In this article, you will discover valuable insights into nursing considerations and management strategies for individuals with panic-anxiety disorders. As a nurse, it is crucial to understand the unique challenges that these individuals face and to provide them with the support and care they need. We will explore various aspects of nursing considerations, such as assessment, intervention, and education, that are essential for effectively managing panic-anxiety disorders. By implementing these considerations, you can make a significant difference in the lives of your patients who are battling panic-anxiety disorders.
Assessment
Physical assessment
During the assessment of a patient with panic-anxiety disorder, it is crucial to conduct a thorough physical examination. This examination should include the patient’s vital signs, such as blood pressure, heart rate, and respiratory rate. Additionally, it is important to assess for any physical symptoms that may be associated with anxiety, such as chest pain, shortness of breath, or gastrointestinal disturbances. The nurse should also inquire about the patient’s sleep patterns, appetite, and energy levels, as these can provide valuable insights into the overall physical well-being of the individual.
Psychosocial assessment
In addition to the physical assessment, a comprehensive psychosocial assessment is necessary to gain a deeper understanding of the patient’s psychological and emotional well-being. This assessment should explore the patient’s perception of anxiety, triggers, and coping mechanisms. It is also vital to evaluate the patient’s support system, including family dynamics, relationships, and social support. Assessing the patient’s level of functioning, including work, school, and daily activities, can help identify the impact of panic-anxiety disorder on their overall quality of life.
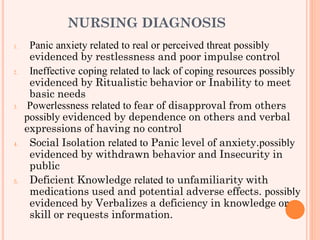
Diagnosis
Diagnostic criteria
To establish a diagnosis of panic-anxiety disorder, healthcare professionals refer to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria. The criteria include recurrent, unexpected panic attacks, which are sudden and intense episodes of fear or discomfort. These attacks are often accompanied by physical symptoms, such as palpitations, chest pain, sweating, and shortness of breath. Furthermore, the presence of persistent worry about additional panic attacks or their consequences is a common feature of this disorder.
Differential diagnoses
While panic-anxiety disorder has distinct diagnostic criteria, it is essential to consider other potential diagnoses to ensure accurate treatment. Some conditions that may present with similar symptoms include generalized anxiety disorder, social anxiety disorder, specific phobias, and medical conditions such as thyroid disorders or cardiovascular disease. Thorough assessment and collaboration with the multidisciplinary team are crucial for accurate differential diagnosis.
Treatment
Pharmacological interventions
Pharmacological interventions are often an integral part of the treatment plan for panic-anxiety disorders. Medications such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed to manage symptoms. Additionally, benzodiazepines may be utilized for short-term relief during severe panic attacks. It is important for the nurse to closely monitor the patient for any potential side effects, drug interactions, and ensure adherence to the prescribed medication regimen.
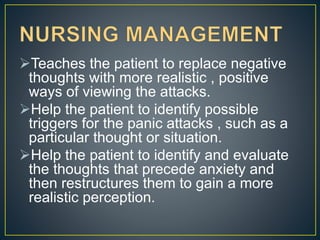
Non-pharmacological interventions
Non-pharmacological interventions play a vital role in the holistic management of panic-anxiety disorders. Cognitive-behavioral therapy (CBT) is a widely recognized and effective approach that helps patients identify and modify negative thought patterns and behaviors associated with anxiety. Relaxation techniques, such as deep breathing exercises and progressive muscle relaxation, can provide patients with powerful tools to manage their anxiety symptoms. Other non-pharmacological interventions may include mindfulness-based stress reduction, yoga, and exercise programs tailored to the individual’s needs.
Education and Support
Psychoeducation
Psychoeducation is an essential component of nursing care for patients with panic-anxiety disorders. It involves providing patients with accurate information about their condition, including its causes, symptoms, and treatment options. Educating patients about the nature of panic attacks and the underlying mechanisms of anxiety can help reduce fear and increase their understanding of the disorder. Furthermore, psychoeducation empowers patients to actively participate in their treatment and make informed decisions about their healthcare.
