Did you know that depression and sleep disorders are closely interconnected? In this article, we will explore the fascinating link between these two conditions and how they can impact each other. Depression can often lead to various sleep disturbances, such as insomnia or oversleeping, while sleep disorders can contribute to the development or worsening of depressive symptoms. Understanding this complex relationship can help pave the way for more effective treatment strategies and improved overall mental well-being. So, let’s delve into the intricate connection between depression and sleep disorders and shed light on how they affect one another.

Understanding Depression
Depression is a common mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities. It affects people of all ages, genders, and backgrounds. It is important to note that depression is not simply feeling “down” or having a bad day; rather, it is a serious medical condition that can significantly impact a person’s daily life.
What is depression?
Depression is more than just a transient mood or emotional state. It is a complex disorder with a range of symptoms that can vary from mild to severe. Some common symptoms of depression include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in previously enjoyable activities
- Changes in appetite and weight (either increased or decreased)
- Sleep disturbances (insomnia, oversleeping, or restless sleep)
- Fatigue or loss of energy
- Difficulty concentrating, making decisions, or remembering things
- Feelings of guilt, worthlessness, or helplessness
- Recurring thoughts of death or suicide
Depression can have a profound impact on a person’s overall well-being, relationships, and ability to function in daily life.
Types of depression
There are several different types of depression, each with its own unique set of symptoms and characteristics. Some common forms of depression include:
- Major depressive disorder (MDD): This is the most common form of depression, characterized by persistent feelings of sadness, loss of interest, and a range of other symptoms.
- Persistent depressive disorder (PDD): PDD is a chronic form of depression that lasts for two years or longer. It may have fewer symptoms but can still significantly affect daily functioning.
- Bipolar disorder: Also known as manic-depressive disorder, bipolar disorder involves periods of intense highs (mania) followed by episodes of depressive symptoms.
- Seasonal affective disorder (SAD): SAD is a type of depression that occurs during specific seasons, typically the winter months when there is less natural sunlight.
These are just a few examples of the different types of depression that exist. It is important to remember that depression is a complex and multifaceted disorder that can present differently in each individual.
Prevalence of depression
Depression is a widespread concern that affects millions of people worldwide. According to the World Health Organization (WHO), more than 264 million people of all ages suffer from depression globally. In the United States alone, approximately 17.3 million adults (7.1% of the population) have experienced at least one major depressive episode.
It is important to note that depression does not discriminate and can affect individuals of all ages, genders, and backgrounds. The causes of depression are complex and may involve a combination of genetic, biological, environmental, and psychological factors. Seeking help and support is crucial for those experiencing depression, as there are effective treatment options available.
Exploring Sleep Disorders
Sleep disorders are conditions that interfere with a person’s ability to get sufficient, restful sleep. They can result in various negative consequences, including daytime fatigue, mood disturbances, and impaired cognitive function. Understanding the different types of sleep disorders and their causes is essential for identifying and treating these conditions effectively.
Types of sleep disorders
There are numerous different types of sleep disorders, each with its own set of symptoms and characteristics. Some common sleep disorders include:
- Insomnia: Insomnia is the inability to fall asleep or stay asleep, leading to difficulty getting enough restful sleep.
- Sleep apnea: Sleep apnea is a disorder in which a person’s breathing repeatedly stops and starts during sleep. This can cause snoring, gasping for air, and disrupted sleep patterns.
- Narcolepsy: Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness and sudden attacks of sleep.
- Restless legs syndrome (RLS): RLS is a neurological condition that causes an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations. This can disrupt sleep and cause insomnia.
- REM sleep behavior disorder (RBD): RBD is a parasomnia that causes a person to act out their dreams while still asleep. This can result in violent movements and potentially harm the person or their sleep partner.
These are just a few examples of the wide range of sleep disorders that exist. It is important to consult a healthcare professional for a proper diagnosis and treatment plan if experiencing any signs or symptoms of a sleep disorder.
