In this article, you will discover essential nursing considerations for GERD (Gastroesophageal Reflux Disease) and the strategies that nurses can employ in effectively managing this condition. From understanding the causes of GERD to implementing preventive measures, this comprehensive guide will equip you with the knowledge and tools needed to provide optimal care for patients suffering from GERD. With a focus on promoting patient comfort, preventing complications, and improving quality of life, these nursing considerations will play a vital role in ensuring the well-being of individuals with GERD.

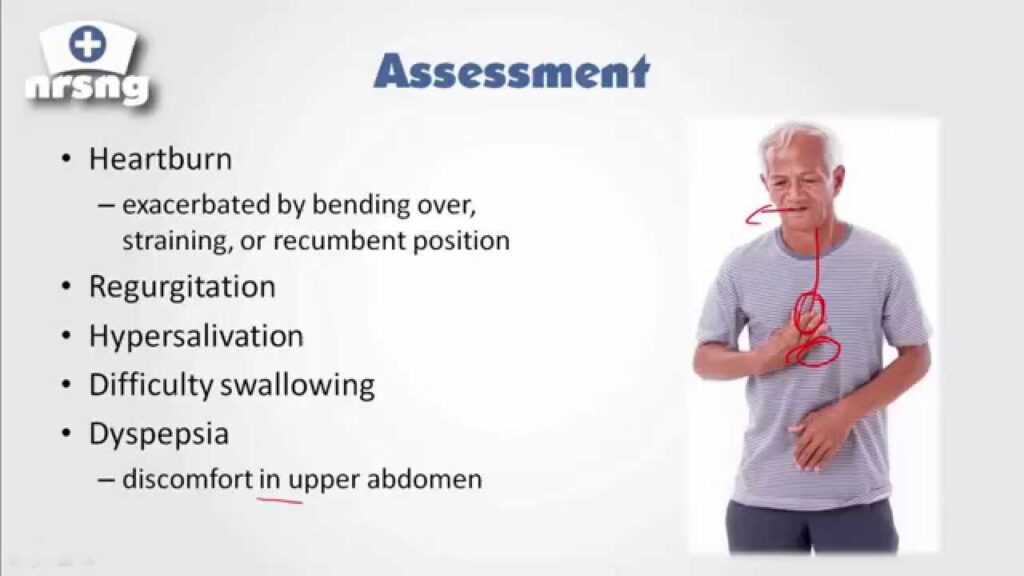
Assessment
Health history
When assessing a patient with GERD, it is important to obtain a detailed health history. This includes asking about any previous diagnosis of GERD, as well as any symptoms experienced such as heartburn, regurgitation, or difficulty swallowing. Additionally, the nurse should inquire about any other medical conditions the patient may have, as well as any medications they are currently taking. Understanding the patient’s health history will help guide the nurse in developing an appropriate care plan.
Physical examination
A thorough physical examination is important in evaluating a patient with GERD. The nurse should assess the patient’s vital signs, including blood pressure, heart rate, and respiratory rate. They should also inspect the patient’s abdomen for any signs of distension or tenderness. A comprehensive examination of the throat and mouth should be performed, as GERD can sometimes cause inflammation or damage to these areas. It is also important to check for any signs of weight loss or malnutrition, as these can be potential complications of GERD.
Symptom assessment
Assessing the patient’s symptoms is crucial in managing GERD. The nurse should ask the patient about the frequency and severity of their symptoms, as well as any factors that seem to trigger or worsen them. Common symptoms of GERD include heartburn, regurgitation, and indigestion. It is also important to inquire about any other symptoms the patient may be experiencing, such as chest pain or difficulty swallowing. Understanding the patient’s symptoms will help guide the nurse in developing an individualized care plan.
Diagnostic Tests
Esophageal pH monitoring
Esophageal pH monitoring is a common diagnostic test used to evaluate GERD. This test involves placing a small tube through the nose or mouth and into the esophagus. The tube measures the pH levels in the esophagus as the patient goes about their normal activities. This test can help determine the amount of acid in the esophagus and how often acid reflux occurs. Esophageal pH monitoring is often recommended for patients with persistent or atypical symptoms of GERD.
