When it comes to uterine-cervical cancer, nurses play a vital role in providing care and support to patients. From diagnosis to treatment and beyond, nurses are there every step of the way, ensuring that patients receive the best possible care. This article explores the essential nursing considerations and management strategies for uterine-cervical cancer, highlighting the importance of a compassionate and holistic approach to patient care. By understanding the unique challenges and needs of these patients, nurses can make a significant difference in their journey towards healing and recovery.
Prevention and Screening
Promotion of HPV Vaccination
As a nurse, one of the key responsibilities in preventing and managing uterine-cervical cancer is promoting the importance of HPV vaccination. Human papillomavirus (HPV) is the primary cause of cervical cancer, and the vaccine can significantly reduce the risk of infection. It is crucial to educate patients, parents, and caregivers about the benefits of HPV vaccination and the appropriate age groups for vaccination. By promoting and encouraging HPV vaccination, you can play a vital role in preventing this type of cancer.
Education on Regular Pap Smears
Regular Pap smear screenings are crucial for early detection and prevention of uterine-cervical cancer. It is essential to educate women about the importance of regular Pap smears and the age at which they should start scheduling these screenings. By explaining the purpose and procedure of a Pap smear, you can help alleviate any fears or misconceptions that patients may have. Encourage women to maintain their routine Pap smear appointments and emphasize the importance of early detection in improving treatment outcomes.
Adherence to Recommended Screening Guidelines
As a nurse, it is essential to educate patients on adhering to the recommended screening guidelines for uterine-cervical cancer. These guidelines may vary depending on the patient’s age, medical history, and risk factors. Stress the importance of regular screenings and provide clear instructions on how often they should be scheduled. By ensuring patients understand and follow the screening guidelines, you can contribute to the early detection and effective management of uterine-cervical cancer.
Diagnosis
Understanding Diagnostic Procedures
When a patient is suspected of having uterine-cervical cancer, it is crucial to help them understand the diagnostic procedures involved in confirming the diagnosis. As a nurse, you can explain the purpose and steps of tests such as colposcopy, biopsy, and imaging tests. This will help alleviate any fears or anxiety the patient may have. By ensuring patients have a clear understanding of these procedures, you can help them navigate the diagnostic process with confidence and support.
Assisting in Biopsy
Biopsy plays a crucial role in the diagnosis of uterine-cervical cancer. As a nurse, you may be involved in assisting a physician during biopsy procedures. It is essential to ensure a sterile environment, provide appropriate support and reassurance to the patient, and closely monitor for any signs of complications. You can also educate patients on what to expect during and after the biopsy procedure, including any potential discomfort or side effects. By providing comprehensive care during the biopsy, you can contribute to a smooth and accurate diagnosis process.
Supporting Patients During Imaging Tests
Imaging tests, such as CT scans or MRI scans, are often performed to determine the extent and stage of uterine-cervical cancer. Patients may experience anxiety or claustrophobia during these tests. As a nurse, it is important to provide emotional support and reassurance. Explain the purpose and process of the imaging test, answer any questions, and ensure the patient feels comfortable and safe throughout the procedure. Your support can make a significant difference in the patient’s experience and overall well-being.
Treatment Options
Chemotherapy Administration
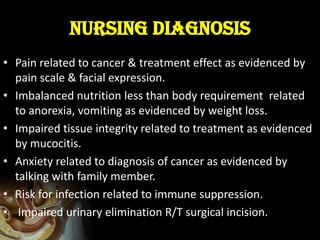
Chemotherapy is a common treatment modality for uterine-cervical cancer. As a nurse, you play a crucial role in administering chemotherapy and monitoring patients for any potential side effects or complications. It is important to understand the medications used, their potential side effects, and the appropriate methods of administration. By closely monitoring patients, providing supportive care, and educating them about possible side effects, you can help minimize discomfort and enhance treatment outcomes.
Radiation Therapy
Radiation therapy is another treatment option for uterine-cervical cancer. Nurses are essential in facilitating and supporting patients undergoing radiation therapy. It is crucial to educate patients about the purpose, process, and potential side effects of radiation therapy. Additionally, you may need to provide care for radiation-induced skin reactions and ensure patients understand proper skin care techniques during treatment. Your knowledge and support can greatly contribute to the patient’s comfort and overall well-being during radiation therapy.