Causes of sleep disorders
Sleep disorders can have various underlying causes, including:
- Medical conditions: Certain medical conditions, such as chronic pain, respiratory disorders, and neurological disorders, can contribute to the development of sleep disorders.
- Medications: Some medications, such as certain antidepressants or stimulants, can interfere with sleep and contribute to the development of sleep disorders.
- Lifestyle factors: Poor sleep hygiene, irregular sleep schedules, excessive caffeine or alcohol consumption, and high levels of stress can all contribute to the development of sleep disorders.
- Psychological factors: Mental health conditions, such as anxiety and depression, can disrupt sleep patterns and contribute to the development of sleep disorders.
It is essential to identify and address the underlying causes of sleep disorders for effective management and treatment.
Effects of sleep disorders
Sleep disorders can significantly impact a person’s physical and mental well-being. Some common effects of sleep disorders include:
- Daytime fatigue: Sleep disorders can result in persistent daytime fatigue, making it difficult to stay awake and alert during the day.
- Mood disturbances: Lack of quality sleep can contribute to mood swings, irritability, and increased risk of developing mental health disorders such as depression and anxiety.
- Impaired cognitive function: Sleep disorders can lead to difficulties with concentration, memory, problem-solving, and overall cognitive performance.
- Reduced quality of life: The chronic fatigue and other symptoms associated with sleep disorders can negatively impact a person’s overall quality of life, interfering with work, relationships, and daily activities.
Recognizing the effects of sleep disorders is crucial for seeking appropriate treatment and improving overall well-being.
The Relationship Between Depression and Sleep Disorders
Depression and sleep disorders often go hand in hand, with each condition influencing and exacerbating the other. Understanding the correlation between depression and sleep disorders is essential for effective diagnosis and treatment.
Correlation between depression and sleep disorders
Research has consistently shown a strong correlation between depression and sleep disorders. Studies have found that individuals with depression are much more likely to experience sleep disturbances, such as insomnia or hypersomnia, compared to those without depression. Furthermore, individuals with sleep disorders, such as sleep apnea or insomnia, are at a higher risk of developing depression.
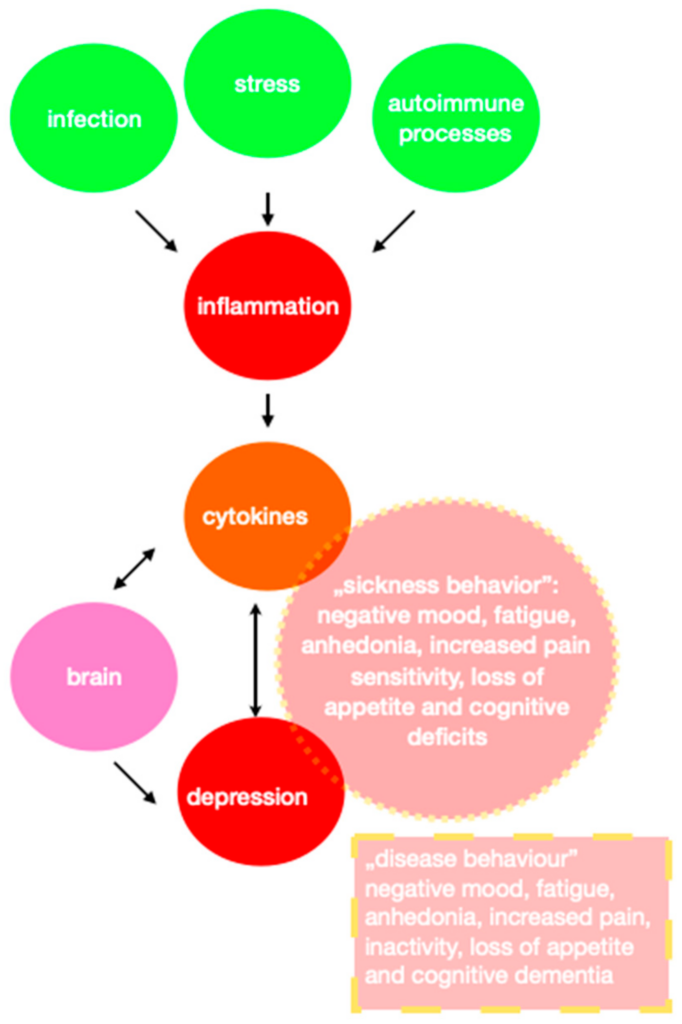
Impact of sleep disorders on depression
Sleep disorders can significantly impact the development and severity of depressive symptoms. Chronic sleep deprivation or poor sleep quality can contribute to and exacerbate feelings of sadness, hopelessness, and irritability. Lack of quality sleep can also interfere with the brain’s ability to regulate emotions, making it more difficult for individuals with depression to manage their symptoms effectively. Sleep disorders can also reduce the effectiveness of treatment for depression, making it important to address and manage sleep disturbances alongside depression.