Upper gastrointestinal endoscopy
An upper gastrointestinal endoscopy, also known as an EGD, is a procedure used to visualize the inside of the esophagus, stomach, and small intestine. During this test, a thin tube with a camera on the end is inserted through the mouth and into the digestive tract. This allows the healthcare provider to assess the lining of the esophagus for signs of inflammation or damage. An EGD can also be used to take biopsies if needed. This test is often performed in patients with suspected complications of GERD, such as Barrett’s esophagus or esophageal ulcers.
Barium swallow test
A barium swallow test, also known as an esophagram, is a radiographic study used to evaluate the structure and function of the esophagus. During this test, the patient swallows a liquid containing barium, a contrast material that shows up on X-ray. X-ray images are then taken as the barium passes through the esophagus and into the stomach. This test can help identify any structural abnormalities or motility disorders that may be contributing to the patient’s symptoms. A barium swallow test is often performed in patients with suspected GERD who have not responded to initial treatment.
Esophageal manometry
Esophageal manometry is a diagnostic test used to evaluate the function of the esophagus and lower esophageal sphincter (LES). This test measures the pressure and coordination of the muscles in the esophagus as the patient swallows. Esophageal manometry can help determine if the LES is functioning properly and if there are any motility disorders present. This test is often performed in patients with suspected esophageal motility disorders or if surgery is being considered as a treatment option.

Medications
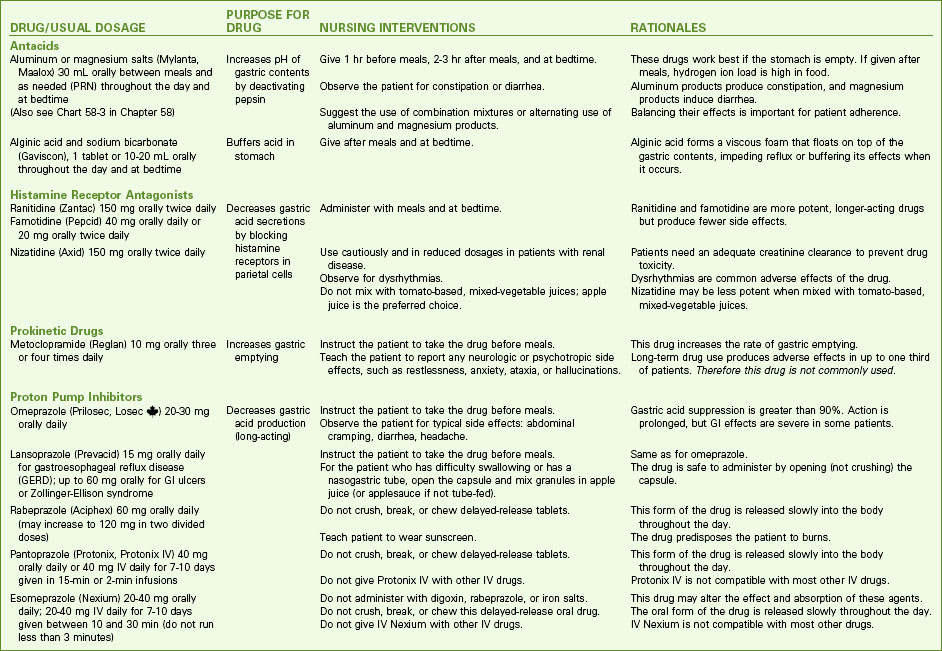
Proton pump inhibitors (PPIs)
Proton pump inhibitors (PPIs) are a class of medications commonly used to treat GERD. These medications work by reducing the production of stomach acid. PPIs are highly effective in controlling symptoms of GERD and promoting healing of the esophagus. They are typically taken once daily, usually before breakfast. It is important for patients to take PPIs as prescribed and to continue taking them for the full recommended duration of treatment to achieve optimal results.
H2 receptor blockers
H2 receptor blockers, also known as H2 blockers, are another class of medications used to treat GERD. These medications work by reducing the production of stomach acid, but they are not as potent as PPIs. H2 blockers are often used as an alternative to PPIs or as an adjunctive therapy in patients with mild to moderate symptoms of GERD. H2 blockers are typically taken as needed, before a meal or at bedtime. It is important for patients to follow the dosing instructions provided by their healthcare provider.
