In order to provide optimal care for burn patients, it is essential for nurses to be aware of important nursing considerations and effective nursing management techniques. From assessing the extent and depth of the burn injury to monitoring vital signs and preventing infection, nurses play a vital role in promoting the healing process and minimizing complications. By implementing appropriate pain management strategies, ensuring proper wound care, and offering emotional support, nurses can greatly contribute to the overall well-being and recovery of burn patients. This article will explore the key nursing considerations and nursing management approaches that are crucial in providing comprehensive care for individuals with burns.
Assessment and Documentation
Initial assessment
The initial assessment is a crucial step in managing burn patients. It involves evaluating the patient’s overall condition, determining the cause and extent of the burn, and identifying any associated injuries. During this assessment, you will need to gather information about the burn, including when and how it occurred, as well as the patient’s current symptoms and pain level. It is essential to take note of the location and size of the burn, as well as any possible complications such as inhalation injuries. This information will guide your interventions and help you communicate effectively with the healthcare team.
Burn classification
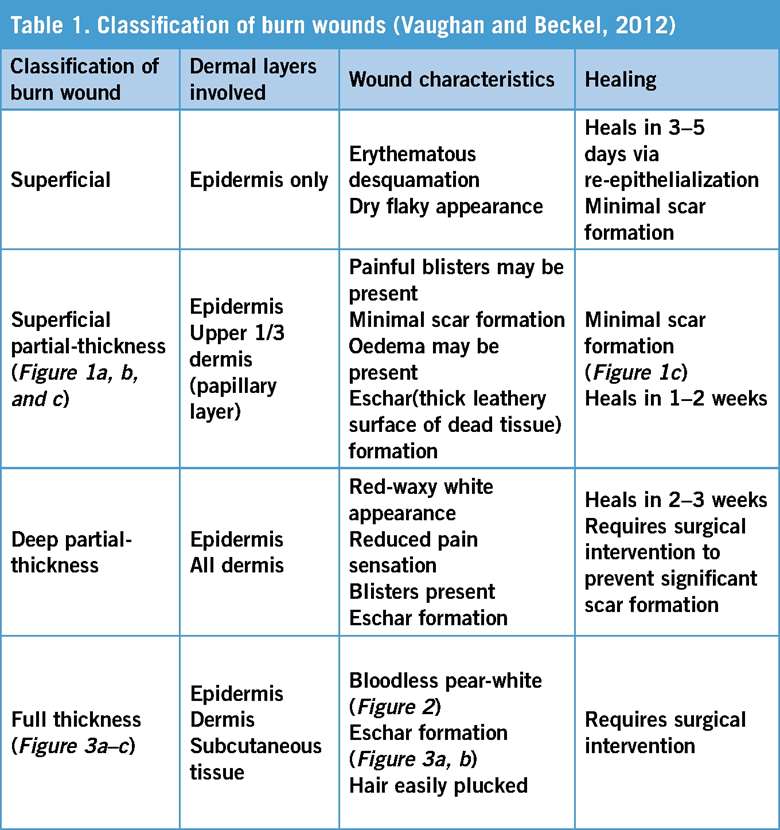
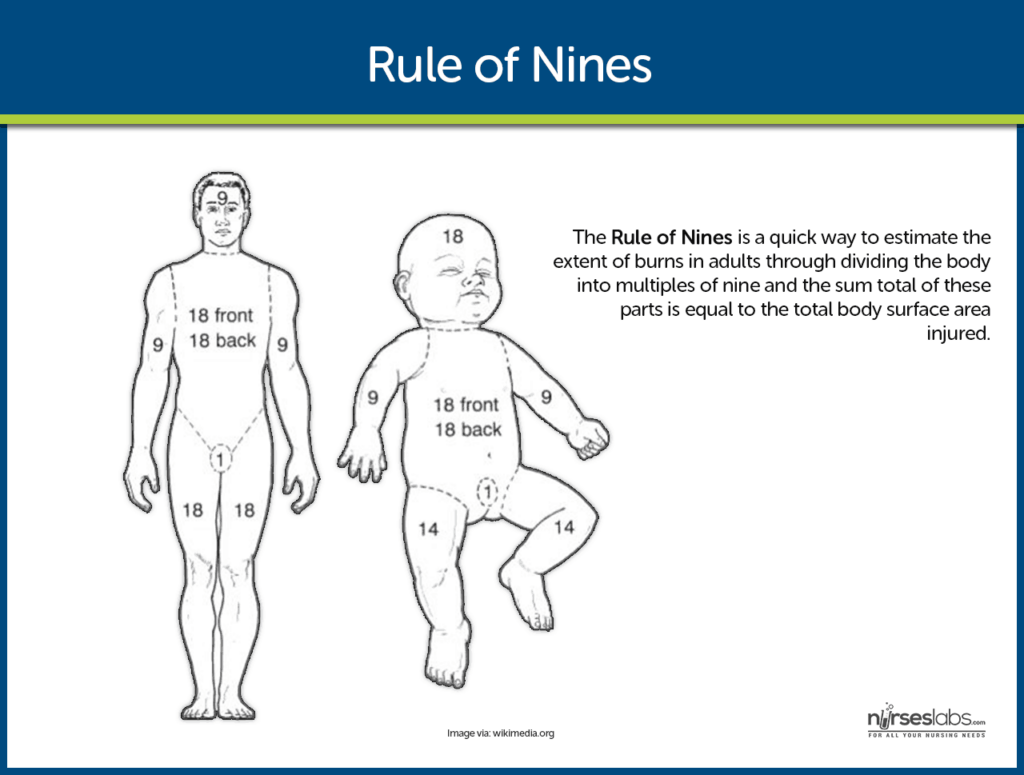
Burns can be classified into different categories based on their depth and severity. The most common classification system used is the “rule of nines” or the “Lund and Browder chart.” This system divides the body into regions, each accounting for a specific percentage of the total body surface area (TBSA). By determining the TBSA affected, you can estimate the severity of the burn and facilitate treatment decisions. Additionally, burns may be categorized as first-degree, second-degree, or third-degree, based on the depth of tissue involvement. Understanding the classification of burns is essential to provide appropriate care and interventions.
Extent and depth of burn
