In this article, you will discover the fascinating connection between HIV and Kaposi’s Sarcoma, a rare form of cancer that primarily affects individuals with weakened immune systems. Through an exploration of the link between these two medical conditions, we will shed light on the intricate relationship between HIV infection and the development of Kaposi’s Sarcoma. Join us on this journey as we unravel the complexities and implications of this significant association.
Overview of Kaposi’s Sarcoma
Definition and Background
Kaposi’s sarcoma is a rare type of cancer that primarily affects the skin, but can also involve other organs such as the lungs, gastrointestinal tract, and lymph nodes. It is characterized by the development of abnormal blood vessels and the growth of tumors. This condition was first described by a dermatologist named Moritz Kaposi in 1872, and since then, significant progress has been made in understanding its causes, symptoms, and treatment options.
Symptoms and Types
The symptoms of Kaposi’s sarcoma can vary depending on the type and stage of the disease. The most common form is classic Kaposi’s sarcoma, which primarily affects older individuals of Mediterranean or Eastern European descent. It usually presents with small, raised, reddish-purple or brownish lesions on the skin, typically on the lower extremities. In contrast, epidemic or HIV-associated Kaposi’s sarcoma primarily occurs in individuals with compromised immune systems, such as those with HIV/AIDS. It can manifest as widespread skin lesions, as well as involvement of internal organs.
Epidemiology and Risk Factors
Kaposi’s sarcoma is relatively rare, but its prevalence varies widely depending on geographic location and population groups. The incidence of classic Kaposi’s sarcoma is higher in Mediterranean, Eastern European, and African populations, while epidemic Kaposi’s sarcoma is most commonly seen in regions with a high prevalence of HIV infection, such as sub-Saharan Africa. The risk factors for Kaposi’s sarcoma include immunosuppression, especially in the context of HIV/AIDS, as well as infection with human herpesvirus 8 (HHV-8), also known as Kaposi’s sarcoma-associated herpesvirus (KSHV).
HIV and Kaposi’s Sarcoma
Correlation Between HIV and Kaposi’s Sarcoma
The correlation between HIV and Kaposi’s sarcoma is well-established. In fact, Kaposi’s sarcoma was one of the defining AIDS-related illnesses when the HIV epidemic emerged in the 1980s. HIV infection weakens the immune system, making individuals more susceptible to developing opportunistic infections and certain types of cancer, including Kaposi’s sarcoma. It is estimated that individuals with HIV/AIDS have a significantly increased risk of developing Kaposi’s sarcoma compared to the general population.
Prevalence Among HIV Patients
Kaposi’s sarcoma is one of the most common malignancies among individuals with HIV/AIDS. Prior to the introduction of combination antiretroviral therapy (ART), it was estimated that up to 20-30% of individuals with advanced HIV infection developed Kaposi’s sarcoma. However, with the effective control of HIV replication using ART, the incidence of Kaposi’s sarcoma has significantly declined in the developed world. Nevertheless, it remains a significant concern in resource-limited settings with limited access to ART and high HIV prevalence.
Transmission and Acquisition
Kaposi’s sarcoma is not directly transmitted from person to person; rather, it arises as a result of infection with HHV-8. This virus is primarily transmitted through close contact with infected individuals, such as through sexual contact, organ transplantation, or mother-to-child transmission. Individuals with HIV are more likely to acquire HHV-8 infection, and once infected, they have a higher risk of developing Kaposi’s sarcoma compared to the general population. It is important to note that not all individuals infected with HHV-8 will develop Kaposi’s sarcoma, suggesting that other factors, such as immune dysfunction, play a role in disease progression.
Understanding the Pathogenesis of Kaposi’s Sarcoma
Role of Human Herpesvirus 8 (HHV-8)
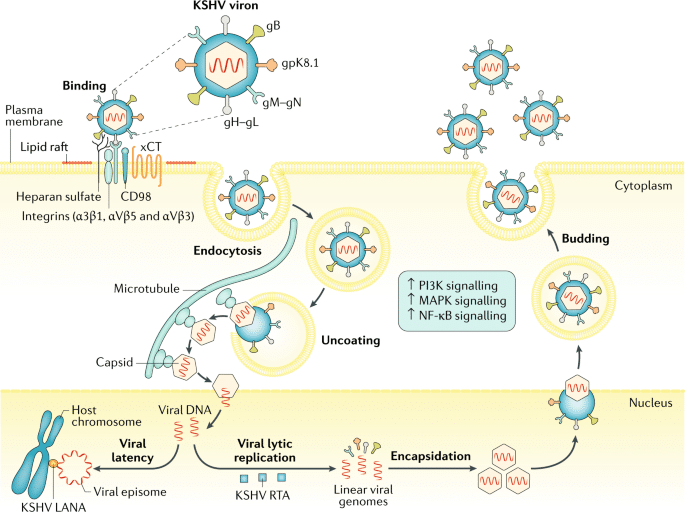
HHV-8 is a key player in the development of Kaposi’s sarcoma. This virus is known to infect the cells that line blood vessels, leading to the formation of abnormal blood vessels and the production of factors that promote tumor growth. It is still not completely understood how HHV-8 triggers the development of Kaposi’s sarcoma, but it is likely a combination of viral proteins and the host immune response that contribute to tumor formation.
