Living with fibromyalgia can be a challenging and overwhelming experience, as the chronic pain and fatigue can greatly impact your daily life. However, what many people may not realize is that fibromyalgia is often interconnected with mental health issues. In this article, we will take a closer look at the link between fibromyalgia and mental health, exploring how these two conditions can impact each other and offering guidance on how to manage them effectively. Together, let’s navigate the intricate connection between fibromyalgia and mental health, and discover strategies for finding balance and relief.
Understanding Fibromyalgia
Fibromyalgia is a chronic condition that is characterized by widespread pain in the body, along with fatigue, sleep disturbances, and cognitive difficulties. It is estimated to affect around 2-4% of the population, predominantly women. While the exact cause of fibromyalgia is unknown, it is believed to involve a combination of genetic, environmental, and psychological factors. The diagnosis of fibromyalgia is based on a thorough clinical evaluation and the presence of specific criteria, such as widespread pain for at least three months and tenderness at certain points in the body known as tender points.
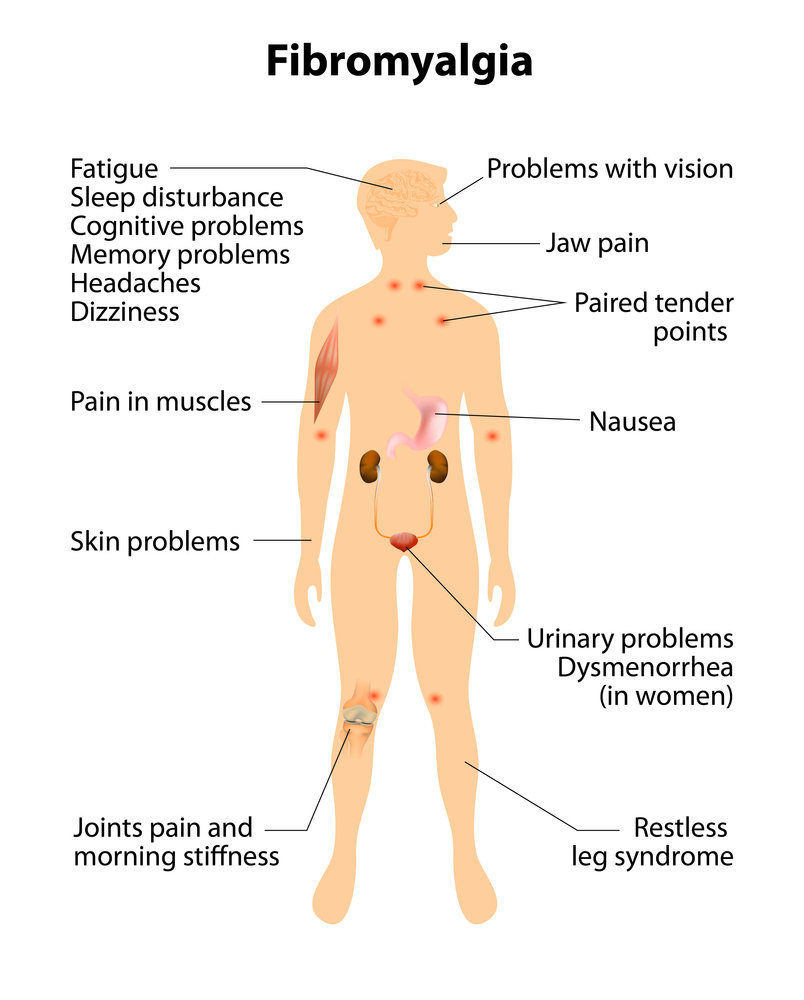
Signs and Symptoms of Fibromyalgia
The signs and symptoms of fibromyalgia can vary from person to person, but the most common symptom is chronic pain that is present throughout the body. This pain is often described as a deep ache, burning sensation, or shooting pain. Other symptoms may include fatigue, sleep disturbances, cognitive difficulties (often referred to as “fibro fog”), headaches, irritable bowel syndrome (IBS), and sensitivity to temperature, light, and sound. These symptoms can significantly impact a person’s daily life and overall well-being.