Assessing the extent and depth of the burn is crucial for determining the severity of the injury and planning appropriate interventions. The size of the burn is typically estimated using the “rule of nines” or the Lund and Browder chart, as mentioned earlier. Depth is determined by evaluating the damage to the layers of the skin. Superficial burns affect the epidermis, partial-thickness burns involve the dermis, while full-thickness burns extend through all layers of the skin and may involve underlying tissues. Accurate assessment of the extent and depth of the burn will guide wound care, fluid resuscitation, and other interventions.
Associated injuries
In addition to the burn itself, patients may also have other injuries or complications that need to be identified and addressed. Thermal burns are often accompanied by inhalation injuries, especially if the burn occurred in an enclosed space or involved the respiratory tract. Inhalation injuries can lead to airway edema, respiratory distress, and carbon monoxide poisoning. Other injuries, such as fractures or trauma from the burn incident, may also be present and require evaluation and treatment. Identifying and managing associated injuries is crucial for providing comprehensive care to burn patients.
Documenting findings
Accurate and detailed documentation is essential when caring for burn patients. It serves as a legal record, facilitates communication with the healthcare team, and enables continuity of care. When documenting findings, be sure to include information about the burn’s characteristics, such as location, size, and depth. Note any associated injuries or complications, as well as the patient’s vital signs, pain level, and response to interventions. Documenting the patient’s physical and emotional status, as well as their psychosocial support needs, is also important. Ensure documentation is timely, objective, and thorough, following your facility’s guidelines and standards.
Pain Management
Assessing pain
Pain assessment is crucial in burn management, as burns can be extremely painful. It is essential to regularly assess the patient’s pain, as well as their response to pain management interventions. Use a pain scale appropriate for the patient’s age and cognitive abilities to evaluate the intensity of their pain. Keep in mind that burn pain can be complex, involving both acute and chronic components. Assessing pain involves not only evaluating its severity but also considering its impact on the patient’s overall well-being and ability to participate in their care.
