If you have ever wondered about the important role that nurses play in managing spine curvature disorders, then this article is for you. We will explore the various nursing considerations and management techniques that are crucial in ensuring the well-being and comfort of individuals with spine curvature disorders. From assessing pain levels to implementing appropriate interventions, nurses are a vital part of the healthcare team working to improve the quality of life for patients with these conditions. So, let’s dive into the world of nursing considerations for spine curvature disorders!
Assessment and Diagnosis
Patient history
When assessing a patient with spine curvature disorders, it is crucial to obtain a detailed patient history. This includes gathering information about the onset and duration of symptoms, any previous spine surgeries or treatments, and any family history of spine disorders. Additionally, it is important to inquire about any underlying medical conditions or medications that may contribute to the curvature of the spine.
Physical examination
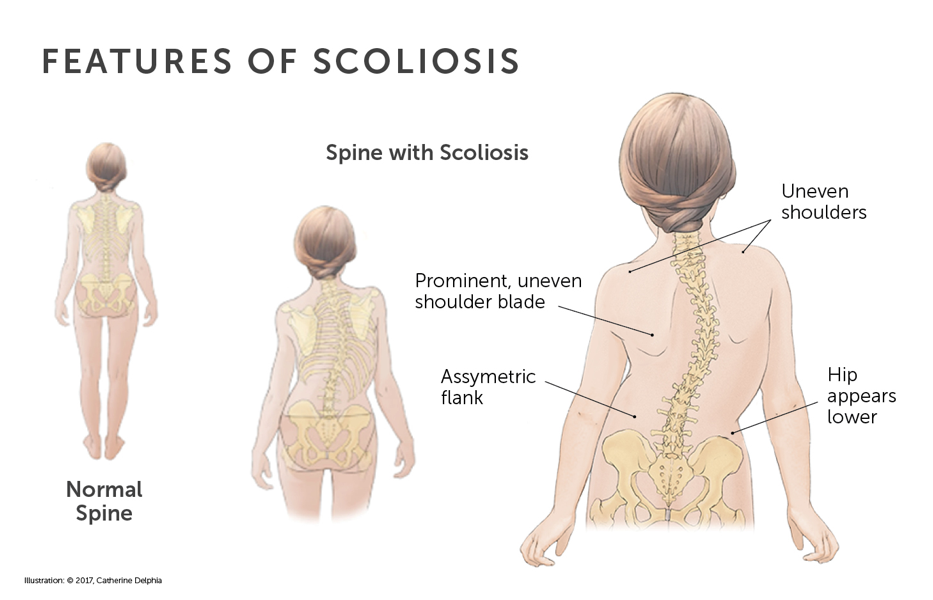
A comprehensive physical examination is essential in the assessment of spine curvature disorders. The healthcare provider will carefully observe the patient’s posture, gait, and range of motion. They will also assess the patient’s spinal alignment, looking for any visible deformities such as an S-shaped curve (scoliosis), hunchback appearance (kyphosis), or exaggerated lower back curvature (lordosis). Furthermore, the provider will palpate the spine to assess for any tenderness, muscle spasms, or signs of neurological deficits.
Radiographic imaging
Radiographic imaging is often utilized to confirm the diagnosis and assess the severity of spine curvature disorders. X-rays, CT scans, and MRIs may be ordered to obtain detailed images of the spine. These imaging modalities can help identify the location, extent, and type of curvature present. By visualizing the spine’s structure, healthcare providers can develop an appropriate treatment plan and monitor the progression of the disorder over time.
