Have you ever heard of Deep Vein Thrombosis? If not, don’t worry, because in this article we will help you understand what it is and why it is important to be aware of it. Deep Vein Thrombosis, or DVT, is a condition in which blood clots form in the deep veins of the body, most commonly in the legs. These clots can be dangerous as they have the potential to travel to the lungs and cause a life-threatening condition known as pulmonary embolism. By gaining a better understanding of DVT, you can take steps to prevent it and ensure your overall well-being.
Overview of Deep Vein Thrombosis
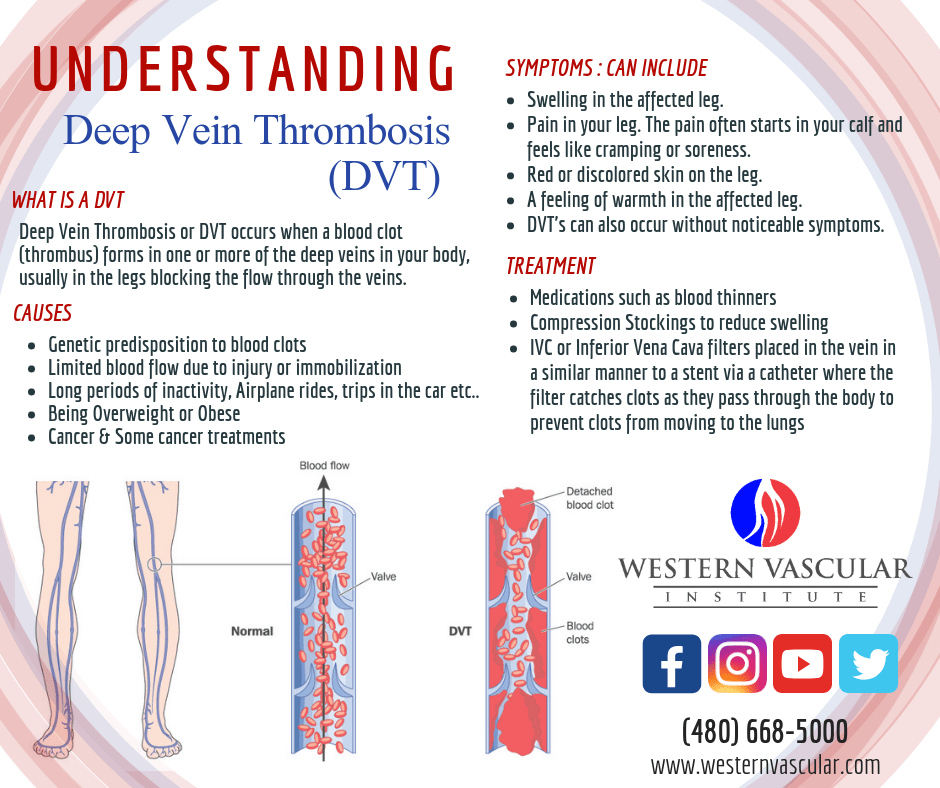
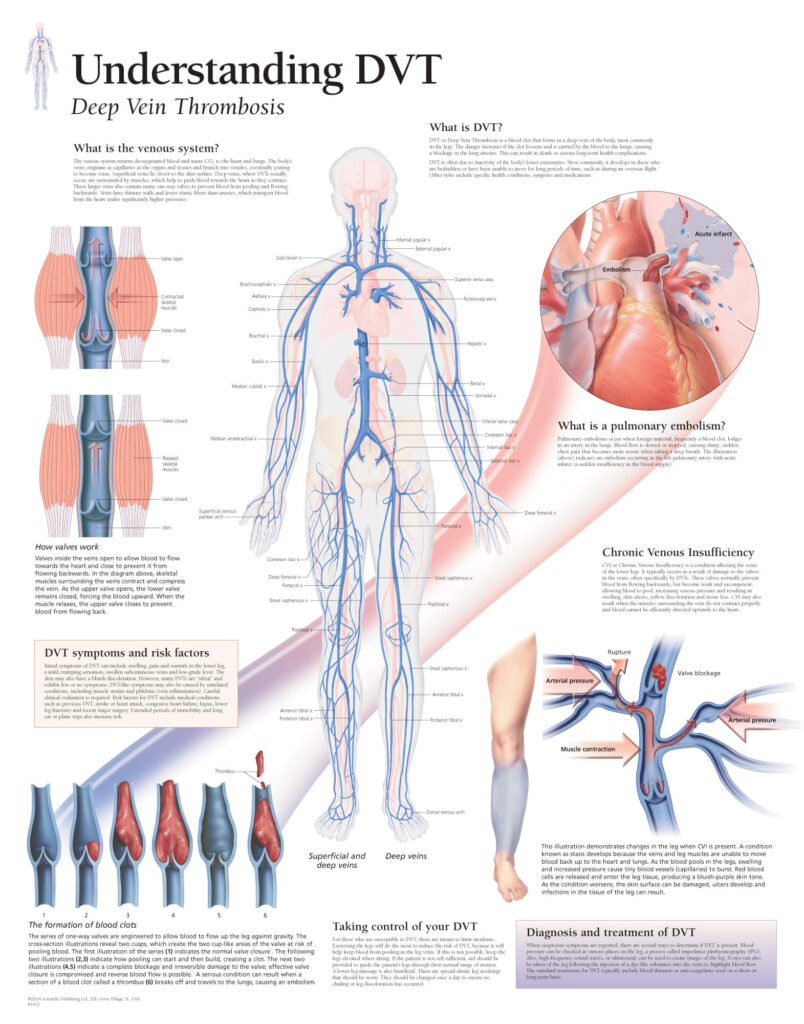
Deep Vein Thrombosis (DVT) is a medical condition that occurs when a blood clot forms in a deep vein, usually in the lower leg or thigh. This condition can be quite serious as it can lead to complications such as pulmonary embolism, where the blood clot breaks free and travels to the lungs. DVT affects millions of people around the world and can have long-term consequences if not properly diagnosed and treated.
Definition and Description
Deep Vein Thrombosis (DVT) refers to the formation of blood clots in the deep veins, typically in the lower extremities. The veins affected are those that lie deep within the muscles. These blood clots can restrict blood flow, causing pain, swelling, and potentially further health complications. If left untreated, DVT can lead to pulmonary embolism, where the clot dislodges and travels to the lungs, causing serious health risks.