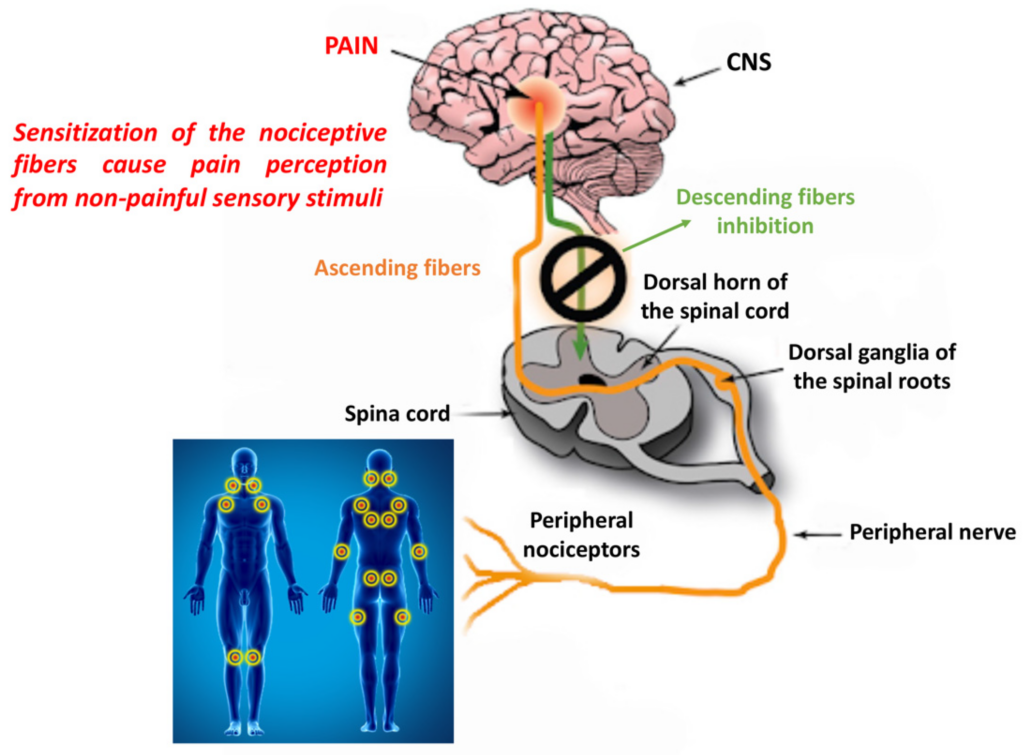
Causes of Fibromyalgia
The exact cause of fibromyalgia is still not fully understood, but research suggests that it may involve a combination of genetic, environmental, and psychological factors. There is evidence to suggest that certain genes may make a person more susceptible to developing fibromyalgia. Environmental factors, such as physical or emotional trauma, infections, or repetitive injuries, may also trigger the onset of fibromyalgia in susceptible individuals. Additionally, psychological factors, such as high levels of stress or a history of abuse, may contribute to the development and exacerbation of fibromyalgia symptoms.
Diagnosis of Fibromyalgia
Diagnosing fibromyalgia can be challenging, as there are no specific tests or imaging studies that can definitively confirm the condition. Instead, the diagnosis is based on a comprehensive clinical evaluation and the presence of specific criteria set by the American College of Rheumatology. These criteria include widespread pain for at least three months and the presence of tenderness at specific points in the body known as tender points. Additional tests may be done to rule out other potential causes of the symptoms, such as blood tests, imaging studies, or sleep studies.
The Prevalence of Mental Health Issues in Fibromyalgia Patients
Fibromyalgia is often comorbid with various mental health disorders, with studies suggesting that up to 70% of fibromyalgia patients meet the criteria for at least one psychiatric disorder. It is important to recognize and address these mental health issues as they can significantly impact a person’s quality of life and treatment outcomes.
Mental Health Disorders commonly associated with Fibromyalgia
Depression, anxiety, and post-traumatic stress disorder (PTSD) are some of the most common mental health disorders associated with fibromyalgia. Depression is characterized by persistent feelings of sadness, worthlessness, and a loss of interest in activities. Anxiety refers to excessive worry, restlessness, and a sense of impending doom. PTSD occurs as a result of experiencing or witnessing a traumatic event, leading to symptoms such as intrusive thoughts, nightmares, and hypervigilance.