Antacids
Antacids are medications that provide immediate relief from heartburn and indigestion by neutralizing stomach acid. They are available over the counter and can be taken as needed. Antacids can be used alone for mild symptoms of GERD or in combination with other medications for more severe symptoms. It is important for patients to be aware that prolonged or excessive use of antacids can lead to electrolyte imbalances and other complications, so they should be used under the guidance of a healthcare provider.
Prokinetic agents
Prokinetic agents are medications that help improve the movement of food through the digestive tract. They work by increasing the contractions of the esophagus and stomach, which can help prevent acid reflux. Prokinetic agents are typically used in combination with other medications for the treatment of GERD, particularly in patients with delayed gastric emptying or motility disorders. It is important for patients to be aware that prokinetic agents can have side effects such as diarrhea or fatigue, so they should be used under the supervision of a healthcare provider.
Lifestyle Modifications
Dietary changes
Making dietary changes is an important aspect of managing GERD. Patients should avoid trigger foods and beverages such as spicy foods, citrus fruits, tomatoes, chocolate, caffeine, and alcohol, as these can worsen symptoms of acid reflux. Instead, they should focus on consuming a well-balanced diet that includes lean proteins, whole grains, fruits, vegetables, and low-fat dairy products. It may also be helpful for patients to eat smaller, more frequent meals rather than large, heavy meals, as this can help prevent acid reflux.
Weight management
Maintaining a healthy weight is important in managing GERD. Excess weight can put pressure on the abdomen, which can cause acid reflux. Patients who are overweight or obese should work with their healthcare provider to develop a safe and effective weight loss plan. This may include making dietary changes, increasing physical activity, and seeking support from a registered dietitian or weight loss specialist. Losing weight can help reduce symptoms of GERD and improve overall health.
Elevation of the head of the bed
Raising the head of the bed by 6-8 inches can help prevent acid reflux during sleep. This can be achieved by using bed risers or placing blocks under the bed legs at the head of the bed. Elevating the head of the bed helps keep stomach acid in the stomach and prevents it from flowing back into the esophagus. Patients should also avoid lying down for at least 2-3 hours after eating to allow for proper digestion and prevent acid reflux.
Smoking cessation
Smoking is a known risk factor for GERD and can worsen symptoms. It can also weaken the lower esophageal sphincter, which allows stomach acid to flow back into the esophagus. Patients who smoke should be encouraged to quit smoking to reduce symptoms of GERD. Healthcare providers can provide resources and support to help patients quit smoking, such as smoking cessation medications, counseling services, and support groups.
Patient Education
Understanding GERD
Educating patients about GERD is an essential part of their care. Patients should be provided with information about what GERD is and how it affects the body. They should understand that GERD occurs when stomach acid flows back into the esophagus, causing symptoms such as heartburn, regurgitation, and indigestion. Patients should also be informed about the potential complications of GERD, such as esophageal strictures, Barrett’s esophagus, esophageal ulcers, and esophageal cancer. Understanding the disease process and potential complications can help patients make informed decisions about their treatment and lifestyle choices.
Management strategies
Patients should be educated about various management strategies for GERD. This includes information about lifestyle modifications, such as dietary changes, weight management, elevation of the head of the bed, and smoking cessation. Patients should also be informed about the different medications used to treat GERD, including PPIs, H2 blockers, antacids, and prokinetic agents. They should understand the benefits and potential side effects of each medication and how to take them correctly. Additionally, patients should be informed about the importance of adhering to their treatment plan and seeking regular follow-up with their healthcare provider.
Medication adherence
Adherence to medication therapy is crucial in managing GERD. Patients should be educated about the importance of taking their medications as prescribed and for the full recommended duration of treatment. They should understand how the medications work and how they can help control their symptoms and promote healing of the esophagus. Patients should also be informed about potential side effects and how to manage them. It is important for patients to communicate with their healthcare provider if they have any questions or concerns about their medications.
Importance of lifestyle modifications
Patients should understand the importance of lifestyle modifications in managing GERD. While medications can help control symptoms, lifestyle changes are necessary to address the underlying causes of GERD. Patients should be informed about the impact of dietary choices, weight management, elevation of the head of the bed, and smoking cessation on their symptoms and overall health. They should understand that making these changes can help alleviate their symptoms and reduce the risk of complications. It is important for patients to be motivated and committed to making these lifestyle modifications for long-term management of GERD.