Prevalence and Incidence
DVT is a relatively common condition that affects millions of people worldwide each year. The incidence of DVT increases with age, with older individuals being more susceptible to developing blood clots. Certain risk factors, such as a sedentary lifestyle, obesity, and pregnancy, can also increase the likelihood of developing DVT. It is important to be aware of these risk factors and take appropriate measures to prevent the condition.
Risk Factors
Several factors contribute to the development of DVT. Sedentary behavior, such as prolonged periods of sitting or lying down, increases the risk of blood clot formation. Obesity, smoking, and hormonal changes during pregnancy or the use of birth control pills can also increase the likelihood of developing DVT. Additionally, individuals with a personal or family history of blood clotting disorders are at a higher risk. Understanding these risk factors can help individuals take preventive measures.
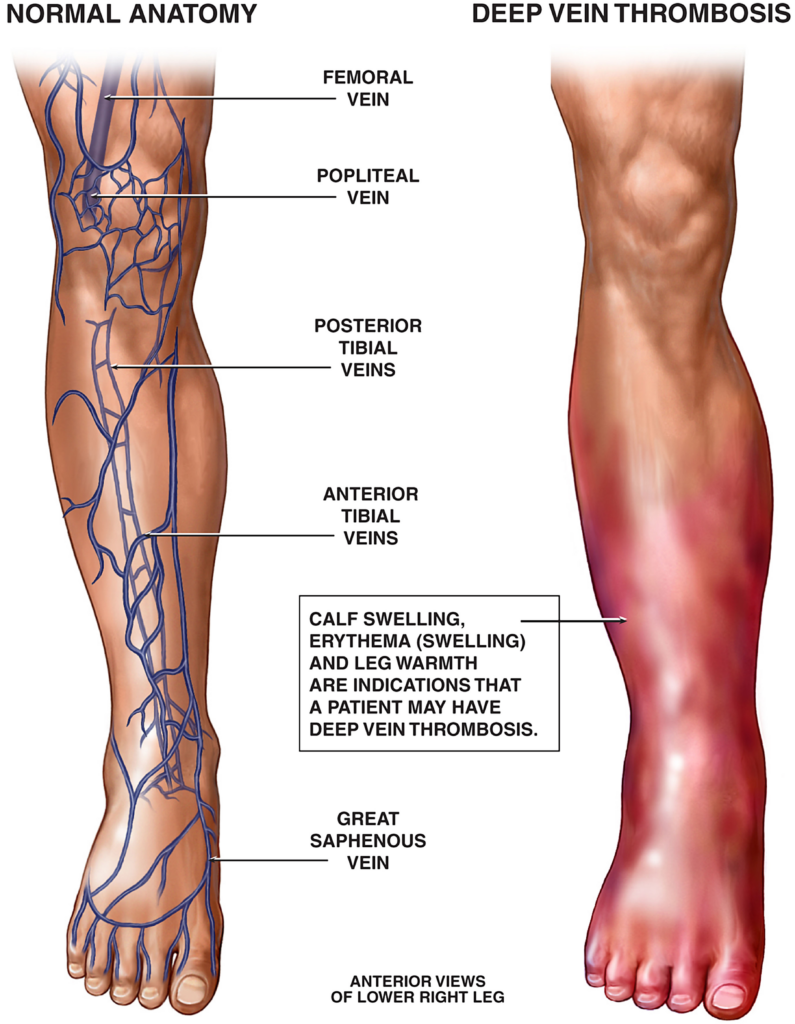
Symptoms and Signs
Recognizing the symptoms and signs of DVT is crucial for early detection and proper treatment. Common symptoms include pain, swelling, warmth, and redness in the affected leg. Some individuals may also experience a heavy ache or cramping sensation in the leg. It is important to seek medical attention if you notice these symptoms, as prompt diagnosis and treatment can prevent complications.