Impact of depression on sleep disorders
Depression can also negatively impact sleep patterns and contribute to the development or exacerbation of sleep disorders. Depressive symptoms, such as persistent sadness, racing thoughts, and anxiety, can interfere with the ability to fall asleep or stay asleep. Additionally, individuals with depression may experience changes in sleep architecture, such as reduced REM sleep or disruptions in sleep stages. These sleep disturbances can further contribute to the development of sleep disorders and worsen existing sleep problems.
Understanding the bidirectional relationship between depression and sleep disorders is crucial for effective treatment and management of both conditions.
Common Symptoms of Depression and Sleep Disorders
Recognizing the common symptoms of depression and sleep disorders is essential for early detection and intervention.
Depressive symptoms
Common symptoms of depression include:
- Persistent feelings of sadness, emptiness, or hopelessness
- Loss of interest or pleasure in previously enjoyable activities
- Changes in appetite and significant weight loss or gain
- Sleep disturbances, such as insomnia or hypersomnia
- Fatigue, lack of energy, or decreased motivation
- Difficulty concentrating, making decisions, or remembering things
- Feelings of guilt, worthlessness, or excessive self-blame
- Recurring thoughts of death or suicide
It is important to note that not everyone with depression will experience all these symptoms, and symptoms can vary in severity.
Sleep disorder symptoms
Common symptoms of sleep disorders include:
- Difficulty falling asleep or staying asleep (insomnia)
- Excessive daytime sleepiness or fatigue
- Restless legs or an uncontrollable urge to move legs (RLS)
- Loud snoring, gasping for air, or breathing pauses during sleep (sleep apnea)
- Sudden episodes of falling asleep during the day (narcolepsy)
- Acting out dreams or violent movements during sleep (RBD)
These are just a few examples of the common symptoms of sleep disorders. It is important to consult a healthcare professional if experiencing any persistent sleep disturbances.

Sleep Disorders as a Risk Factor for Depression
Sleep disorders can serve as a significant risk factor for the development of depression. Understanding the long-term effects of sleep disorders on mental health is crucial for early intervention and prevention.
Long-term effects of sleep disorders on mental health
Persistent sleep disturbances, such as insomnia or sleep apnea, can have detrimental effects on mental health. Chronic sleep deprivation can significantly increase the risk of developing mental health disorders, including depression and anxiety. Lack of quality sleep can affect the brain’s ability to regulate emotions and process information, leading to mood disturbances and cognitive impairments. Therefore, addressing and managing sleep disorders is crucial for maintaining optimal mental health.
Sleep disorders and the development of depression
Research has consistently shown a strong link between sleep disorders and the development of depression. In individuals with sleep disorders, the chronic fatigue and daytime sleepiness can contribute to the development of depressive symptoms. Additionally, individuals with untreated sleep disorders may experience reduced quality of life, impaired cognitive function, and increased stress, all of which can increase the risk of developing depression. Early detection and treatment of sleep disorders are vital for preventing the onset of depression.
Understanding the intricate relationship between sleep disorders and depression is essential for effective prevention and treatment strategies.
