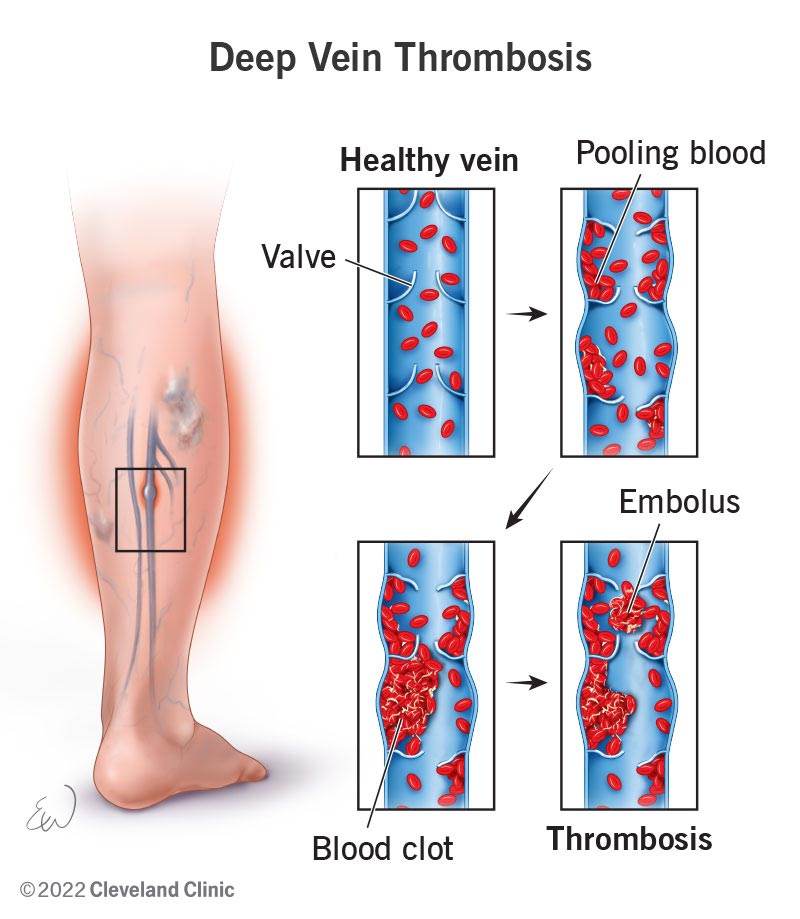
When it comes to taking care of your health, it’s essential to be well-informed about conditions like Deep Vein Thrombosis (DVT) and the available treatments. DVT occurs when a blood clot forms in a deep vein, usually in the leg. While it can be a serious condition, there are effective methods to treat and manage it. This article will explore some of the treatment options for DVT, providing you with valuable information to ensure you can make informed decisions about your health. So, let’s dive right in and discover the best ways to tackle Deep Vein Thrombosis together!
Prevention and Risk Factors
Preventing DVT
When it comes to preventing deep vein thrombosis (DVT), there are several measures you can take to reduce your risk. Regular physical activity, such as walking or stretching, can help promote blood circulation and prevent blood from pooling in your veins. If you have a sedentary lifestyle or are prone to sitting for long periods, make sure to take breaks and move around every hour or so.
Maintaining a healthy weight is also important in preventing DVT. Obesity can increase your risk, so it’s essential to eat a balanced diet and engage in regular exercise to stay within a healthy weight range. Additionally, avoid smoking and excessive alcohol consumption, as they can both contribute to the development of blood clots.
Risk Factors for DVT
Certain factors can increase your risk of developing DVT. These include:
- Prolonged immobility, such as being bedridden or sitting for long periods during travel
- Recent surgery, especially involving the lower extremities or abdomen
- Hormonal changes, such as pregnancy, birth control pills, or hormone replacement therapy
- Chronic medical conditions, like cancer, heart disease, or inflammatory bowel disease
- Family or personal history of blood clots
- Advanced age
- Obesity
- Inherited blood clotting disorders
If you have one or more of these risk factors, it’s important to be vigilant and take preventive measures to reduce your chances of developing DVT.