Pain medication administration
Effective pain management involves a multimodal approach, combining pharmacological and non-pharmacological interventions. Pharmacological interventions include the administration of analgesic medications. Non-opioid analgesics, such as non-steroidal anti-inflammatory drugs (NSAIDs), can be used for mild to moderate pain, while opioids are reserved for severe pain. Keep in mind that burn patients may require higher doses of analgesics due to increased metabolism and tolerance. Ensure proper medication administration, following your facility’s guidelines and considering any contraindications or potential side effects.
Non-pharmacological pain management techniques
Complementing pharmacological interventions, non-pharmacological pain management techniques can help provide relief and improve the patient’s overall comfort. These techniques include distraction, relaxation techniques, guided imagery, massage, and heat or cold application. Encouraging deep breathing exercises and providing support during painful procedures can also help alleviate pain. Collaborate with the patient to identify strategies that work best for them and integrate them into their care plan. Non-pharmacological pain management techniques can enhance the patient’s sense of control and well-being during their recovery.

Fluid and Electrolyte Balance
Assessing fluid status
Burn injuries disrupt the body’s fluid and electrolyte balance, leading to fluid loss and potential dehydration. Assessing the patient’s fluid status is crucial to guide fluid resuscitation and prevent complications. Monitor vital signs, including blood pressure, heart rate, respiratory rate, and urine output. Evaluate the patient’s mucous membranes for dryness and turgor for signs of dehydration. Laboratory tests, such as electrolyte panels and complete blood count (CBC), can provide further insight into the patient’s fluid and electrolyte balance. Regular assessment of fluid status will help determine the appropriate fluid replacement therapy.
IV fluid therapy
Intravenous (IV) fluid therapy plays a significant role in the management of burn patients. It aims to restore and maintain adequate fluid balance, prevent dehydration, and support tissue perfusion. The type and volume of fluids administered depend on the patient’s burn severity, extent, and comorbidities. Initially, a large-bore IV catheter is used for rapid fluid resuscitation, followed by a maintenance fluid rate adjusted according to the patient’s needs. Special attention should be given to monitoring urine output, central venous pressure, and signs of fluid overload or inadequate resuscitation.
Monitoring electrolyte levels
Burns can disrupt the body’s electrolyte balance, leading to electrolyte imbalances such as hyperkalemia or hypokalemia. Regular monitoring of electrolyte levels is essential to detect and correct any abnormalities promptly. Common electrolytes to monitor include sodium, potassium, calcium, and magnesium. In addition to laboratory tests, assess the patient’s clinical signs and symptoms, such as muscle weakness, cardiac arrhythmias, or neuromuscular irritability. Collaborate with the healthcare team to adjust IV fluids and electrolyte replacement, ensuring the patient maintains optimal electrolyte levels.
Preventing fluid overload
While fluid resuscitation is essential, it is crucial to monitor for signs of fluid overload to prevent complications. These signs may include edema, pulmonary congestion, decreased oxygen saturation, and increased blood pressure. Regularly assess the patient’s lungs for crackles or difficulty breathing and monitor urine output for any sudden changes. Adjust fluid administration according to the patient’s response and closely monitor fluid intake and output. Collaboration with the healthcare team and close monitoring will help prevent fluid overload and promote optimal fluid and electrolyte balance.
Wound Care
Cleaning the burn wound
Proper wound care is essential for promoting healing and preventing infection in burn patients. Cleaning the burn wound is a critical aspect of wound care. Start by ensuring a clean and sterile environment, following infection control protocols. Depending on the burn’s severity and the healthcare facility’s guidelines, you may use various techniques to clean the wound, such as gentle irrigation with sterile saline or antimicrobial solutions. Remove any debris or non-viable tissue while minimizing trauma to the wound. Proper wound cleaning helps remove bacteria and promote an optimal environment for healing.
Applying dressings
After cleaning the burn wound, applying appropriate dressings is necessary to protect the wound and facilitate healing. The choice of dressings depends on the burn’s severity and depth, as well as the patient’s individual needs. Dressings may include non-adherent dressings, hydrogels, foams, or antimicrobial dressings. These dressings can provide moisture balance, thermal insulation, and protection from external contaminants. Ensure proper application and securement of dressings, while also considering the patient’s comfort and any previous allergies or sensitivities. Regularly assess the dressings for signs of infection or inadequate wound healing.