Depression as a Risk Factor for Sleep Disorders
Depression can also serve as a significant risk factor for the development of sleep disorders. Understanding how depression affects sleep quality and contributes to sleep-related disturbances is crucial for comprehensive treatment.
How depression affects sleep quality
Depression can significantly disrupt sleep patterns and quality. Common ways in which depression affects sleep include:
- Insomnia: Many individuals with depression experience difficulty falling asleep or staying asleep, leading to insomnia.
- Hypersomnia: On the other hand, depression can also cause excessive sleepiness or prolonged sleep duration, known as hypersomnia.
- Fragmented sleep: Individuals with depression may experience fragmented or restless sleep, waking up frequently throughout the night and feeling unrefreshed in the morning.
- Nightmares: Depression can increase the likelihood of experiencing distressing nightmares, further disrupting sleep quality.
These sleep disturbances can worsen depressive symptoms and lead to a vicious cycle of poor sleep and worsening mental health.
Depression-related sleep disorders
Depression can contribute to the development of specific sleep disorders, such as:
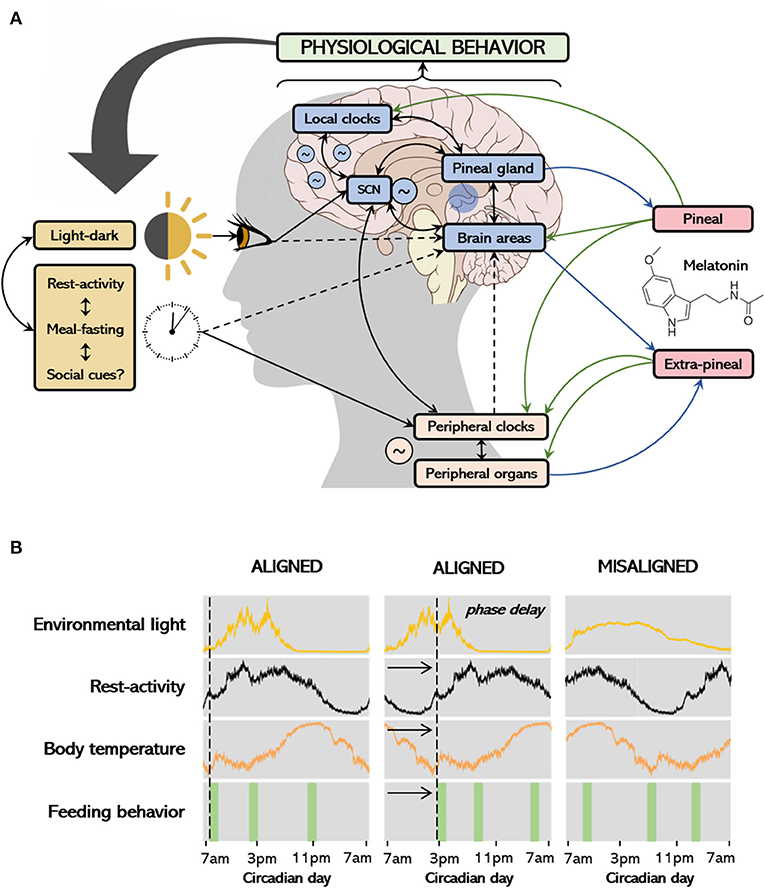
- Circadian rhythm disorders: Depression can disrupt the body’s internal clock, leading to difficulties regulating sleep-wake cycles.
- REM sleep behavior disorder (RBD): Depressive symptoms can increase the risk of developing RBD, a condition in which individuals act out their dreams while asleep.
- Sleep-related anxiety: Individuals with depression may experience increased anxiety surrounding sleep, leading to heightened arousal and difficulty falling or staying asleep.
Recognizing the impact of depression on sleep quality is crucial for comprehensive treatment and addressing the underlying causes of sleep disturbances.
Diagnosing and Treating Depression and Sleep Disorders
Proper diagnosis and treatment are essential for effectively managing depression and sleep disorders. Understanding the diagnostic criteria and available treatment options can aid in developing a personalized treatment plan.