Support groups
Support groups provide a valuable platform for individuals with panic-anxiety disorders to connect with others who have experienced similar challenges. These groups foster a sense of community, validation, and understanding, which can be immensely beneficial for patients. Nurses can collaborate with mental health professionals to identify and refer patients to local support groups or online communities where they can share their experiences, exchange coping strategies, and receive emotional support.
Emotional Support
Active listening
Active listening is a fundamental skill that nurses can utilize to provide emotional support to patients with panic-anxiety disorders. By actively listening without judgment and reflecting upon the patient’s feelings and concerns, nurses can create a safe and empathetic environment. This approach encourages patients to express their thoughts and emotions openly, fostering a therapeutic nurse-patient relationship. Active listening also allows nurses to gain a deeper understanding of the patient’s individual needs and tailor their care accordingly.
Empathy and understanding
Demonstrating empathy and understanding is crucial when providing emotional support to patients with panic-anxiety disorders. By acknowledging and validating the patient’s feelings, nurses can help alleviate distress and promote a sense of comfort. Offering reassurance and demonstrating empathy through verbal and non-verbal cues can significantly impact the patient’s overall well-being. It is essential for nurses to be patient, compassionate, and non-judgmental, creating a safe space where patients feel heard, understood, and supported.
Safety Measures
Risk assessment
When caring for patients with panic-anxiety disorders, conducting regular risk assessments is essential to identify potential risks and ensure patient safety. Assessing for suicidal ideation, self-harm behaviors, and substance abuse is crucial. Nurses should also evaluate the patient’s home environment for any safety hazards that may exacerbate anxiety symptoms. By proactively identifying and addressing potential risks, healthcare providers can take necessary precautions to minimize harm and optimize patient well-being.
Environmental modifications
Environmental modifications can play a significant role in supporting patients with panic-anxiety disorders. Creating a calming and therapeutic environment can help reduce anxiety triggers and enhance a sense of security. Nurses can adjust lighting, reduce noise levels, and provide a comfortable space for patients to relax. Visual aids and written instructions can assist individuals in feeling more in control of their environment. Collaborating with the multidisciplinary team to implement safety protocols and environmental modifications is crucial for promoting a therapeutic milieu.
Crisis Management
De-escalation techniques
During a crisis or panic attack, de-escalation techniques are essential to help patients regain control and calm their distress. Nurses can employ various strategies such as remaining calm, using a calm and soothing tone of voice, and taking a non-confrontational approach. Providing clear and concise instructions, using grounding techniques, and encouraging deep breathing can help redirect the patient’s focus and reduce anxiety. It is important for nurses to be trained in de-escalation techniques and regularly practice these skills to effectively manage crises.
Emergency protocols
In situations where immediate intervention is necessary, nurses should be familiar with emergency protocols specific to panic-anxiety disorders. This includes knowing the steps to take if the patient becomes physically distressed or experiences severe panic symptoms. Collaborative efforts with the multidisciplinary team, such as psychologists, psychiatrists, and emergency medical services, are critical to ensure a coordinated and timely response to emergencies. Nurses should regularly review and update their knowledge on emergency protocols to provide optimal care in high-stress situations.
Collaboration with Multidisciplinary Team
Psychiatrist
Collaboration with a psychiatrist is essential for the comprehensive management of patients with panic-anxiety disorders. Psychiatrists play a key role in diagnosing and prescribing medications tailored to the individual’s needs. Regular communication with the psychiatrist allows for ongoing evaluation of treatment efficacy and adjustment of medication regimens as necessary. The nurse can provide valuable insights regarding the patient’s response to pharmacological interventions and facilitate effective communication between the patient and psychiatrist.