Preventing infection
Preventing infection is vital in burn management, as burns create an open wound susceptible to microbial invasion. Infection can significantly delay wound healing and lead to systemic complications. To prevent infection, practice thorough hand hygiene before and after wound care. Use sterile techniques and sterile dressings when handling the burn wound. Properly disinfect any equipment used during wound care. Administer prophylactic antibiotics as prescribed, following appropriate guidelines and considering the patient’s allergies or sensitivities. Regularly assess the burn wound for signs of infection, such as increased erythema, swelling, or purulent discharge.
Promoting wound healing
Promoting wound healing is a fundamental goal in burn care. Besides appropriate wound care, several interventions can help facilitate the healing process. Maintain a moist wound environment by using appropriate dressings or topical agents. This promotes re-epithelialization and reduces pain. Adequate nutrition, including an increased protein intake, is crucial for wound healing. Collaborate with a dietitian to ensure the patient’s nutritional needs are met. Manage pain effectively, as pain can impair wound healing. Evaluate the patient’s overall health status, including comorbidities, and address any factors that may impede wound healing. Regularly assess the wound’s progress and adjust interventions as needed.

Infection Control
Hand hygiene
Proper hand hygiene is crucial in preventing the spread of infection within the healthcare setting. Before and after every patient interaction, wash your hands following prescribed hand hygiene protocols. Use soap and water for visibly soiled hands or an alcohol-based hand sanitizer when hands are not visibly soiled. Pay attention to all areas, including between fingers, fingertips, and wrists. Hand hygiene is especially important before and after any wound care or invasive procedures, to reduce the risk of introducing pathogens into the burn wound.
Isolation precautions
Burn patients may require isolation precautions, depending on the severity of their burn and the presence of infections or other communicable diseases. Follow your facility’s guidelines for appropriate isolation protocols, including the use of personal protective equipment (PPE). Isolation precautions may involve contact precautions, droplet precautions, or airborne precautions, depending on the specific pathogens involved. Ensure proper donning and doffing of PPE to prevent cross-contamination. Educate the patient, their family, and other healthcare providers about the importance of adherence to isolation precautions to minimize the risk of spreading infections.
Antibiotic administration
Antibiotics play a crucial role in preventing and treating infections in burn patients. Prophylactic antibiotics may be prescribed in specific cases, such as severe burns or when inhalation injuries are present. Antibiotic selection should be based on local susceptibility patterns and the patient’s allergies or sensitivities. Administer antibiotics as prescribed, following appropriate guidelines for dosage, route, and duration. Ensure timely administration and monitor for any signs of adverse reactions or superinfections. Collaboration with the healthcare team, including infectious disease specialists, may be required in cases of suspected or confirmed infections.
Monitoring for signs of infection
Regular monitoring for signs of infection is crucial in burn management. Assess the burn wound for increasing erythema, edema, warmth, or purulent discharge, which may indicate an infection. Monitor the patient’s vital signs, including temperature, heart rate, and white blood cell count, as they can provide valuable information about the presence of infection. Be vigilant for any systemic signs, such as fever, chills, or confusion. Communicate any concerning findings to the healthcare team promptly. Early detection and treatment of infections are essential in preventing serious complications and promoting successful burn healing.
Nutritional Support
Assessing nutritional needs
Assessing a burn patient’s nutritional needs is crucial for supporting the healing process and preventing malnutrition. Burns increase metabolic demands, which may necessitate increased caloric and protein intake. Work closely with a dietitian to evaluate the patient’s nutritional status and develop an appropriate nutrition plan. Consider factors such as the patient’s age, weight, burn severity, comorbidities, and overall health. Monitor weight changes, intake, and output to assess the effectiveness of the nutrition plan. Regular reassessment of nutritional needs will help ensure the patient receives adequate nutrition to support recovery.
Enteral or parenteral nutrition
Enteral or parenteral nutrition may be required for burn patients who cannot meet their nutritional needs orally. Enteral nutrition involves providing nutrients through a feeding tube, usually directly into the stomach or small intestine, while parenteral nutrition is administered intravenously. The choice between enteral and parenteral nutrition depends on the patient’s condition, the function of their gastrointestinal tract, and their ability to tolerate oral intake. Collaborate with a dietitian and the healthcare team to determine the most appropriate route and formulation for nutritional support, considering the patient’s specific needs and goals.