Causes and Pathophysiology of Deep Vein Thrombosis
Virchow’s Triad
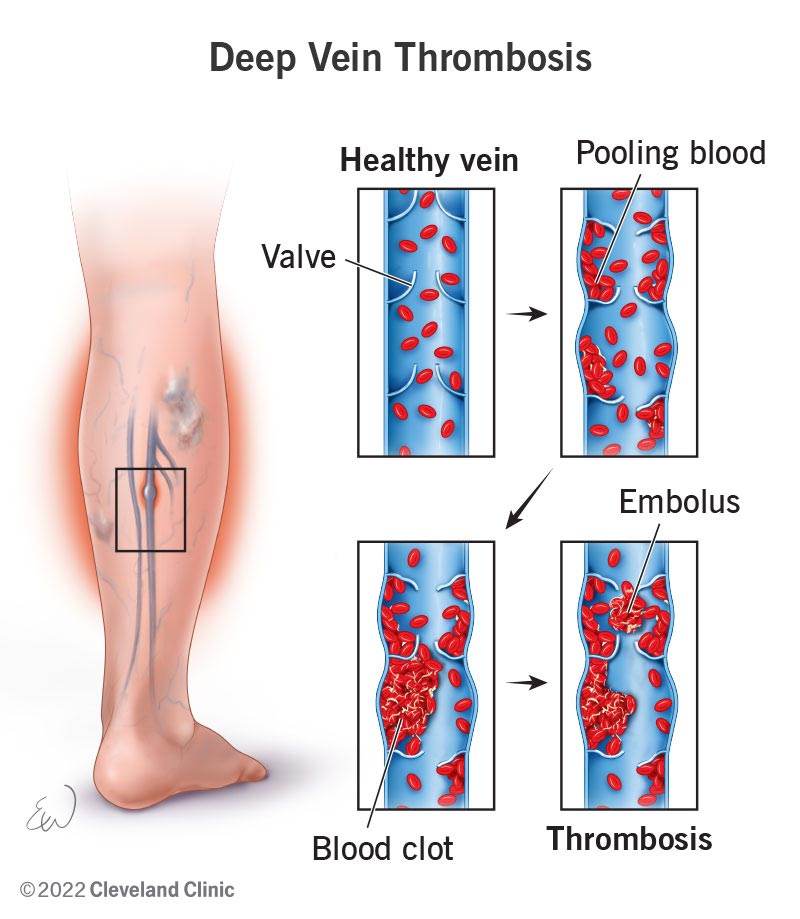
Virchow’s Triad is a concept that explains the main factors contributing to the development of DVT. It consists of three components: stasis of blood flow, endothelial injury, and hypercoagulability. Stasis occurs when blood circulation slows down, allowing blood to pool and potentially form clots. Endothelial injury refers to damage to the inner lining of blood vessels, which can trigger the formation of blood clots. Hypercoagulability refers to an increased tendency of the blood to clot. Understanding this triad can help in identifying and managing the risk factors associated with DVT.
Blood Clot Formation
The formation of a blood clot starts with the activation of platelets and the coagulation cascade. Platelets adhere to the site of injury, forming a plug, while the coagulation cascade leads to the production of fibrin, a protein that forms a mesh-like structure, strengthening the clot. In DVT, this process occurs within deep veins, leading to the formation of a thrombus or blood clot. The understanding of this process is essential for healthcare professionals to develop appropriate treatment strategies.