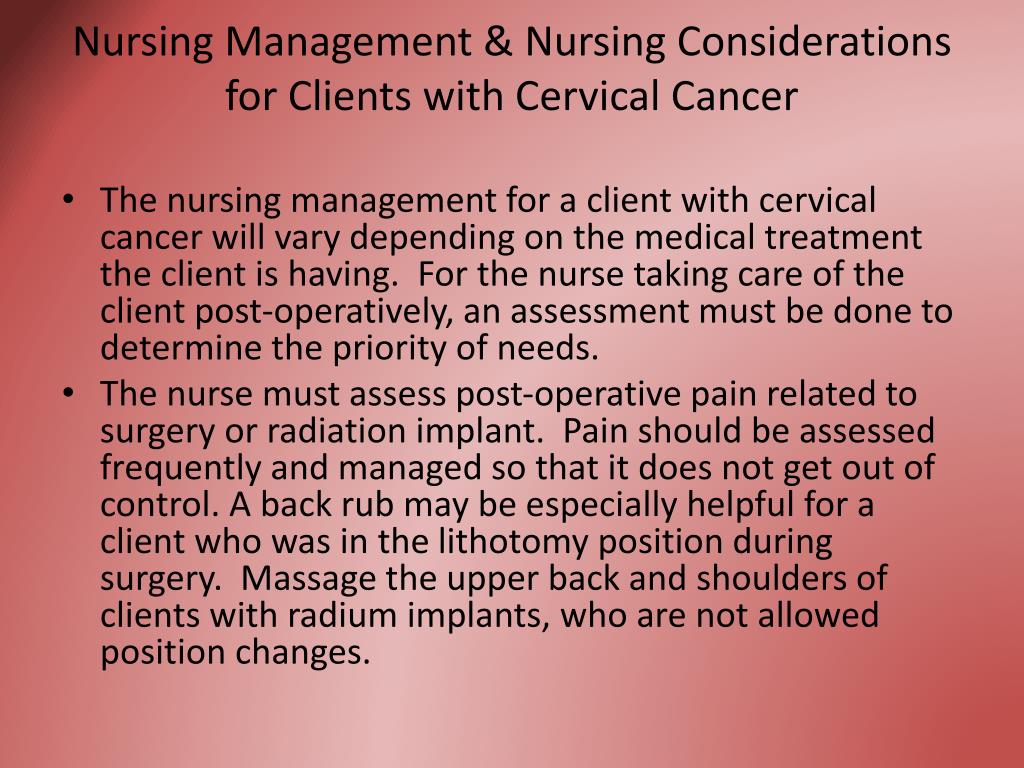
Surgical Interventions
Surgical interventions, such as hysterectomy or lymph node dissection, may be necessary for the treatment of uterine-cervical cancer. As a nurse, you will provide preoperative, intraoperative, and postoperative care to these patients. It is important to educate patients about the surgical procedure, potential complications, and postoperative recovery. Ensure that patients have realistic expectations and provide emotional support during this challenging time. Your comprehensive care can greatly contribute to optimal surgical outcomes and patient satisfaction.
Management of Side Effects
Addressing Nausea and Vomiting
Nausea and vomiting are common side effects of cancer treatments, including chemotherapy and radiation therapy. As a nurse, you can play a vital role in addressing these symptoms. Administering antiemetic medications, providing dietary recommendations, and offering emotional support are key aspects of managing nausea and vomiting. Encourage patients to communicate any discomfort or concerns, and work closely with the healthcare team to adjust medications and interventions as needed. By effectively managing nausea and vomiting, you can enhance the patient’s overall quality of life during treatment.
Managing Fatigue
Fatigue is a significant side effect experienced by many patients undergoing treatment for uterine-cervical cancer. As a nurse, you can help patients manage their fatigue levels and provide strategies for conserving energy. Encourage patients to incorporate regular rest periods into their daily routine, engage in light physical activity, and prioritize self-care activities. It is important to monitor the patient’s energy levels and address any underlying causes of fatigue, such as anemia or poor nutrition. By supporting patients in managing fatigue, you can contribute to their well-being and ability to cope during treatment.