Collaborating with a dietitian
Collaboration with a dietitian is essential in providing optimal nutritional support to burn patients. Dietitians are experts in assessing nutritional requirements, developing nutrition plans, and monitoring the patient’s response to interventions. Work closely with the dietitian to ensure the patient’s nutritional goals are met and to address any barriers or challenges that may impede adequate nutritional intake. Regular communication, documentation, and interdisciplinary collaboration will enhance the patient’s nutritional care and support their recovery.
Psychosocial Support
Assessing emotional well-being
Burn injuries can have significant physical and emotional impacts on patients. Assessing the patient’s emotional well-being is crucial to identify any psychological distress or coping challenges. Use appropriate assessment tools and techniques to evaluate the patient’s emotional state, such as anxiety, depression, and post-traumatic stress symptoms. Assessing emotional well-being involves actively listening to the patient, asking open-ended questions, and being sensitive to their unique experiences and needs. Regularly reassess the patient’s emotional well-being throughout their burn care journey to ensure appropriate psychosocial support.
Providing emotional support
Providing emotional support is a fundamental aspect of burn care. Be attentive, empathetic, and supportive in your interactions with the patient. Acknowledge their emotional challenges and validate their feelings. Provide information and education about the burn healing process, potential outcomes, and available resources. Encourage the patient to express their concerns, fears, and emotions, and foster a caring and non-judgmental environment. Be an active listener and provide appropriate referrals to other healthcare professionals, such as psychologists or counselors, as needed. Your emotional support can significantly impact the patient’s overall well-being and quality of life.
Referring for counseling services
In some cases, burn patients may benefit from professional counseling services to address their emotional and psychological needs. Referring the patient for counseling allows them to receive specialized support from trained professionals, such as psychologists or counselors. Collaborate with the healthcare team to identify appropriate counseling services and facilitate the referral process. Educate the patient and their family about the potential benefits of counseling and encourage their active participation. Regularly assess the patient’s progress in counseling and communicate with the counselor to ensure continuity of care and support for the patient’s psychosocial well-being.
Respiratory Management
Assessing airway patency
Respiratory management is crucial in burn patients, especially those with inhalation injuries. Assess the patient’s airway patency regularly, evaluating for any signs of airway compromise, such as stridor, hoarseness, or difficulty breathing. Monitor oxygen saturation levels, respiratory rate, depth, and effort. Collaborate with the healthcare team, including respiratory therapists, to perform more advanced assessments, such as bronchoscopy or arterial blood gas analysis if necessary. Prompt recognition and intervention for airway compromise are essential to ensure the patient’s respiratory stability and prevent further complications.
Administering supplemental oxygen
Supplemental oxygen may be required in burn patients with respiratory distress or inadequate oxygenation. Administer supplemental oxygen as prescribed, carefully monitoring the patient’s oxygen saturation levels and respiratory status. Use appropriate oxygen delivery systems, such as nasal cannula, face mask, or ventilator support, depending on the patient’s needs and the severity of their respiratory compromise. Ensure proper fit and comfort of any oxygen delivery devices, educating the patient and their family about their purpose and usage. Collaborate with respiratory therapists to optimize oxygenation and promote the patient’s respiratory well-being.
Monitoring respiratory status
Continuous monitoring of the burn patient’s respiratory status is essential to detect any worsening or improvement in their condition. Assess respiratory rate, depth, and effort at regular intervals. Observe for signs of respiratory distress, such as increased work of breathing, use of accessory muscles, or restlessness. Auscultate lung sounds to evaluate for any adventitious sounds, such as crackles or wheezes. Monitor oxygen saturation levels continuously and maintain target values appropriate for the patient’s condition. Promptly communicate any concerning findings to the healthcare team for further evaluation and intervention.