Diagnosis
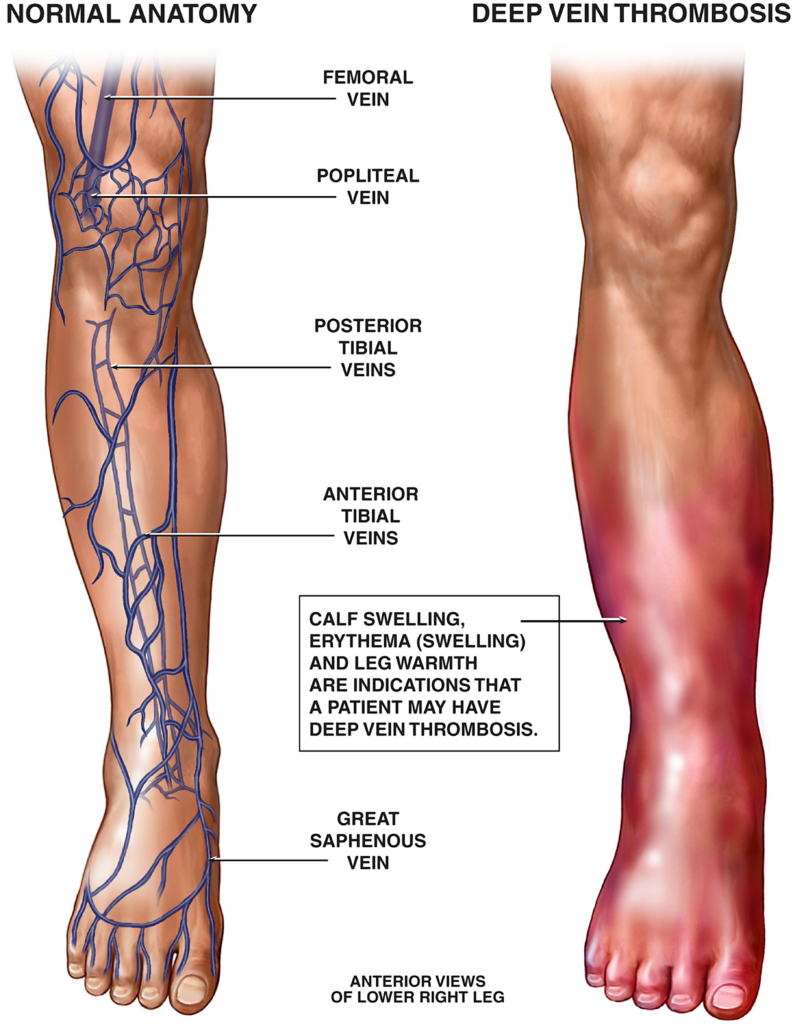
Symptoms of DVT
Detecting DVT early is crucial for successful treatment. Be aware of the following symptoms and seek medical attention if you experience them:
- Swelling in the affected leg, ankle, or foot
- Pain or tenderness, often in the calf or thigh
- Warmth and redness over the affected area
- Skin discoloration, such as bluish or reddish tint
It’s important to note that not everyone with DVT experiences noticeable symptoms. If you’re at high risk due to surgery or other factors, consult your doctor about screening tests.
Physical Examination
During a physical examination, your healthcare provider will assess your symptoms and examine the affected limb. They will check for swelling, tenderness, and areas of warmth or redness. The examination may include measuring the circumference of your legs to compare any size differences between limbs, indicating possible DVT.
Diagnostic Tests
To confirm the presence of DVT, your doctor may recommend certain diagnostic tests. These tests can include:
- Duplex ultrasound: This non-invasive test uses sound waves to visualize blood flow and identify any clots or blockages in the veins.
- D-dimer blood test: This test measures a substance released when a blood clot breaks up. While a positive result doesn’t confirm DVT, a negative result can help rule it out.
- Venography: This invasive procedure involves injecting a contrast dye into your vein to visualize blood flow. It’s typically reserved for cases where other tests provide inconclusive results.
A proper diagnosis is essential to determine the most effective treatment plan for your DVT.