Diagnostic criteria for depression
Depression is typically diagnosed using the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Some key criteria for diagnosing depression include:
- Presence of a depressive episode lasting at least two weeks.
- Five or more depressive symptoms present, including persistent feelings of sadness or emptiness, loss of interest or pleasure, changes in appetite or weight, sleep disturbances, fatigue, difficulty concentrating, feelings of guilt or worthlessness, and recurring thoughts of death or suicide.
- Symptoms significantly impair daily functioning and cause distress.
It is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
Diagnostic criteria for sleep disorders
Sleep disorders are diagnosed based on a thorough evaluation of an individual’s sleep patterns, symptoms, medical history, and potentially through sleep studies or other assessments. Diagnostic criteria for specific sleep disorders vary, but they often include chronic sleep disturbances that interfere with daily functioning and cause distress. Consulting a sleep specialist can help determine an accurate diagnosis and guide appropriate treatment.
Treatment options for co-occurring depression and sleep disorders
The treatment of co-occurring depression and sleep disorders typically involves addressing both conditions simultaneously. Treatment options may include:
- Psychotherapy: Cognitive-behavioral therapy (CBT) is an effective approach for treating both depression and sleep disorders. It focuses on identifying and modifying negative thoughts, behaviors, and patterns that contribute to both conditions.
- Medication: Antidepressant medications may be prescribed to help manage depressive symptoms. Sleep aids or sedatives may also be used for short-term relief of sleep disturbances.
- Lifestyle modifications: Adopting healthy sleep habits, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, avoiding stimulants like caffeine close to bedtime, and creating a comfortable sleep environment, can significantly improve sleep quality and overall well-being.
- Stress reduction techniques: Incorporating stress-reduction techniques like mindfulness meditation, deep breathing exercises, and relaxation techniques can help manage both depression and sleep disturbances.
A comprehensive treatment plan tailored to the individual’s needs, preferences, and severity of symptoms is crucial for long-term success.
Cognitive-Behavioral Therapy for Depression and Sleep Disorders
Cognitive-behavioral therapy (CBT) is a widely recognized and effective approach for treating both depression and sleep disorders. Understanding how CBT can address these conditions is essential for considering this treatment option.
Overview of cognitive-behavioral therapy
CBT is a goal-oriented, evidence-based therapy that focuses on identifying and modifying negative thoughts, beliefs, and behaviors that contribute to mental health disorders. It aims to help individuals develop healthier coping strategies, improve problem-solving skills, and change patterns of thinking and behavior that perpetuate symptoms.
CBT for depression
CBT for depression typically involves:
- Identifying and challenging negative thoughts and beliefs that contribute to depressive symptoms.
- Learning and implementing healthy coping strategies and problem-solving skills.
- Setting realistic goals and developing an action plan to achieve them.
- Addressing underlying emotional and interpersonal issues that contribute to depression.
- Establishing a routine and engaging in pleasurable activities to promote positive mood.
CBT for depression can help individuals develop more adaptive ways of thinking and behaving, leading to improved mood and overall well-being.
CBT for sleep disorders
CBT is also highly effective for treating sleep disorders. CBT for sleep disorders often includes:
- Sleep hygiene education: Learning and implementing healthy sleep habits, such as maintaining a consistent sleep schedule, creating a sleep-friendly environment, and avoiding stimulating activities before bed.
- Stimulus control: Restricting the bed and bedroom to sleep-related activities only, associating the bed with relaxation and sleep, and eliminating factors that interfere with sleep (e.g., electronic devices).
- Sleep restriction: Gradually limiting time spent in bed to increase sleep efficiency and consolidate sleep.
- Relaxation techniques: Learning and practicing relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or guided imagery, to promote relaxation and improve sleep quality.
- Cognitive restructuring: Identifying and challenging negative thoughts and beliefs about sleep, reducing bedtime anxiety, and developing more positive and realistic expectations about sleep.
CBT for sleep disorders helps individuals develop healthier sleep habits, address negative thoughts or behaviors associated with sleep, and improve overall sleep quality.