Types of Spine Curvature Disorders
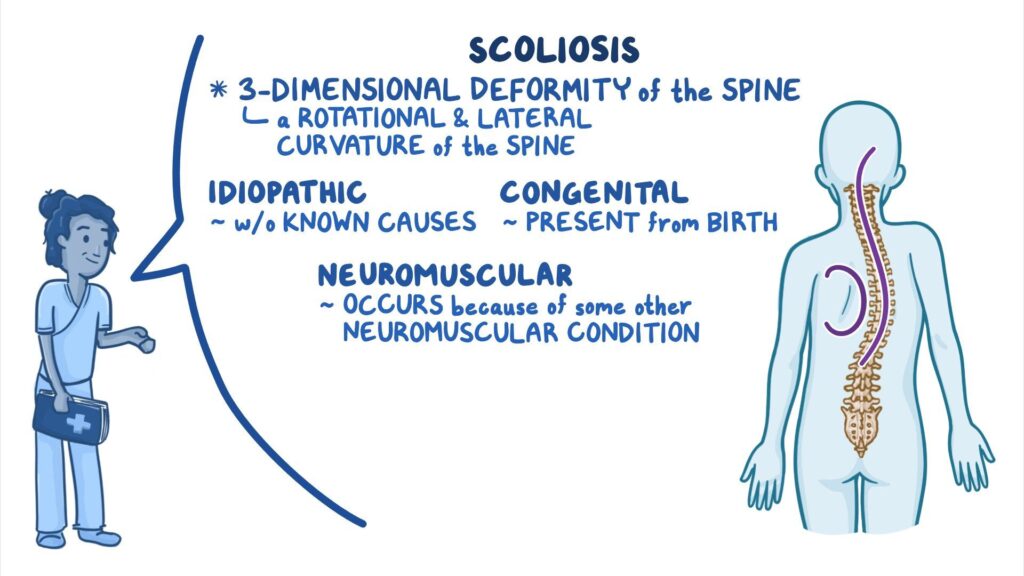
Scoliosis
Scoliosis is a sideways curvature of the spine, resulting in the spine appearing like an ‘S’ or ‘C’ shape when viewed from behind. It is most commonly diagnosed during adolescence, but it can also develop in adults. Scoliosis can cause pain, limited mobility, and changes in appearance. The severity of the curvature can vary, ranging from mild to severe. Treatment options for scoliosis include observation, bracing, and surgery in more severe cases.
Kyphosis
Kyphosis refers to an excessive forward curvature or rounding of the upper back, resulting in a hunched or stooped appearance. It can occur at any age, but it is most commonly seen in older individuals. Kyphosis can lead to pain, difficulty breathing, and reduced mobility. Treatment approaches include physical therapy exercises, pain management, and, in some cases, corrective surgery.
Lordosis
Lordosis refers to an exaggerated inward curvature of the lower back, causing the buttocks to protrude. It can be present at birth or develop later in life due to factors such as poor posture, obesity, or certain medical conditions. Lordosis can cause discomfort, difficulty standing or walking, and limited range of motion. Treatment options for lordosis focus on addressing the underlying cause, such as weight loss, physical therapy, and pain management.
Common Symptoms
Back pain
One of the most prevalent symptoms experienced by individuals with spine curvature disorders is back pain. This pain can range from mild to severe and may be localized to a specific area or radiate to other parts of the body. The pain can be intermittent or constant, and it may worsen with activities or prolonged periods of sitting or standing.
Visible spinal deformity
Spine curvature disorders often result in visible deformities of the spine. These deformities can manifest as an abnormal curvature or misalignment of the spine. In scoliosis, the sideways curvature can be evident when viewing the patient from behind. Kyphosis may cause a noticeable hunchback appearance, while lordosis can result in an exaggerated inward curvature of the lower back.
Limited range of motion
Individuals with spine curvature disorders may experience a limited range of motion in their spine. This can make it challenging to perform daily activities such as bending, twisting, or lifting objects. Range of motion limitations can also impact functional abilities, such as walking, climbing stairs, or getting in and out of bed. Physical therapy and targeted exercises can help improve flexibility and enhance mobility in these cases.
Potential Complications
Respiratory compromise
Severe spine curvature disorders, particularly in the thoracic (upper back) region, can lead to respiratory compromise. The abnormal curvature can restrict lung expansion, impairing the individual’s ability to breathe deeply and efficiently. This may result in shortness of breath, fatigue, decreased exercise tolerance, and an increased risk of respiratory infections. Close monitoring of respiratory function and prompt intervention, such as respiratory therapy or surgical intervention, may be necessary in severe cases.