Medical Treatment
Anticoagulant Medications
The mainstay of medical treatment for DVT is anticoagulant medication, often referred to as blood thinners. These medications prevent new blood clots from forming and help existing clots dissolve over time. They don’t actually thin the blood but rather slow down its ability to clot.
Commonly prescribed anticoagulant medications include:
- Heparin: Usually administered through injection, it rapidly prevents clotting and is often used in hospital settings.
- Warfarin: Taken orally, it helps prevent future blood clots but takes time to reach its full effect. Regular monitoring of blood clotting levels is necessary while on warfarin.
- Direct oral anticoagulants (DOACs): These newer medications, such as rivaroxaban and apixaban, offer more convenient dosing and require less frequent monitoring.
The specific type of anticoagulant and duration of treatment will depend on the severity and location of your DVT, as well as any underlying medical conditions.
Thrombolytic Therapy
In certain cases of severe DVT or when there’s a risk of the clot traveling to the lungs, your doctor may recommend thrombolytic therapy. This treatment involves the administration of medications that rapidly dissolve blood clots. Thrombolytic therapy is typically reserved for emergency situations or when other treatments have not been effective.
Compression Stockings
Compression stockings are specially designed stockings that help improve blood flow in the legs and reduce the risk of DVT. They apply pressure to the lower limbs, promoting the circulation of blood back towards the heart. Compression stockings are commonly used both as a preventive measure and during the treatment of DVT. Your doctor will advise you on the appropriate type and fit for your condition.
Surgical Treatment
Thrombectomy
Thrombectomy is a surgical procedure performed to remove a blood clot from a vein. It’s usually considered when the clot is causing severe symptoms, fails to respond to other treatments, or poses a high risk of complications. During the procedure, a surgeon creates an incision near the clot and physically removes it from the vein, restoring normal blood flow.
Inferior Vena Cava Filters
Inferior vena cava (IVC) filters are small, cone-shaped devices inserted into the inferior vena cava, the large vein that carries deoxygenated blood from the lower body to the heart. These filters act as a barrier, catching blood clots before they can reach the lungs, potentially preventing a life-threatening condition called pulmonary embolism. IVC filters may be considered if anticoagulant medications aren’t suitable or effective for a patient.

Home and Self-Care Treatments
Elevating the Affected Limb
Elevating the affected limb above the level of your heart can help reduce swelling and improve blood circulation. Try to elevate your leg whenever you’re resting or sleeping, using pillows or a cushion.
Applying Heat or Cold
Applying heat or cold to the affected area can provide temporary relief and help reduce swelling and pain. Use a heating pad or take warm baths for soothing heat therapy, or apply ice packs wrapped in a cloth for cold therapy. Be sure to follow your doctor’s recommendations regarding the appropriate temperature and duration.
Wearing Compression Stockings
As mentioned earlier, compression stockings promote blood circulation and reduce the risk of DVT. If prescribed by your doctor, wear the stockings as directed and make sure they fit properly to maximize their effectiveness.
Exercising and Staying Active
Regular exercise and staying physically active is essential for preventing complications of DVT. Engage in activities that promote blood flow, such as walking, swimming, or cycling. However, it’s crucial to consult your healthcare provider before starting any exercise regimen to ensure it’s safe for your specific situation.
Complications and Management
Post-Thrombotic Syndrome
Post-thrombotic syndrome (PTS) is a potential long-term complication of DVT that can cause chronic pain, swelling, and skin changes in the affected limb. To manage PTS, treatments such as compression therapy, elevation, and pain management techniques may be utilized. Adhering to preventive measures and seeking early treatment for DVT can help reduce the risk of developing PTS.
Pulmonary Embolism
One of the most severe complications of DVT is a pulmonary embolism (PE), which occurs when a blood clot breaks off and travels to the lungs. It can be life-threatening and requires immediate medical attention. If you experience sudden shortness of breath, chest pain, or cough up blood, call emergency services immediately.
Preventing Recurrence
If you’ve had a DVT, you’re at an increased risk of recurrence. To prevent future episodes, it’s important to follow any long-term treatment plans prescribed by your doctor. This may include taking anticoagulant medications for an extended period or making lifestyle modifications to reduce risk factors.