Supporting Sexual Health and Intimacy
Uterine-cervical cancer and its treatments can significantly impact a patient’s sexual health and intimacy. As a nurse, it is important to provide a safe and supportive environment for patients to discuss their concerns and challenges related to sexual well-being. Offer information and resources on sexual health, including potential changes in libido, vaginal dryness, and body image concerns. Refer patients to sexual health specialists or counselors who can provide further guidance and support. By addressing the impact of uterine-cervical cancer on sexual health, you can help patients maintain a fulfilling and intimate relationship with their partners.

Psychosocial Support
Providing Emotional Support
A cancer diagnosis can evoke a range of emotions for patients and their families. As a nurse, providing emotional support is an integral part of your role. Take the time to listen actively, validate feelings, and offer reassurance during patient interactions. Encourage patients to express their fears and concerns openly and provide them with resources for additional support, such as counseling or support groups. By demonstrating empathy and compassion, you can help patients navigate the emotional challenges associated with uterine-cervical cancer.
Assessing Coping Mechanisms
Each patient copes with a cancer diagnosis differently. As a nurse, it is important to assess a patient’s coping mechanisms and provide appropriate support. Some patients may benefit from stress management techniques, such as deep breathing exercises or guided imagery. Others may find solace in engaging with support groups or counseling services. By understanding the individual coping strategies of each patient, you can tailor your support and interventions to meet their specific needs.
Referring to Support Groups or Counseling Services
Support groups and counseling services can be invaluable resources for patients and families affected by uterine-cervical cancer. As a nurse, it is crucial to be aware of local support groups and counseling services and provide referrals as needed. These resources offer a platform for patients to connect with others who share similar experiences and receive professional guidance in managing the emotional impact of cancer. By referring patients to support groups or counseling services, you can help them cultivate a strong support network and find comfort in shared experiences.
Pain Management
Evaluating Pain Levels
Pain is a common concern for patients with uterine-cervical cancer, especially during advanced stages or following surgical interventions. As a nurse, your role in pain management is critical. Start by assessing the patient’s pain levels using appropriate pain assessment tools and ask them to describe the pain they are experiencing. Evaluate both the intensity and quality of the pain, as this information will guide your interventions.
Administering Pain Medications
The administration of pain medications is often a primary intervention in managing pain for patients with uterine-cervical cancer. As a nurse, it is essential to understand and follow the prescribed pain medication regimen, including the appropriate dosage and timing. Regularly assess the patient’s response to pain medications and advocate for adjustments if necessary. Educate patients on the importance of adhering to their pain medication schedule and address any concerns or side effects they may experience.
Exploring Alternative Pain Relief Techniques
In addition to pharmacological interventions, alternative pain relief techniques can be effective in managing pain for patients with uterine-cervical cancer. As a nurse, you can explore non-pharmacological options such as relaxation techniques, massage therapy, acupuncture, or guided imagery. These techniques can provide patients with additional tools to cope with pain and reduce reliance on medication. Collaborate with the healthcare team to develop a holistic pain management plan that incorporates both pharmacological and non-pharmacological approaches.
Nutritional Support
Assessing Nutritional Requirements
Nutritional support is crucial for patients diagnosed with uterine-cervical cancer. As a nurse, you play a vital role in assessing a patient’s nutritional requirements. Evaluate the patient’s nutritional status, including weight, body mass index (BMI), and dietary intake. Collaborate with a registered dietitian to develop a personalized nutrition plan that addresses any specific needs or restrictions. Regularly monitor the patient’s nutritional status and make adjustments as necessary to support optimal health and well-being.
Promoting Adequate Caloric Intake
Weight loss and malnutrition are common concerns for patients with uterine-cervical cancer. It is essential to promote adequate caloric intake to prevent further weight loss and support the body’s healing processes. Encourage patients to consume nutrient-dense foods and provide strategies to manage any treatment-related side effects that may affect appetite or taste. Work closely with the patient and their support system to develop meal plans that are realistic, enjoyable, and meet their individual nutritional needs.
Addressing Malnutrition or Weight Loss
For patients experiencing malnutrition or significant weight loss, additional interventions may be necessary. Collaborate with the healthcare team to address underlying causes of malnutrition, such as gastrointestinal symptoms or treatment-related side effects. Consider nutritional supplements or enteral feeding options if appropriate. It is important to monitor the patient’s progress and adjust interventions as necessary. By addressing malnutrition or weight loss promptly, you can help improve the patient’s overall health and well-being.