Impact of Immune Dysfunction
Immunosuppression, particularly due to HIV infection, plays a crucial role in the development and progression of Kaposi’s sarcoma. HIV impairs the immune system’s ability to control HHV-8 infection, allowing the virus to replicate unchecked. In addition, HIV-associated immune dysfunction leads to a state of chronic inflammation and the release of cytokines that promote the growth of Kaposi’s sarcoma tumors. Restoring immune function through ART is a key component in the management of HIV-related Kaposi’s sarcoma.
Angiogenesis and Tumor Development
Angiogenesis, the formation of new blood vessels, is a hallmark of Kaposi’s sarcoma. HHV-8 infects the cells lining the blood vessels and induces the release of factors that stimulate angiogenesis, such as vascular endothelial growth factor (VEGF). This excessive blood vessel growth provides the necessary nutrients and oxygen to support the development of Kaposi’s sarcoma tumors. Inhibition of angiogenesis has emerged as a potential therapeutic target for Kaposi’s sarcoma treatment.
Clinical Presentation and Diagnosis
Skin Lesions and Other Manifestations
The most common clinical manifestation of Kaposi’s sarcoma is the presence of skin lesions. These lesions initially appear as small, red or purple patches that may progress to raised nodules or tumors. They can be asymptomatic or may cause itching, pain, or discomfort. In addition to skin involvement, Kaposi’s sarcoma can affect internal organs, leading to symptoms such as shortness of breath, cough, gastrointestinal bleeding, and lymph node enlargement.
Diagnostic Procedures and Tools
To diagnose Kaposi’s sarcoma, a healthcare provider may conduct a physical examination to assess the characteristic skin lesions and any other abnormal findings. A biopsy of the affected tissue is often necessary to confirm the diagnosis. This involves the removal of a small piece of the lesion for examination under a microscope. Additional tests, such as imaging studies (e.g., MRI, CT scan) and laboratory tests, may be performed to determine the extent of disease involvement and to rule out other possible conditions.

Treatment Options for Kaposi’s Sarcoma
Antiretroviral Therapy (ART)
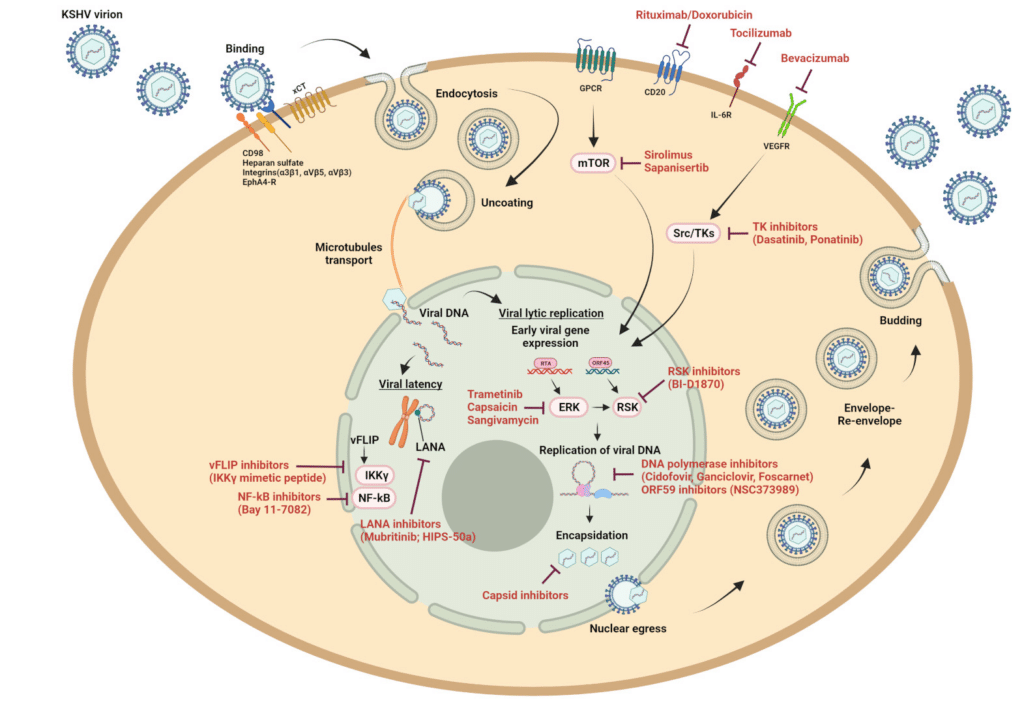
ART is a cornerstone of the management of HIV-related Kaposi’s sarcoma. By suppressing HIV replication and restoring immune function, ART can effectively control the growth and progression of Kaposi’s sarcoma tumors. In many cases, initiation or optimization of ART can result in regression or stabilization of the disease. It is crucial for individuals with HIV-related Kaposi’s sarcoma to work closely with their healthcare provider to ensure optimal HIV treatment and management.
