In this article, you will explore the essential nursing considerations and management strategies for patients diagnosed with polyps in the colon. Whether you are a seasoned nurse or just starting your career in the field, understanding the unique care requirements for individuals with this condition is crucial. From potential complications to effective monitoring techniques, this comprehensive guide will equip you with the knowledge and skills needed to provide optimal care and support to these patients. So, let’s dive in and discover how you can make a difference in the lives of those affected by polyps-colon!

Definition of Polyps-Colon
Polyps-Colon, also known as colorectal polyps, are abnormal growths that develop on the inner lining of the colon, or large intestine. These growths can vary in size and shape, ranging from small, flat bumps to larger, mushroom-like structures. While most polyps are benign, meaning they are not cancerous, certain types of polyps have the potential to turn into cancer over time if left untreated. Therefore, it is crucial to identify and remove polyps during diagnostic procedures to prevent the development of colorectal cancer.
Prevalence and Risk Factors
Colorectal polyps are relatively common, with prevalence increasing with age. While anyone can develop polyps, certain risk factors can increase the likelihood of their formation. These risk factors include age over 50, a family history of polyps or colorectal cancer, a personal history of inflammatory bowel disease (such as Crohn’s disease or ulcerative colitis), a sedentary lifestyle, obesity, smoking, and a diet high in fat and low in fiber. Understanding these risk factors can help healthcare providers identify individuals who may be at a higher risk of developing polyps and take appropriate preventive measures.

Signs and Symptoms
In many cases, colorectal polyps do not cause any noticeable symptoms. However, some people may experience rectal bleeding, changes in bowel habits (such as persistent diarrhea or constipation), abdominal pain or cramping, weakness or fatigue, unexplained weight loss, or a feeling of incomplete bowel movement. It is important to note that these symptoms can also be associated with other gastrointestinal conditions, so further investigation is necessary to determine the presence of polyps.
Diagnostic Procedures
When colorectal polyps are suspected, healthcare providers may recommend various diagnostic procedures to confirm their presence and determine their characteristics. These procedures can include nursing assessment, physical examination, laboratory tests, imaging studies, and gastrointestinal endoscopy.
Nursing Assessment
During the nursing assessment, the healthcare provider will gather information about your medical history, including any previous gastrointestinal issues, family history of polyps or colorectal cancer, and current symptoms. They will also ask about your lifestyle habits, such as diet, physical activity level, and tobacco use. This assessment helps to identify potential risk factors and provide a more comprehensive understanding of the patient’s overall health.
Physical Examination
A physical examination may be performed to assess the abdomen for any signs of tenderness, masses, or abnormal bowel sounds. The healthcare provider may also perform a digital rectal examination to feel for any abnormalities in the rectum or lower part of the colon. These examinations can provide important clues about the presence of polyps and help guide further diagnostic procedures.
Laboratory Tests
Laboratory tests, such as complete blood count (CBC) and fecal occult blood test (FOBT), may be ordered to evaluate for any signs of anemia or blood in the stool. While these tests are not specific to polyps, they can help identify any underlying conditions that may be causing the symptoms. Further testing may be necessary to confirm the presence of polyps.
Imaging Studies
Imaging studies, such as computed tomography (CT) scans or magnetic resonance imaging (MRI), may be utilized to visualize the colon and identify any abnormalities or polyps. These non-invasive procedures enable healthcare providers to obtain detailed images of the colon, assisting in the diagnosis and characterization of polyps. The results of these imaging studies can help determine the best course of action for further evaluation or treatment.