Cardiac dysfunction
In some instances, spine curvature disorders can also affect cardiac function. Severe curvatures can compress the chest cavity, potentially impacting the positioning and function of the heart. This compression can lead to reduced cardiac output, resulting in symptoms such as palpitations, chest pain, and exercise intolerance. Regular cardiovascular assessments and collaboration with cardiology specialists are essential to ensure the early identification and management of any cardiac dysfunction.
Pain and discomfort
Spine curvature disorders can cause chronic pain and discomfort, significantly affecting an individual’s quality of life. The abnormal alignment of the spine can place excessive pressure on the surrounding muscles, ligaments, and nerves, leading to ongoing pain and discomfort. Nursing interventions, such as administering pain medications and teaching pain management techniques, can help alleviate these symptoms and improve the patient’s overall well-being.
Nursing Interventions
Pain management
Effective pain management is critical in supporting individuals with spine curvature disorders. As nurses, it is essential to assess and monitor the patient’s pain levels regularly. This includes evaluating the intensity, location, and characteristics of the pain. Non-pharmacological interventions, such as heat or cold therapy, massage, and relaxation techniques, can be utilized alongside pharmacological interventions to provide optimal pain relief.
Assistive devices and bracing
Assistive devices and bracing may be recommended for individuals with spine curvature disorders, depending on the severity and type of curvature. Orthotic devices, such as back braces or body jackets, can help support the spine, promote better alignment, and reduce pain. Nurses play a vital role in educating patients on the proper use and care of these devices, as well as monitoring their effectiveness and ensuring compliance.
Promoting mobility and exercise
Maintaining mobility and engaging in appropriate exercise is crucial for individuals with spine curvature disorders. Nurses can assist patients in developing personalized exercise plans tailored to their specific condition and limitations. These exercises may focus on improving posture, strengthening the supporting muscles, and increasing overall flexibility. Regular physical therapy sessions and encouraging daily physical activity can contribute to better functional outcomes and improved quality of life.
Psychosocial Support
Addressing body image concerns
Spine curvature disorders can significantly impact an individual’s body image and self-esteem. Visible deformities may cause feelings of self-consciousness, embarrassment, or isolation. As nurses, providing positive reinforcement and addressing body image concerns can help promote self-acceptance and boost the patient’s self-confidence. Encouraging open communication and offering resources, such as counseling or support groups, can also assist individuals in coping with their body image issues.
Providing emotional support
Caring for individuals with spine curvature disorders involves recognizing and addressing the emotional challenges they may face. Chronic pain, limited mobility, and the potential need for invasive treatments can take a toll on a patient’s emotional well-being. Nurses can provide emotional support by offering a listening ear, validating their feelings, and providing information and education about coping strategies and available resources.
Encouraging participation in support groups
Support groups can be invaluable for individuals with spine curvature disorders and their families. These groups provide a sense of community and a platform for sharing experiences, coping strategies, and emotional support. Nurses can play a pivotal role by identifying and recommending local support groups, both in-person and online. Encouraging patients to participate in these groups can foster a sense of belonging, normalize their experiences, and promote overall psychosocial well-being.
Preventive Measures
Screening and early detection
Early detection and intervention are key in managing spine curvature disorders. Regular screenings during childhood and adolescence can help identify potential abnormalities and ensure prompt referral to specialists if necessary. Additionally, proactive screening in high-risk individuals, such as those with a family history of spine disorders or certain medical conditions, can help identify and address any emerging curvature earlier, potentially preventing complications.
Encouraging proper posture
Promoting proper posture is crucial in preventing the progression of spine curvature disorders. Nurses can educate individuals about the importance of maintaining good posture during daily activities, such as sitting, standing, and lifting. Simple measures, such as using supportive chairs, adjusting workstation ergonomics, and emphasizing the correct alignment of the spine, can help individuals minimize excessive stress on their spine and reduce the risk of developing or worsening curvature.