Alternative and Complementary Treatments
Natural Supplements
While natural supplements may be marketed as alternatives to medical treatment, it’s crucial to consult your healthcare provider before using them. Some supplements, such as fish oil or garlic, may have blood-thinning properties and can interact with anticoagulant medications, increasing the risk of bleeding. Your doctor can provide specific guidance on any supplements that are safe and appropriate for you.
Herbal Remedies
Similar to natural supplements, many herbal remedies have potential medicinal properties but can also interact with medications or have unintended side effects. It’s important to discuss the use of herbal remedies with your healthcare provider to ensure they won’t interfere with your DVT treatment plan.
Acupuncture
Acupuncture is a traditional Chinese therapy that involves the insertion of thin needles into specific points on the body. While some studies suggest it may help with pain management and circulation, more research is needed to determine its effectiveness specifically for DVT. If you’re interested in trying acupuncture, consult a qualified practitioner experienced in treating circulatory disorders.
Lifestyle Changes
Healthy Diet
Adopting a healthy diet can play a significant role in managing and preventing DVT. Focus on consuming a variety of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products. Limit your intake of processed foods, sugary snacks, and foods high in saturated fats. Maintaining a balanced diet can help control weight, blood pressure, and cholesterol levels, reducing the risk of DVT.
Weight Management
Maintaining a healthy weight is important for overall cardiovascular health, including the prevention of DVT. If you’re overweight or obese, work with your healthcare provider to develop a safe and effective weight loss plan. This may involve dietary changes, regular exercise, and, in some cases, additional support such as counseling or a weight management program.
Smoking Cessation
Smoking damages blood vessels and increases the risk of blood clots, making it a particularly risky habit for individuals with DVT. If you’re a smoker, quitting is one of the best things you can do to improve your overall health and reduce the risk of future thrombotic events. Seek support from your healthcare provider, consider nicotine replacement therapies, or join a smoking cessation program to increase your chances of success.
Psychological Support
Coping with DVT
Being diagnosed with DVT can be overwhelming and emotionally challenging. It’s normal to experience feelings of anxiety, fear, or frustration. Remember that you are not alone, and there are resources available to help you cope. Reach out to your healthcare team, friends, and family for support. They can provide guidance, reassurance, and understanding during this time.
Support Groups
Joining a support group for individuals with DVT can offer a valuable network of shared experiences and insights. Connecting with others who have gone through similar experiences can provide a sense of community, emotional support, and practical tips for coping with the challenges of living with DVT. Your healthcare provider may be able to recommend local or online support groups.
Mental Health Counseling
If you find that your emotional well-being is significantly impacted by your DVT diagnosis or treatment, seeking professional mental health counseling can be beneficial. A therapist or counselor can help you process your feelings, develop coping strategies, and provide support as you navigate the challenges of managing DVT.
Implications for Pregnancy
Anticoagulant Considerations
Pregnancy increases the risk of DVT due to hormonal changes and decreased mobility. However, treating DVT in pregnant individuals requires careful consideration of the potential risks to both the mother and the developing baby. Anticoagulant medications, such as heparin, are often preferred over oral blood thinners during pregnancy.
If you’re pregnant or planning to become pregnant and have a history of DVT or other risk factors, consult a healthcare provider with expertise in managing DVT in pregnancy. They will work with you to develop an appropriate treatment plan that balances the benefits of anticoagulant therapy with the potential risks.
Monitoring and Management during Pregnancy
Pregnant individuals with a history of DVT may require additional monitoring and management throughout their pregnancy. This may include regular ultrasounds to check for blood clots, adjustments to anticoagulant medication dosages, and close collaboration between obstetricians and hematologists. It’s crucial to follow your healthcare provider’s recommendations and attend all scheduled prenatal appointments to ensure the best possible outcomes for both you and your baby.
In conclusion, deep vein thrombosis is a serious condition that requires prompt diagnosis and appropriate treatment to prevent complications. By understanding the prevention measures, recognizing the symptoms, and seeking medical attention, you can effectively manage DVT. Remember to work closely with your healthcare provider and follow their guidance to minimize the risk of recurrence and ensure optimal health and well-being.