Suctioning if necessary
Suctioning may be necessary in burn patients with excessive mucus production or impaired airway clearance. Before suctioning, assess the patient’s respiratory status, and ensure proper positioning and suctioning technique. Follow your facility’s guidelines and use appropriate suctioning equipment. Apply sterile technique, and ensure suctioning is done gently and within the patient’s tolerance. Monitor the patient’s response, including oxygen saturation levels and respiratory distress during and after the procedure. Collaborate with the healthcare team, especially respiratory therapists, for guidance and support during suctioning interventions.

Preventing Complications
Preventing contractures
Contractures, the permanent shortening of muscles and tendons, can occur as a complication of burn injuries. Preventing contractures involves early and aggressive mobilization and range of motion exercises. Collaborate with physical and occupational therapists to develop an individualized mobilization plan for the patient. Encourage regular and active movement of the affected joints and provide appropriate splinting or positioning to maintain proper alignment. Monitor the patient’s progress, evaluate their range of motion regularly, and adjust interventions as needed. Preventing contractures is essential to promote functional recovery and provide the best possible outcome for the patient.
Preventing deep vein thrombosis
Burn patients are at increased risk for deep vein thrombosis (DVT) due to immobility, hypercoagulability, and endothelial damage. Preventing DVT involves several measures. Encourage early mobilization and ambulation as appropriate to prevent venous stasis. Use compression stockings or intermittent pneumatic compression devices to improve circulation and prevent blood clots. Administer prophylactic anticoagulant medications, such as low molecular weight heparin, as prescribed. Monitor the patient for signs and symptoms of DVT, such as swelling, pain, or redness in the extremities. Prompt identification and intervention for DVT can help prevent life-threatening complications such as pulmonary embolism.
Preventing pressure ulcers
Pressure ulcers, also known as bedsores, can develop in burn patients due to prolonged immobility, compromised tissue perfusion, and impaired sensation. Preventing pressure ulcers involves regular assessment of the patient’s skin integrity and implementing preventive measures. Use appropriate support surfaces, such as pressure-relieving mattresses or cushions, to reduce pressure on vulnerable areas. Implement repositioning schedules and encourage frequent position changes to relieve pressure. Maintain optimal skin hygiene and moisture balance, keeping the skin clean, dry, and free from irritants. Educate the patient, their family, and other caregivers about pressure ulcer prevention and early detection.
Collaboration and Communication
Interprofessional collaboration
Managing burn patients requires effective collaboration among various healthcare professionals. Work closely with the interdisciplinary team, including physicians, nurses, physical and occupational therapists, respiratory therapists, dietitians, and psychologists. Recognize and respect the unique expertise each team member brings to the patient’s care. Collaborate in developing and implementing the patient’s care plan, addressing their physical, emotional, and psychosocial needs. Regularly communicate and share relevant information to facilitate continuity of care and promote the patient’s well-being. Actively participate in interdisciplinary meetings or rounds to discuss patient progress and make collaborative decisions.
Effective communication with the healthcare team
Communication is essential in providing safe and coordinated care for burn patients. Maintain open and clear lines of communication with the healthcare team. Effectively communicate and document the patient’s assessment findings, interventions, and response to treatment. Ensure timely sharing of information and any changes in the patient’s condition. Collaborate with other healthcare providers to identify and address potential barriers or challenges in the patient’s care. Regularly update the healthcare team on the patient’s progress and involve them in decision-making processes. Effective communication fosters teamwork, enhances patient safety, and promotes positive outcomes.
Involving the patient and family in care decisions
Involving the patient and their family in care decisions is essential for person-centered and family-centered care. Recognize the patient and their family as active partners in the care process. Involve them in discussions about treatment options, goals of care, and discharge planning. Provide clear and understandable explanations about the patient’s condition, treatment procedures, and potential outcomes. Encourage the patient and their family to ask questions, express their concerns, and actively participate in their care. Promote shared decision-making and respect the patient’s autonomy and preferences. Involving the patient and family in care decisions supports their engagement and satisfaction with their healthcare experience.
In conclusion, providing comprehensive care for burn patients involves a holistic approach encompassing assessment and documentation, pain management, fluid and electrolyte balance, wound care, infection control, nutritional support, psychosocial support, respiratory management, prevention of complications, and effective collaboration and communication. By addressing each aspect with diligence and compassion, nurses can contribute to the optimal recovery and well-being of burn patients and promote their successful rehabilitation.