Educating on ergonomic practices
In addition to promoting proper posture, educating individuals on ergonomic practices can further enhance spine health. This includes teaching individuals how to lift objects correctly using their leg muscles instead of their back, demonstrating proper body mechanics, and providing guidance on appropriate techniques for physical activities. By implementing good ergonomic practices, individuals can reduce the risk of sustaining spinal injuries and minimize strain on their spine.
Collaborative Care
Physical therapy
Physical therapy plays a crucial role in the collaborative care of individuals with spine curvature disorders. Physical therapists work closely with patients to develop customized exercise programs aimed at improving flexibility, strength, and posture. Regular physical therapy sessions can help individuals alleviate pain, enhance mobility, and optimize functional capabilities. Nurses collaborate closely with physical therapy teams, providing ongoing assessments and ensuring seamless communication throughout the patient’s care journey.
Orthopedic consultations
Orthopedic consultations are often warranted for individuals with spine curvature disorders, particularly when surgical intervention or specialized orthotic devices may be necessary. Orthopedic specialists bring expertise in assessing spine deformities, recommending appropriate treatment options, and performing surgical procedures if indicated. Nurses actively facilitate and coordinate orthopedic consultations, ensuring timely access to specialized care and promoting continuity of care across the multidisciplinary team.
Multidisciplinary team approach
The management of spine curvature disorders necessitates a collaborative and multidisciplinary approach. Nurses work alongside numerous healthcare professionals, including orthopedic surgeons, physical therapists, pain specialists, respiratory therapists, and psychologists, to provide holistic care to individuals. The multidisciplinary team collaborates on treatment plans, shares expertise, and ensures seamless communication to optimize patient outcomes and address the various aspects of the patient’s physical, emotional, and psychosocial needs.
Patient Education
Understanding the condition
Patient education is essential in empowering individuals with spine curvature disorders to actively participate in their care. Nurses play a key role in explaining the diagnosis and helping patients understand the underlying cause, progression, and potential complications of their specific condition. By providing accurate and accessible information, nurses can assist patients in making informed decisions regarding their treatment options and self-care strategies.
Self-care and management strategies
Equipping patients with self-care and management strategies is crucial in promoting their well-being and maximizing their quality of life. Nurses can educate individuals on techniques to alleviate pain, such as heat or cold therapy, relaxation techniques, and proper body mechanics. Additionally, they play a vital role in instructing patients on the correct use of assistive devices and braces, ensuring compliance with exercise programs, and teaching self-monitoring techniques to recognize any worsening symptoms promptly.
Recognizing worsening symptoms
Recognizing and promptly addressing any worsening symptoms is crucial in managing spine curvature disorders. Nurses educate patients and their families on signs to be aware of, such as increasing pain, changes in tissue appearance, decreased mobility, or new neurological symptoms. Additionally, nurses emphasize the importance of regular follow-up appointments and maintaining open lines of communication to ensure timely intervention and adjustments to the treatment plan as needed.
Long-Term Management
Regular follow-up appointments
Regular follow-up appointments are an integral part of long-term management for individuals with spine curvature disorders. These appointments allow healthcare providers to monitor the progression of the curvature, assess treatment effectiveness, and address any emerging concerns. Nurses facilitate the scheduling of these appointments, ensuring continuity of care and assisting patients in adhering to their recommended follow-up schedule.
Monitoring progression
Continuous monitoring of the progression of spine curvature disorders is essential to prevent complications and ensure timely intervention. Nurses collaborate with the healthcare team to track any changes in the severity or characteristics of the curvature using radiographic imaging and physical assessments. By closely monitoring the progression, nurses can advocate for appropriate interventions and facilitate effective communication between the patient and the healthcare provider.
Adjusting treatment plan as needed
As spine curvature disorders are dynamic conditions, treatment plans often require adjustments over time. Nurses actively participate in the ongoing evaluation of the patient’s condition, regularly assessing the effectiveness of interventions and evaluating patient outcomes. If necessary, nurses advocate for necessary treatment modifications, such as referral to specialists, recommending alternative pain management strategies, or exploring surgical interventions. By adapting the treatment plan as needed, nurses contribute to optimizing the patient’s health and well-being in the long term.