Risk Factors
Obesity
Obesity is a significant risk factor for GERD. Excess weight can put pressure on the abdomen, which can cause the lower esophageal sphincter to weaken and allow stomach acid to flow back into the esophagus. Patients who are overweight or obese should be encouraged to lose weight through a combination of dietary changes, increased physical activity, and behavior modifications. Losing weight can help reduce symptoms of GERD and improve overall health.
Hiatal hernia
A hiatal hernia is another risk factor for GERD. This condition occurs when part of the stomach pushes up into the chest through the diaphragm, which can weaken the lower esophageal sphincter and allow acid reflux to occur. Patients with a hiatal hernia may require additional management strategies, such as positioning techniques and surgical interventions, to manage their symptoms effectively. It is important for patients with a hiatal hernia to work closely with their healthcare provider to develop an individualized care plan.
Smoking
Smoking is a known risk factor for GERD. It can weaken the lower esophageal sphincter, which allows stomach acid to flow back into the esophagus. Additionally, smoking can increase stomach acid production and irritate the lining of the esophagus. Patients who smoke should be encouraged to quit smoking to reduce symptoms of GERD. Healthcare providers can provide resources and support to help patients quit smoking, such as smoking cessation medications, counseling services, and support groups.
Pregnancy
Pregnancy is a risk factor for GERD due to hormonal changes and the pressure exerted on the abdomen by the growing fetus. Pregnant women may experience symptoms of GERD, such as heartburn and indigestion, particularly in the later stages of pregnancy. Lifestyle modifications and over-the-counter antacids may be recommended as first-line treatment options in pregnant women. It is important for pregnant women with GERD to consult with their healthcare provider before taking any medications to ensure the safety of both the mother and the baby.
Complications
Esophageal strictures
Esophageal strictures are one of the complications that can arise from untreated or poorly controlled GERD. These are narrowings or constrictions in the esophagus that can make it difficult for food and liquids to pass through. Esophageal strictures can cause symptoms such as difficulty swallowing, chest pain, and food getting stuck in the throat. Treatment options for esophageal strictures may include endoscopic dilation, where a balloon is used to stretch the narrowed area, or surgery in more severe cases. Prevention of strictures is key through proper management of GERD.
Barrett’s esophagus
Barrett’s esophagus is a condition that develops when the lining of the esophagus undergoes changes, usually as a result of chronic acid exposure from GERD. This change in the lining can increase the risk of developing esophageal cancer. Patients with Barrett’s esophagus may need to undergo regular surveillance with upper endoscopies and biopsies to monitor for any signs of dysplasia or cancer. Treatment options for Barrett’s esophagus may include medication management, endoscopic therapy, or surgery, depending on the severity of the condition.
Esophageal ulcers
Esophageal ulcers can develop as a complication of untreated or poorly controlled GERD. These are open sores or wounds that form in the lining of the esophagus. Esophageal ulcers can cause symptoms such as chest pain, difficulty swallowing, and bleeding. Treatment options for esophageal ulcers may include medication management to reduce stomach acid production and promote healing, as well as lifestyle modifications to address the underlying causes of GERD. Prevention of ulcers involves proper management of GERD symptoms and following lifestyle modifications.
Esophageal cancer
Esophageal cancer is a potential complication of long-term, untreated GERD. Chronic acid exposure and inflammation can lead to the development of cancerous cells in the lining of the esophagus. Esophageal cancer often presents at an advanced stage and can have a poor prognosis. Regular surveillance and early detection of any precancerous changes, such as Barrett’s esophagus, are crucial in preventing the progression to esophageal cancer. Patients with GERD should be informed about the risk of esophageal cancer and the importance of regular follow-up with their healthcare provider.
Nutritional Considerations
Avoiding trigger foods
Patients with GERD should be advised to avoid trigger foods and beverages that can worsen their symptoms. These may include spicy foods, citrus fruits, tomatoes, chocolate, caffeine, and alcohol. These foods can increase stomach acid production and relax the lower esophageal sphincter, leading to acid reflux. Patients can work with a registered dietitian to develop a personalized meal plan that avoids trigger foods while ensuring proper nutrition.
Eating smaller, more frequent meals
Patients with GERD should be encouraged to eat smaller, more frequent meals rather than large, heavy meals. This can help prevent excess pressure on the stomach and reduce the risk of acid reflux. Patients should also avoid lying down for at least 2-3 hours after eating to allow for proper digestion. It may be helpful for patients to incorporate snacks between meals to help maintain stable blood sugar levels and prevent excessive hunger, which can trigger acid reflux.