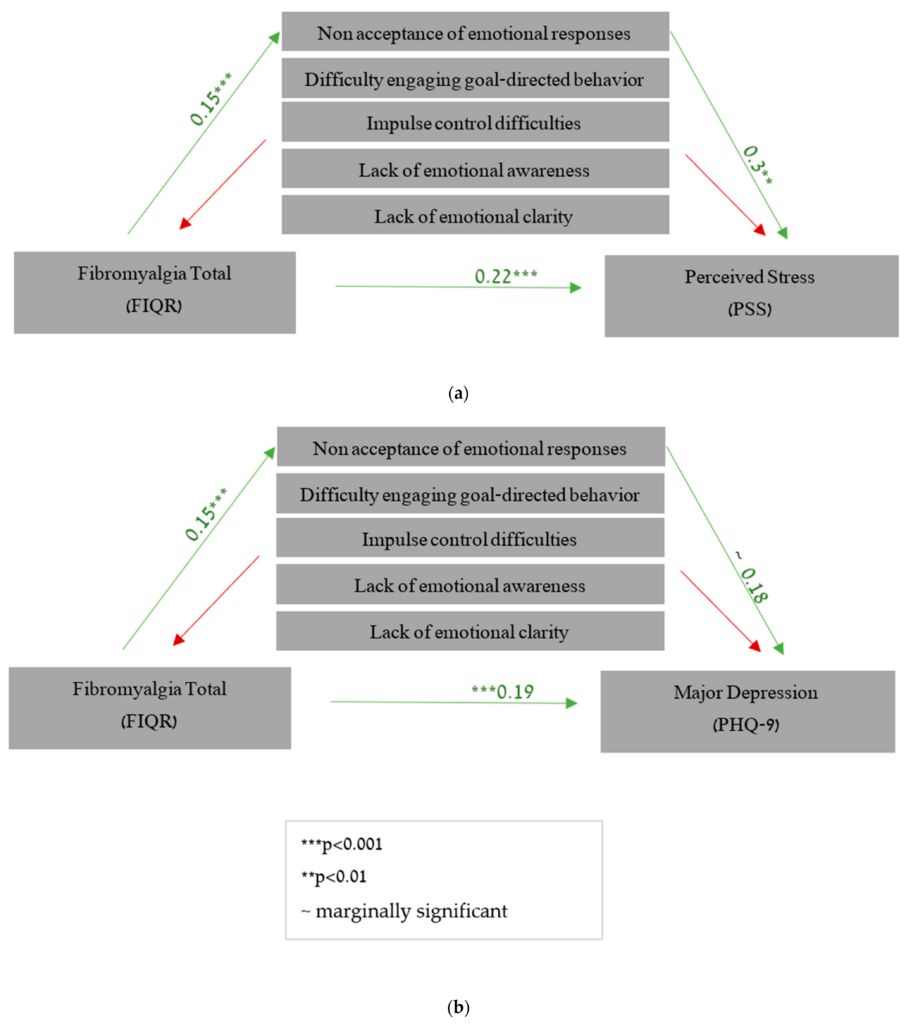
Depression and Fibromyalgia
Depression and fibromyalgia often go hand in hand, with studies showing a bidirectional relationship between the two conditions. Chronic pain and other physical symptoms of fibromyalgia can contribute to the development or worsening of depression, while depression can amplify pain perception and interfere with the management of fibromyalgia symptoms. It is essential for healthcare professionals to screen for and address depression in fibromyalgia patients to ensure optimal treatment outcomes.
Anxiety and Fibromyalgia
Anxiety is another mental health disorder commonly seen in individuals with fibromyalgia. The chronic pain, uncertainty, and sleep disturbances associated with fibromyalgia can lead to increased levels of anxiety. Conversely, anxiety can exacerbate pain perception and potentially impact treatment adherence. Managing anxiety in fibromyalgia patients is crucial to improve overall well-being and reduce the impact of the condition on daily life.
Post-Traumatic Stress Disorder (PTSD) and Fibromyalgia
PTSD can also coexist with fibromyalgia, particularly in individuals who have experienced trauma, such as physical or sexual abuse. The symptoms of PTSD, including intrusive thoughts, flashbacks, and hypervigilance, can further exacerbate the pain and other symptoms experienced by fibromyalgia patients. A comprehensive approach that addresses both the fibromyalgia symptoms and PTSD is necessary to improve the overall well-being of these individuals.
The Bidirectional Relationship Between Fibromyalgia and Mental Health
The relationship between fibromyalgia and mental health is complex and bidirectional, with each influencing the other in multiple ways. Understanding this relationship is crucial in developing effective treatment approaches for individuals with comorbid fibromyalgia and mental health disorders.
Effects of Fibromyalgia on Mental Health
Living with fibromyalgia can have a significant impact on a person’s mental health. The chronic pain, fatigue, and other symptoms associated with fibromyalgia can lead to frustration, sadness, and a sense of helplessness. These feelings can contribute to the development of mental health disorders such as depression and anxiety. Furthermore, the limitations imposed by fibromyalgia can affect a person’s social and occupational functioning, leading to feelings of isolation and low self-esteem.