Therapist
Therapists, such as psychologists or licensed counselors, are integral members of the multidisciplinary team involved in the care of patients with panic-anxiety disorders. Therapists provide evidence-based psychotherapeutic interventions, such as cognitive-behavioral therapy (CBT), to help patients manage their anxiety symptoms. Collaborating with therapists allows for a holistic approach to treatment, addressing both the psychological and emotional aspects of panic-anxiety disorders. Regular communication and interdisciplinary discussions help ensure continuity of care and provide the patient with comprehensive support.
Social worker
Social workers play a crucial role in helping patients navigate various social and financial aspects related to their condition. They can assist with accessing community resources, finding support services, and addressing social determinants of health that may impact the patient’s well-being. Collaborating with social workers can help ensure that patients receive proper support and advocacy in areas such as housing, employment, and health insurance. The nurse can work closely with social workers to develop individualized plans that integrate social support into the patient’s overall treatment approach.
Occupational therapist
Occupational therapists focus on improving the patient’s ability to engage in meaningful activities and regain functional independence. They can assess the patient’s cognitive, physical, and emotional capabilities and develop personalized interventions to promote self-care, work, and leisure participation. Collaboration with occupational therapists allows for a comprehensive approach to treatment, addressing the patient’s overall well-being and quality of life. The nurse can provide valuable input regarding the patient’s progress, challenges, and goals, facilitating a collaborative and cohesive treatment plan.

Documentation and Communication
Accurate and timely documentation
Accurate and timely documentation is crucial in the management of patients with panic-anxiety disorders. Nurses should meticulously record assessment findings, interventions, and the patient’s response to treatment. Documenting changes in symptoms, medication adjustments, and adverse effects allows for comprehensive evaluation and ongoing monitoring of the patient’s progress. Furthermore, clear and concise documentation helps ensure effective communication among members of the healthcare team, promoting continuity of care and patient safety.
Effective communication with healthcare team
Effective communication with the healthcare team is vital in coordinating care for patients with panic-anxiety disorders. Nurses should actively participate in interdisciplinary discussions, sharing relevant information about the patient’s condition, treatment plan, and progress. Regular communication with psychiatrists, therapists, social workers, and occupational therapists allows for collaborative decision-making and ensures the patient receives holistic care. Clear and concise communication helps prevent potential gaps in care, enhances patient outcomes, and promotes a patient-centered approach.
Evaluation
Assessing treatment effectiveness
Regular evaluation of treatment effectiveness is crucial to ensure the patient’s progress and adjust the treatment plan as needed. Nurses should assess the patient’s response to pharmacological interventions, such as the reduction in panic attacks and overall anxiety levels. Additionally, evaluating the patient’s engagement in non-pharmacological interventions, such as therapy attendance and the use of coping strategies, provides valuable insights into treatment efficacy. Through ongoing assessment, healthcare providers can identify areas of improvement and tailor interventions to optimize the patient’s well-being.
Monitoring for adverse effects
While pharmacological interventions can be beneficial, it is essential to closely monitor patients for any potential adverse effects. Nurses should be vigilant for signs of medication side effects, such as sedation, dizziness, or gastrointestinal disturbances. Additionally, assessing for medication non-adherence and monitoring the patient’s overall mental health and well-being is crucial. By regularly monitoring for adverse effects and promptly addressing any concerns, nurses can support the patient’s safety and optimize treatment outcomes.
In conclusion, the nursing considerations for panic-anxiety disorders involve a comprehensive assessment of both the physical and psychosocial aspects of the patient’s well-being. Accurate diagnosis, monitoring of treatment effectiveness, and implementation of pharmacological and non-pharmacological interventions are essential components of nursing care. Additionally, providing education, emotional support, and ensuring patient safety through risk assessment and crisis management are crucial. Collaboration with the multidisciplinary team, effective documentation, and communication contribute to holistic care and continuous evaluation of the patient’s progress. By implementing these nursing considerations, healthcare providers can support individuals with panic-anxiety disorders on their journey towards improved mental health and overall well-being.