Effectiveness of CBT in addressing both depression and sleep disorders
Numerous studies have demonstrated the efficacy of CBT in addressing both depression and sleep disorders. CBT has been shown to reduce depressive symptoms, improve sleep quality, and enhance overall well-being. By simultaneously targeting the underlying factors contributing to both conditions, CBT can provide individuals with the tools they need to effectively manage and overcome depression and sleep disturbances.

Medication Options for Depression and Sleep Disorders
Medication can play a significant role in the treatment of depression and sleep disorders. Understanding the different medication options available is essential for considering appropriate treatment approaches.
Antidepressant medications
Antidepressants are commonly prescribed medications for the treatment of depression. They work by balancing brain chemicals involved in mood regulation. There are several different classes of antidepressants, including selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs). The choice of antidepressant will depend on individual factors such as symptom severity, medical history, and potential side effects. It is important to consult a healthcare professional for a proper evaluation and prescription.
Sleep aids and sedatives
Sleep aids and sedatives are medications that can help promote sleep and manage sleep disturbances. They may be prescribed on a short-term basis to address acute sleep issues or as part of a comprehensive treatment plan for sleep disorders. These medications typically include benzodiazepines, non-benzodiazepine sedatives, or melatonin agonists. It is essential to consult a healthcare professional for appropriate guidance and monitoring when considering sleep aids or sedatives.
Medication should always be used in conjunction with other treatment approaches, such as therapy and lifestyle modifications, for optimal results. Regular monitoring and open communication with a healthcare professional are essential for adjusting medication dosages or addressing any potential side effects.
Lifestyle Changes to Improve Depression and Sleep Disorders
In addition to therapy and medication, implementing certain lifestyle changes can significantly improve symptoms of depression and sleep disorders. These modifications focus on promoting overall well-being and creating a healthy foundation for improved mental health.
Establishing a consistent sleep schedule
Maintaining a consistent sleep schedule can positively impact sleep quality and overall well-being. Going to bed and waking up at the same time every day, even on weekends, helps regulate the body’s internal clock and promotes better sleep. It is important to create a relaxing bedtime routine and avoid stimulating activities, such as using electronic devices, close to bedtime. Creating a sleep-friendly environment, with a comfortable mattress, blackout curtains, and a quiet atmosphere, can also contribute to better sleep.
Exercising regularly
Regular physical exercise has been shown to have numerous benefits for mental health, including reducing symptoms of depression and improving sleep quality. Engaging in aerobic exercise, such as brisk walking, jogging, or cycling, for at least 30 minutes most days of the week can help regulate mood and promote better sleep. However, it is essential to consult a healthcare professional before starting a new exercise regimen, particularly if experiencing severe depression or physical limitations.
Implementing stress-reduction techniques
Stress can significantly impact both depression and sleep patterns. Implementing stress-reduction techniques can help promote better mental health and overall well-being. Some effective stress-reducing techniques include:
- Mindfulness meditation: Focusing on the present moment and accepting it without judgment can help reduce stress and foster calmness.
- Deep breathing exercises: Deep, slow breaths can activate the body’s relaxation response and reduce stress and anxiety.
- Relaxation techniques: Progressive muscle relaxation, guided imagery, or listening to calming music can help relax the body and mind, promoting better sleep and reducing depressive symptoms.
- Journaling or expressive writing: Writing down thoughts, emotions, and concerns can help release stress and provide clarity. It can also serve as a tool for reflection and self-discovery.
Implementing these lifestyle changes alongside therapy and medication can create a holistic approach to managing depression and sleep disorders.
In conclusion, understanding the complex relationship between depression and sleep disorders is crucial for effective diagnosis and treatment. Depression and sleep disorders often co-occur, with each condition influencing and exacerbating the other. Recognizing the common symptoms, risk factors, and treatment options for both conditions can help individuals seek appropriate care and improve their overall well-being. Whether through therapy, medication, lifestyle modifications, or a combination of approaches, addressing both depression and sleep disorders is essential for achieving optimal mental health and quality of life.