Effects of Mental Health on Fibromyalgia
Mental health disorders can also have a profound effect on fibromyalgia symptoms and treatment outcomes. The emotional and psychological factors associated with mental health disorders can amplify pain perception and make it more challenging for individuals to cope with their fibromyalgia symptoms. Additionally, mental health disorders can interfere with the adherence to treatment plans, leading to poorer outcomes and decreased quality of life.
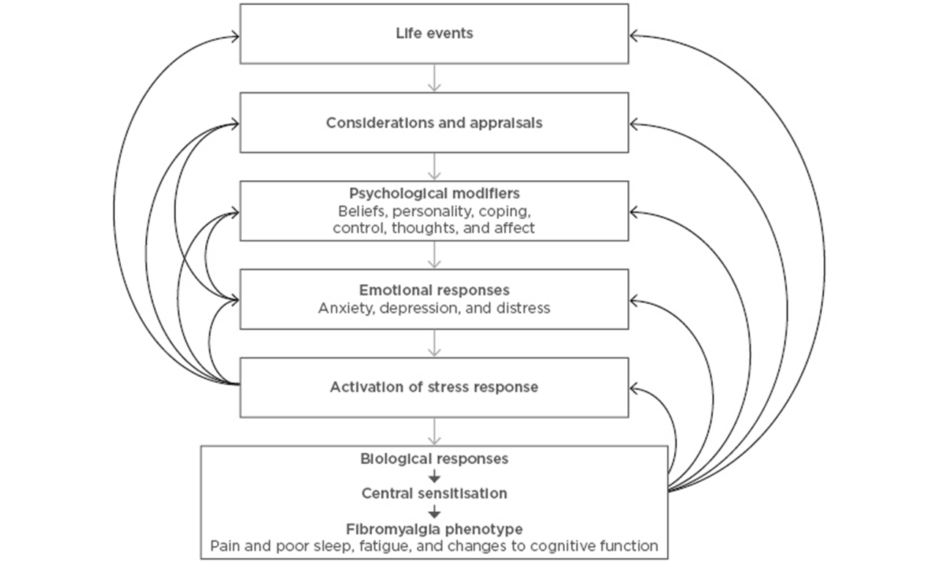
Shared Risk Factors and Biological Pathways
There are several shared risk factors and biological pathways that may contribute to the bidirectional relationship between fibromyalgia and mental health disorders. Some of these include alterations in the stress response system, neurotransmitter imbalances, immune system dysfunction, and genetic factors. Research into these shared mechanisms can help inform the development of targeted treatments that address both the physical and mental aspects of fibromyalgia.
Psychosocial Factors and Fibromyalgia
Psychosocial factors, such as stress, trauma, and social support, can also play a significant role in the development and progression of fibromyalgia and its relationship with mental health. High levels of stress and a history of trauma have been associated with an increased risk of developing fibromyalgia and mental health disorders. On the other hand, having a strong social support network can help individuals cope with the challenges posed by fibromyalgia and improve their overall well-being.
Implications for Treatment
Treating fibromyalgia and the associated mental health disorders requires an integrated and multidisciplinary approach that addresses both the physical and emotional aspects of the condition.
Integrated Approach in Treating Fibromyalgia and Mental Health
An integrated approach involves collaboration between healthcare professionals from different specialties, including rheumatology, psychiatry, and psychology. This teamwork allows for comprehensive assessment, identification of shared goals, and the development of individualized treatment plans that address both the fibromyalgia symptoms and mental health disorders.
Pharmacological Treatments for Fibromyalgia and Mental Health
Pharmacological treatments are commonly used to manage both fibromyalgia and mental health disorders. Medications such as antidepressants, anticonvulsants, and muscle relaxants may be prescribed to alleviate pain, improve sleep, and regulate mood. It is important to closely monitor the effects and side effects of these medications and adjust the treatment plan accordingly.
Psychological Therapies for Fibromyalgia and Mental Health
Psychological therapies, such as cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR), have shown promise in managing fibromyalgia symptoms and improving mental health outcomes. These therapies can help individuals develop coping strategies, challenge negative thoughts, and improve overall well-being. Seeking the help of qualified therapists experienced in treating fibromyalgia and mental health can be beneficial.