Postoperative Care
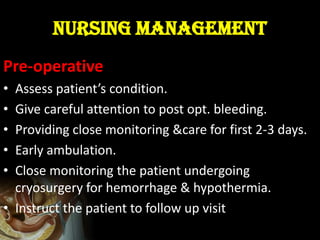
Monitoring Vital Signs
After surgical interventions for uterine-cervical cancer, close monitoring of vital signs is essential to identify any potential complications. As a nurse, you will regularly assess the patient’s blood pressure, heart rate, respiratory rate, and temperature. Monitor for signs of infection, such as fever or increased pain, as well as any other changes in the patient’s condition. Promptly report any abnormalities to the healthcare team to ensure timely interventions and optimal postoperative recovery.
Managing Surgical Incisions
Proper management of surgical incisions is crucial to prevent infections and promote healing. As a nurse, you will assess the incision site regularly for signs of redness, swelling, or drainage. Ensure that the patient understands how to care for their incision at home, including wound cleaning techniques and dressing changes. Provide clear instructions on signs of infection or complications to watch out for and emphasize the importance of following these guidelines. By effectively managing surgical incisions, you can contribute to the patient’s overall recovery and well-being.
Preventing Infection and Complications
Preventing infection and complications is a top priority in postoperative care for patients with uterine-cervical cancer. As a nurse, you will play a critical role in implementing infection control measures and closely monitoring for any signs of infection, such as fever, increased pain, or drainage. Educate the patient and their support system on the importance of hand hygiene, wound care, and proper maintenance of equipment and devices. By diligently following infection prevention protocols and providing thorough patient education, you can help minimize the risk of postoperative complications.
Patient Education
Explaining Treatment Options and Side Effects
Patient education is an integral part of nursing care for uterine-cervical cancer. Take the time to explain the different treatment options available and their potential side effects. Ensure that the patient understands the goals, benefits, and risks associated with each treatment modality. Use clear and simple language, and provide written materials or visual aids to support the patient’s understanding. Encourage patients to ask questions and actively participate in decision-making regarding their treatment.
Providing Information on Self-Care
Self-care plays a vital role in managing uterine-cervical cancer and its treatment. As a nurse, you can provide patients with essential information on self-care practices. Educate patients on maintaining good hygiene, managing treatment-related side effects, and recognizing signs of complications. Offer strategies for managing pain, fatigue, and emotional well-being. By empowering patients with the knowledge and skills to care for themselves, you can enhance their overall quality of life and treatment outcomes.
Encouraging Healthy Lifestyle Choices
Adopting healthy lifestyle choices can have a positive impact on the well-being of patients with uterine-cervical cancer. As a nurse, it is important to encourage patients to make healthy choices in areas such as diet, physical activity, smoking cessation, and stress management. Provide education on the benefits of these lifestyle modifications and offer resources or referrals to support the patient’s efforts. By promoting healthy habits, you can contribute to the patient’s long-term well-being and reduce the risk of cancer recurrence.
End-of-Life Care
Facilitating Advance Care Planning
As a nurse, you may be involved in facilitating advance care planning for patients with uterine-cervical cancer who are approaching end-of-life care. Encourage patients to discuss their wishes and preferences for end-of-life care, including decisions regarding life-sustaining treatments, resuscitation, and hospice care. Provide information on advanced directives and assist patients in documenting their choices. Collaborate with the healthcare team and palliative care specialists to ensure that the patient’s end-of-life wishes are respected and implemented.
Providing Palliative Care
Palliative care focuses on providing relief from symptoms, improving quality of life, and addressing the psychosocial and spiritual aspects of care for patients with uterine-cervical cancer. As a nurse, you will play a vital role in providing compassionate and comprehensive palliative care. This involves managing pain and other distressing symptoms, addressing emotional and spiritual needs, and coordinating care with the healthcare team. By prioritizing palliative care, you can support patients in achieving comfort and dignity during the end-of-life journey.
Supporting Patients and Families
Supporting patients and their families is crucial during the end-of-life care for uterine-cervical cancer. As a nurse, you will provide emotional support, offer guidance on coping strategies, and facilitate communication between patients, families, and the healthcare team. Ensure that patients and families have access to appropriate resources, such as counseling services or support groups, to help them navigate their emotions and find solace in shared experiences. Your compassionate presence and support can make a significant difference in the patient’s and family’s end-of-life experience.