Contributing Factors
Several factors contribute to the development of DVT. Prolonged immobility, such as during long-haul flights or bed rest after surgery, can slow down blood flow, increasing the risk of clot formation. Certain medical conditions, such as cancer, heart disease, and inflammatory disorders, can also increase the likelihood of developing DVT. Additionally, hormonal changes during pregnancy or the use of estrogen-containing medications can contribute to blood clot formation. Being aware of these contributing factors is crucial in the prevention and management of DVT.
Diagnosis of Deep Vein Thrombosis
Medical History and Physical Examination
Diagnosing DVT often begins with a medical history assessment to identify potential risk factors and symptoms. A physical examination is then performed, focusing on the affected leg, looking for signs of swelling, pain, redness, and warmth. These initial steps help healthcare professionals determine the likelihood of DVT and guide further diagnostic testing.
Diagnostic Tests
Various diagnostic tests can be utilized to confirm the presence of DVT. The D-dimer blood test measures a substance produced when blood clots break down. An elevated level of D-dimer suggests the presence of a clot, although further testing is required to confirm the diagnosis. Ultrasound is commonly used to visualize the affected vein and to assess blood flow. Occasionally, venography or blood tests for genetic factors can be employed to assist with diagnosis.
Imaging Techniques
Imaging techniques such as ultrasound, venography, and magnetic resonance imaging (MRI) can be used to visualize the deep veins and identify blood clots. Ultrasound is the most common and non-invasive imaging technique used for diagnosing DVT. It allows healthcare professionals to directly visualize the clot and assess the extent of venous blockage. Venography, although less commonly used, involves injecting a contrast dye into a vein to obtain a clear image of blood flow. MRI can provide detailed images of blood vessels without the need for contrast dye.
Complications and Consequences of Deep Vein Thrombosis
Pulmonary Embolism
One of the most severe complications of DVT is a pulmonary embolism (PE). A PE occurs when a blood clot dislodges from the deep veins and travels to the lungs, where it can block the blood flow. This can result in a life-threatening situation, compromising the oxygen supply to the organs. Symptoms of a PE include sudden shortness of breath, chest pain, coughing up blood, and rapid heart rate. Immediate medical attention is required if a PE is suspected.
Post-thrombotic Syndrome
Post-thrombotic Syndrome (PTS) refers to the long-term effects of DVT, which can result in chronic leg pain, swelling, and skin changes. The damaged veins and increased pressure caused by DVT can lead to inefficient blood flow and pooling of blood in the legs. This can cause discomfort and potentially lead to skin ulcerations. Proper management and treatment of DVT can help reduce the risk of developing PTS.

Treatment and Management of Deep Vein Thrombosis
Anticoagulant Therapy
Anticoagulant therapy, commonly referred to as blood thinners, is a standard treatment for DVT. These medications help prevent the formation of new blood clots and reduce the risk of existing clots growing in size. They do not dissolve the clot but allow the body’s natural processes to break it down over time. Anticoagulants can be administered orally or through injections, depending on the severity of the DVT and the individual’s overall health.
Thrombolytic Therapy
Thrombolytic therapy, also known as clot-busting medication, is utilized in severe cases of DVT where there is a high risk of complications. These medications help dissolve the blood clot quickly, restoring blood flow. However, thrombolytic therapy carries a higher risk of bleeding complications and is typically reserved for specific indications and closely monitored patients.
Compression Stockings
Compression stockings can be used as part of the treatment and management plan for individuals with DVT. These specialized stockings apply pressure to the legs, promoting blood flow and preventing blood from pooling in the veins. Compression stockings can reduce swelling and discomfort and help prevent post-thrombotic syndrome. They are available in different compression levels and should be properly fitted and worn consistently for optimal effectiveness.
Inferior Vena Cava Filters
Inferior Vena Cava (IVC) filters may be considered in cases where anticoagulant therapy is contraindicated or ineffective. These filters are placed in the large vein that carries blood from the lower body to the heart, known as the inferior vena cava. Their purpose is to catch blood clots before they reach the lungs, reducing the risk of a pulmonary embolism. IVC filters are often used as a temporary measure and can be removed once the risk has subsided.
Prevention of Deep Vein Thrombosis
Prophylactic Measures
Preventing DVT involves adopting certain preventive measures, particularly in high-risk situations. During long periods of immobility, such as during air travel or recovery after surgery, individuals should try to move and stretch their legs regularly. Avoiding long periods of sitting or standing without movement is also important. Additionally, individuals should wear loose-fitting clothing and avoid constrictive garments that can impede blood flow.