Self-Care Strategies and Lifestyle Modifications
Self-care strategies and lifestyle modifications play a crucial role in managing fibromyalgia and supporting mental health. Regular exercise, proper nutrition, adequate sleep, stress reduction techniques, and establishing a support network are all essential components of a self-care plan. Additionally, individuals should be encouraged to engage in activities they enjoy and prioritize their mental and emotional well-being.
The Role of Healthcare Professionals
Healthcare professionals have a vital role to play in recognizing, understanding, and addressing the complex relationship between fibromyalgia and mental health.
Awareness and Education for Healthcare Professionals
Healthcare professionals need to be educated about the connection between fibromyalgia and mental health to ensure accurate diagnosis, appropriate treatment, and effective management. Continuing education programs and professional conferences can provide valuable information and resources to improve the care provided to individuals with comorbid fibromyalgia and mental health disorders.
Collaborative Care for Comorbid Fibromyalgia and Mental Health Disorders
Collaborative care models involving multiple healthcare professionals, including rheumatologists, psychiatrists, psychologists, and primary care physicians, can help ensure a comprehensive and coordinated approach to treating fibromyalgia and mental health disorders. Clear communication, shared treatment goals, and regular follow-up are essential components of collaborative care.
Screening and Assessing Mental Health in Fibromyalgia Patients
Screening and assessing mental health in fibromyalgia patients should be a routine part of the diagnostic process and ongoing management. Validated screening tools and assessments can help identify the presence and severity of mental health disorders, enabling appropriate interventions and treatment plans to be implemented.
Referral and Access to Specialists
Referral and access to specialists, such as rheumatologists, psychiatrists, psychologists, and pain management experts, are essential for individuals with comorbid fibromyalgia and mental health disorders. Timely access to these specialists can help optimize treatment outcomes and improve the overall well-being of the patient.
Support and Resources for Those Affected
Support groups, psychoeducation programs, advocacy organizations, and online resources can provide valuable support and resources for individuals affected by fibromyalgia and mental health disorders.
Support Groups and Peer Networks
Support groups and peer networks allow individuals to connect with others who share similar experiences, providing a sense of validation, support, and understanding. These groups can offer emotional support, practical advice, and a safe space to share struggles and triumphs.
Psychoeducation and Self-Management Programs
Psychoeducation programs provide individuals with knowledge and information about fibromyalgia and mental health disorders, helping them understand their condition better and develop self-management skills. These programs may include workshops, educational materials, and resources that empower individuals to take an active role in their treatment and improve their overall well-being.
Advocacy Organizations for Fibromyalgia and Mental Health
Advocacy organizations play a significant role in raising awareness, providing resources, and advocating for the needs of individuals affected by fibromyalgia and mental health disorders. These organizations often offer support, education, and opportunities for individuals to get involved and make a difference in their communities.
Online Resources and Information
Online resources, such as websites, forums, and educational materials, can provide valuable information, support, and resources for individuals affected by fibromyalgia and mental health disorders. These resources can help individuals stay connected, access up-to-date information, and find additional support when needed.
Future Directions in Research
While significant progress has been made in understanding the link between fibromyalgia and mental health, there is still much to learn. Future research should focus on unraveling the underlying mechanisms, developing targeted interventions, conducting longitudinal studies to track treatment outcomes, and improving access to care for individuals with fibromyalgia and mental health disorders.
Unraveling the Underlying Mechanisms
Further research is needed to better understand the underlying mechanisms that contribute to the bidirectional relationship between fibromyalgia and mental health disorders. This includes exploring shared biological pathways, genetic factors, and psychosocial factors that may influence the development and progression of both conditions.
Developing Targeted Interventions
Targeted interventions that address both the physical and mental aspects of fibromyalgia and mental health disorders can significantly improve treatment outcomes. Future research should focus on developing and testing interventions that target shared risk factors, biological mechanisms, and psychosocial factors.
Longitudinal Studies and Treatment Outcomes
Longitudinal studies that track individuals with comorbid fibromyalgia and mental health disorders over time can provide valuable insights into treatment outcomes and the long-term impact of these conditions. Understanding the trajectory of these conditions can help inform the development of personalized treatment plans and interventions.
Improving Access to Care
Improving access to care for individuals with comorbid fibromyalgia and mental health disorders is crucial. This includes increasing awareness among healthcare professionals, reducing barriers to specialist referrals, and ensuring adequate resources and support are available for these individuals. By improving access to care, we can enhance treatment outcomes and improve the overall well-being of those affected by fibromyalgia and mental health disorders.