Maintaining adequate hydration
Staying adequately hydrated is important in managing GERD. Drinking enough water can help dilute stomach acid and promote proper digestion. Patients should aim to drink at least 8 cups of water per day, or more if recommended by their healthcare provider. It is important for patients to avoid sugary beverages, carbonated drinks, and drinks that contain caffeine, as these can worsen symptoms of GERD.
Monitoring nutritional deficiencies
Patients with long-term GERD or those who have undergone certain treatments, such as surgery or medication management, may be at risk for nutritional deficiencies. This is because certain medications can interfere with the absorption of essential nutrients, and chronic acid reflux can affect the digestion and absorption of nutrients. Patients should be monitored for signs of nutritional deficiencies, such as fatigue, weakness, anemia, or changes in hair or nails. If deficiencies are identified, patients may need to take supplements or make dietary modifications under the guidance of a registered dietitian.
Collaborative Care
Referral to a gastroenterologist
In the management of GERD, collaborative care with a gastroenterologist is often necessary. Gastroenterologists specialize in diagnosing and treating conditions of the digestive tract, including GERD. Primary care providers may refer patients to a gastroenterologist for further evaluation and management if symptoms are severe, do not respond to initial treatment, or if complications are suspected. Gastroenterologists can perform specialized tests, such as esophageal pH monitoring, upper gastrointestinal endoscopy, or esophageal manometry, to further evaluate the patient’s condition and guide treatment decisions.
Collaboration with a registered dietitian
Registered dietitians play a key role in managing GERD through dietary modifications. They can work with patients to develop personalized meal plans that avoid trigger foods and ensure proper nutrition. Dietitians can provide education about portion sizes, food choices, and meal timing to help reduce symptoms of GERD and promote overall health. Collaborating with a registered dietitian can help patients make sustainable lifestyle changes and achieve their treatment goals.
Coordination with other healthcare providers
The management of GERD often involves coordination with other healthcare providers to address the various aspects of the patient’s care. This may include collaborating with a primary care provider, gastroenterologist, registered dietitian, pharmacist, and other specialists such as surgeons or pulmonologists, depending on the patient’s individual needs. Effective coordination and communication among healthcare providers are crucial in ensuring that the patient receives comprehensive and individualized care.
Multidisciplinary approach
GERD is a complex condition that requires a multidisciplinary approach to management. The collaboration of various healthcare providers, such as nurses, physicians, dietitians, and other specialists, ensures that the patient receives comprehensive care that addresses all aspects of their condition. A multidisciplinary approach can help optimize treatment outcomes, improve patient satisfaction, and prevent complications. It is important for healthcare providers to communicate and work together to develop an individualized care plan that meets the unique needs of each patient.
Patient Support
Emotional support
Living with a chronic condition like GERD can be emotionally challenging. Patients may experience feelings of frustration, anxiety, or depression due to the impact of their symptoms on their daily life. Providing emotional support to patients is an important aspect of their care. Nurses can offer empathy, active listening, and reassurance to help patients cope with their emotions. Patients may also benefit from counseling services or support groups that provide a safe space to discuss their experiences and learn from others facing similar challenges.
Support groups
Support groups can be a valuable resource for patients with GERD. Support groups provide an opportunity for patients to connect with others who are going through similar experiences, share coping strategies, and learn from one another. Support groups can provide emotional support, practical tips, and information about managing GERD. They can also help patients feel less isolated and understand that they are not alone in their journey.
Counseling services
Counseling services can play a crucial role in helping patients manage the emotional aspects of living with GERD. Counseling can help patients develop coping strategies for dealing with the challenges and lifestyle changes associated with their condition. Counseling can also provide support in managing stress, anxiety, and depression, which can exacerbate symptoms of GERD. Referring patients to counseling services can help them develop the necessary skills and mindset to navigate their condition successfully.
Home health services
In some cases, patients with severe or complicated GERD may benefit from home health services. Home health services provide medical care, education, and support in the comfort of the patient’s home. This can be especially beneficial for patients who have difficulty traveling to appointments or who require additional assistance with their care. Home health nurses can provide ongoing monitoring, medication management, wound care, and education to help patients manage their condition and prevent complications.