Early Ambulation and Leg Exercises
One of the most effective ways to prevent DVT is early ambulation, especially after surgery or extended immobility. Encouraging movement and walking as soon as possible helps maintain proper blood circulation in the lower extremities. In situations where movement is limited, healthcare professionals may recommend specific leg exercises that promote blood flow and reduce the risk of clot formation.
Drug Prophylaxis
In certain high-risk situations, such as major orthopedic surgery or hospitalization for medical conditions, healthcare professionals may prescribe drug prophylaxis to prevent DVT. This can involve the administration of anticoagulant medications or the use of intermittent pneumatic compression devices. These interventions aim to reduce the risk of blood clot formation during periods of immobilization or surgery.
Lifestyle Modifications for Deep Vein Thrombosis
Dietary Recommendations
Maintaining a healthy diet is important for managing the risk factors associated with DVT. Eating a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats can promote overall cardiovascular health. Limited intake of sodium and processed foods can help manage blood pressure levels, reducing the risk of DVT.
Physical Activity and Exercise
Regular physical activity and exercise play a significant role in preventing DVT. Engaging in activities that promote cardiovascular health, such as walking, swimming, or cycling, can improve circulation, strengthen the muscles, and reduce the risk of blood clot formation. It is important to discuss exercise plans with a healthcare professional, especially if there are specific considerations or restrictions.
Smoking and Alcohol Cessation
Smoking and excessive alcohol consumption can significantly increase the risk of DVT. Smoking damages blood vessels and promotes blood clot formation, while excessive alcohol can impair liver function, affecting the body’s natural ability to prevent clot formation. Quitting smoking and moderating alcohol intake can greatly reduce the risk of developing DVT.
Long-Term Management of Deep Vein Thrombosis
Follow-up Care
After a DVT diagnosis, regular follow-up care is essential. Healthcare professionals will monitor your progress, adjust treatment as needed, and provide recommendations to prevent future blood clots. Regular check-ups allow healthcare professionals to assess risk factors, manage medications, and provide ongoing support.
Duration of Anticoagulation
The duration of anticoagulation therapy may vary depending on the individual and the specific circumstances. For a first-time unprovoked DVT, a treatment period of three to six months is typically recommended. However, for individuals with certain risk factors, such as recurrent DVT or an underlying clotting disorder, extended or lifelong anticoagulation therapy may be necessary. The duration of therapy should be discussed with a healthcare professional.
Patient Education and Support
Education and support are crucial components of long-term management for individuals with DVT. Healthcare professionals should provide comprehensive information about the condition, treatment options, and lifestyle modifications. This empowers individuals to better understand and manage their condition, reducing the risk of future blood clots and improving overall quality of life.
Research and Advances in Deep Vein Thrombosis
Genetic Studies
Research into genetic factors associated with DVT has provided valuable insights into the pathophysiology of the condition. Genetic studies have identified specific gene mutations that predispose individuals to blood clot formation. Understanding these genetic factors can help identify high-risk individuals and develop targeted preventive strategies.
New Drug Development
Ongoing research and development efforts are focused on identifying new and more effective medications for the prevention and treatment of DVT. Novel anticoagulants with improved safety profiles and options for oral administration are being investigated. These advancements have the potential to simplify treatment regimens and improve patient outcomes.
Surgical Interventions
Surgical interventions may be considered in certain cases of DVT. Thrombectomy, a procedure to remove the blood clot, can be used in severe cases where medication alone is insufficient. Surgical interventions are typically reserved for specific indications, and the decision to pursue surgery is made on an individual basis, taking into consideration factors such as clot location and the patient’s overall health.
Impact of Deep Vein Thrombosis on Quality of Life
Psychological Effects
The diagnosis and treatment of DVT can have psychological effects on individuals. The realization that they have a potentially life-threatening condition can cause anxiety, stress, and emotional distress. It is important for healthcare professionals to provide emotional support and resources to help individuals cope with these psychological impacts.
Functional Impairment
DVT, particularly when followed by post-thrombotic syndrome, can lead to functional impairment. Chronic pain, swelling, and mobility limitations can impact an individual’s ability to perform daily activities and maintain an active lifestyle. Physical therapy and rehabilitation programs can play a crucial role in optimizing functional outcomes and improving quality of life for individuals with DVT.
In conclusion, Deep Vein Thrombosis is a serious medical condition that can have significant consequences if not properly diagnosed and treated. Recognizing the risk factors, symptoms, and available diagnostic and treatment options are essential for managing and preventing DVT. By understanding the impact of DVT and implementing lifestyle modifications, individuals can take proactive steps towards reducing their risk and improving their overall quality of life. Ongoing research and advancements in the field continue to enhance our understanding and management of this condition, providing hope for improved outcomes in the future.