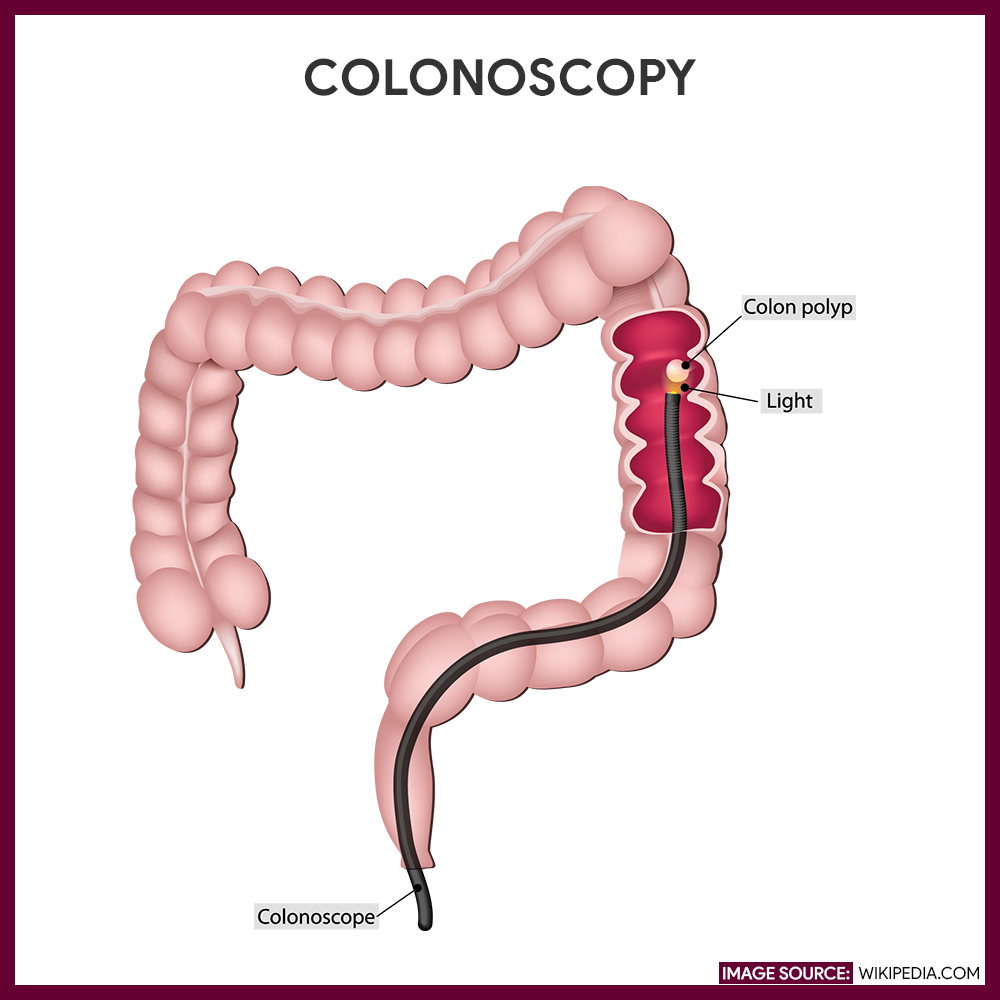
Gastrointestinal Endoscopy
Gastrointestinal endoscopy, specifically colonoscopy, is the gold standard for diagnosing and treating colorectal polyps. During a colonoscopy, a long, flexible tube with a camera at its tip is inserted into the rectum and guided through the colon. This allows the healthcare provider to visualize the entire colon and rectum and to remove any polyps encountered. Colonoscopy is a reliable method for screening, diagnosing, and removing polyps, as it both identifies and treats any detected abnormalities in a single procedure.
Postoperative Care
In cases where polyps are removed during colonoscopy or other surgical procedures, postoperative care is essential for a successful recovery. After the procedure, the patient will be closely monitored for any signs of complications, such as bleeding or infection. Pain management measures will be implemented as needed to ensure the patient’s comfort. It is crucial to provide clear instructions on diet modification, medication usage, and activity restrictions to promote optimal healing and prevent any potential complications.
In conclusion, polyps-colon, or colorectal polyps, are abnormal growths that require careful assessment and monitoring. Through various diagnostic procedures, healthcare providers can determine the presence, characteristics, and potential risk associated with polyps. Nursing considerations, such as thorough assessments, collaboration with other healthcare professionals, and proper postoperative care, play a crucial role in managing patients with polyps-colon. By identifying and addressing polyps early, healthcare providers can help prevent the development of colorectal cancer and improve patient outcomes.