reflux of stomach acid into the esophagus. Diagnosis usually involves a combination of medical history, physical examination, and diagnostic tests. Treatment options range from lifestyle modifications to medications and surgical interventions. Untreated GERD can lead to complications such as esophagitis, strictures, Barrett’s esophagus, and even esophageal cancer. Diet plays a crucial role in managing GERD, with trigger foods like citrus fruits, tomatoes, chocolate, and fatty foods best avoided. Specific considerations need to be made for managing GERD during pregnancy, in infants and children, and in individuals who are obese. Natural remedies and alternative treatments, such as herbal supplements, acupuncture, probiotics, and relaxation techniques, can also be explored to complement conventional treatment under the guidance of a healthcare professional. By understanding GERD and its various aspects, individuals can take steps to manage the condition effectively and improve their quality of life.