Local Therapies
For localized Kaposi’s sarcoma lesions that are causing symptoms or aesthetic concerns, various local therapies can be employed. These include radiation therapy, surgical excision, cryotherapy (freezing the lesions), and laser therapy. These treatments can help to shrink or remove visible lesions and improve quality of life. However, local therapies are generally not effective in treating widespread or internally located Kaposi’s sarcoma tumors.
Systemic Chemotherapy
Systemic chemotherapy is considered the mainstay of treatment for advanced or disseminated Kaposi’s sarcoma. It involves the use of drugs that target rapidly dividing cancer cells, thereby reducing tumor growth and spread. Commonly used chemotherapy agents for Kaposi’s sarcoma include liposomal doxorubicin, paclitaxel, and vinblastine. Combination chemotherapy regimens are often used to improve treatment response. Chemotherapy can cause side effects, so close monitoring and supportive care are essential.
Management Strategies for HIV-related Kaposi’s Sarcoma
Role of Antiretroviral Therapy (ART)
As mentioned earlier, ART plays a critical role in the management of HIV-related Kaposi’s sarcoma. Effective control of HIV replication can lead to immune reconstitution and suppression of HHV-8, resulting in decreased tumor growth and improved prognosis. Regular monitoring of viral load and CD4 cell count is essential to assess the effectiveness of ART and guide treatment decisions.
Oncological Interventions
In cases where Kaposi’s sarcoma does not respond adequately to ART or chemotherapy, additional oncological interventions may be considered. This can involve the use of targeted therapies, such as immune checkpoint inhibitors or targeted agents that specifically inhibit HHV-8 replication or angiogenesis. Additionally, radiation therapy or surgery may be employed to address specific disease manifestations or complications.
Combination Therapies
Given the complexity of HIV-related Kaposi’s sarcoma and the need for optimal control of both HIV and cancer, combination therapies are often used. This may involve the simultaneous or sequential use of ART, chemotherapy, and local therapies, depending on the individual’s disease stage, response to treatment, and overall health status. The goal is to achieve the best possible outcomes in terms of disease control, symptom management, and quality of life.
Prognosis and Follow-up
Outcome and Survival Rates
The prognosis for individuals with Kaposi’s sarcoma depends on several factors, including the extent of disease involvement, the immune status of the individual, and the response to treatment. With the advent of effective ART and the availability of newer treatment options, the prognosis for HIV-related Kaposi’s sarcoma has significantly improved. However, late-stage or widespread disease can still be challenging to manage, and overall survival rates can vary.
Monitoring and Follow-up
Regular monitoring and follow-up are crucial for individuals with HIV-related Kaposi’s sarcoma. This includes close monitoring of the disease progression, response to treatment, and potential side effects of therapy. Healthcare providers will conduct physical examinations, order laboratory tests, and perform imaging studies as necessary to assess disease status and guide treatment decisions. Close collaboration between the individual and their healthcare team is essential for optimal disease management.
Prevention and Future Perspectives
Public Health Interventions
Public health interventions are crucial for preventing and controlling Kaposi’s sarcoma, particularly in high-risk populations. This includes promoting safe sexual practices to reduce the transmission of HIV and HHV-8, as well as providing education and resources for HIV testing, early diagnosis, and access to ART. Public health campaigns can also raise awareness about the signs and symptoms of Kaposi’s sarcoma, enabling earlier detection and intervention.
Vaccination Strategies
As HHV-8 is a key player in Kaposi’s sarcoma development, vaccination strategies aimed at preventing HHV-8 infection are an active area of research. Although no vaccine is currently available, studies are ongoing to develop vaccines that can provide protection against HHV-8 and potentially reduce the risk of Kaposi’s sarcoma.
Advancements in Research and Treatment
Advancements in research and treatment have significantly improved the outcomes for individuals with HIV-related Kaposi’s sarcoma. Ongoing studies are focused on further understanding the underlying mechanisms of Kaposi’s sarcoma pathogenesis, identifying new therapeutic targets, and developing novel treatment approaches. Promising areas of research include immunotherapy, gene therapy, and targeted therapies, which hold the potential to revolutionize the management of this complex disease.

Conclusion
Kaposi’s sarcoma is a complex disease that is intimately linked to HIV/AIDS. While significant progress has been made in our understanding of its causes and treatment options, challenges still remain. The management of HIV-related Kaposi’s sarcoma requires a multidisciplinary approach, involving close collaboration between HIV specialists, oncologists, and other healthcare providers. With ongoing research and advancements in treatment, there is hope for continued improvements in outcomes and quality of life for individuals living with this challenging condition.