Hey there! If you’ve ever wondered about liver failure and what it entails, this article has got you covered. We’ll give you a digestible overview of the causes, symptoms, and treatment options for liver failure. So, get ready to learn more about this important topic and gain a better understanding of what happens when the liver stops functioning properly.
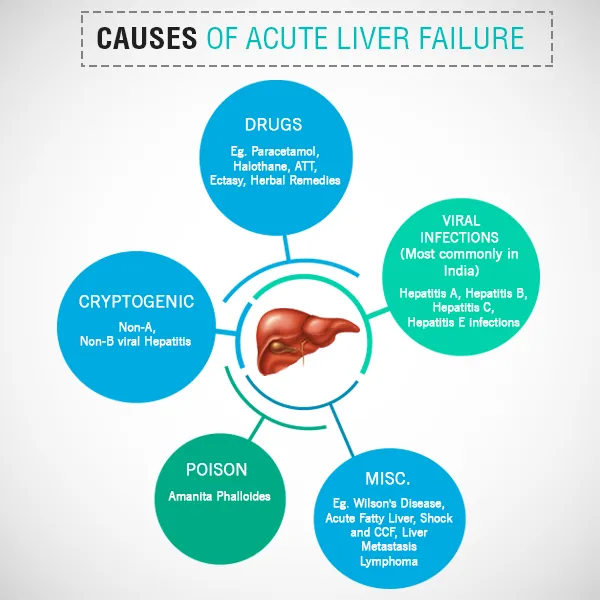
Causes of Liver Failure
Liver failure occurs when the liver is unable to perform its vital functions, leading to severe health complications. There are various causes of liver failure, including:
Alcohol-related liver disease
Excessive alcohol consumption over an extended period is a leading cause of liver failure. When alcohol is regularly consumed in large quantities, it can lead to the development of alcoholic hepatitis and cirrhosis. These conditions cause inflammation and scarring of the liver, impairing its ability to function properly.
Hepatitis
Hepatitis is inflammation of the liver, often caused by viral infections. There are several types of viral hepatitis, including hepatitis A, B, C, D, and E. Hepatitis B and C are particularly concerning as they can lead to chronic liver disease, cirrhosis, and ultimately liver failure if left untreated.
Cirrhosis
Cirrhosis is a chronic condition characterized by the irreversible scarring of the liver. It can be caused by factors such as excessive alcohol consumption, chronic hepatitis, fatty liver disease, or certain genetic disorders. Over time, the scarring replaces healthy liver tissue and impairs liver function, eventually leading to liver failure.
Nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) is a condition characterized by the accumulation of fat in the liver. It is closely associated with obesity, type 2 diabetes, and high cholesterol levels. In some cases, NAFLD can progress to a more severe condition known as nonalcoholic steatohepatitis (NASH), which can lead to cirrhosis and liver failure.
Autoimmune hepatitis
Autoimmune hepatitis is a chronic disease in which the immune system mistakenly attacks the liver, causing inflammation and damage. If left untreated, autoimmune hepatitis can progress to cirrhosis and liver failure. It is more common in women and may have a genetic component.
Genetic disorders
Certain genetic disorders can increase the risk of liver failure. Examples include hemochromatosis, Wilson disease, alpha-1 antitrypsin deficiency, and glycogen storage diseases. These genetic conditions affect the liver’s ability to function properly and can lead to severe liver damage if left untreated.
Medication-induced liver injury
Some medications can cause liver damage in susceptible individuals. Over-the-counter medications, prescription drugs, and herbal supplements have all been known to cause medication-induced liver injury. It is crucial to follow proper dosage guidelines and consult a healthcare professional if any liver-related symptoms occur during medication use.
Viral infections
Aside from hepatitis viruses, other viral infections can cause liver failure. For example, the Epstein-Barr virus (EBV) and cytomegalovirus (CMV) can both cause hepatitis and potentially lead to liver failure. Prompt diagnosis and early treatment are crucial in managing these viral infections to prevent further liver damage.
Toxins and chemicals
Exposure to certain toxins and chemicals can damage the liver and contribute to liver failure. These toxins can be found in household products, industrial chemicals, pesticides, and environmental pollutants. Avoidance of these toxins and practicing proper safety measures can help reduce the risk of liver damage.
Metabolic disorders
Metabolic disorders like Wilson disease and alpha-1 antitrypsin deficiency can interfere with the liver’s ability to process and metabolize fats, proteins, and other substances. Over time, this can lead to severe liver damage and liver failure.
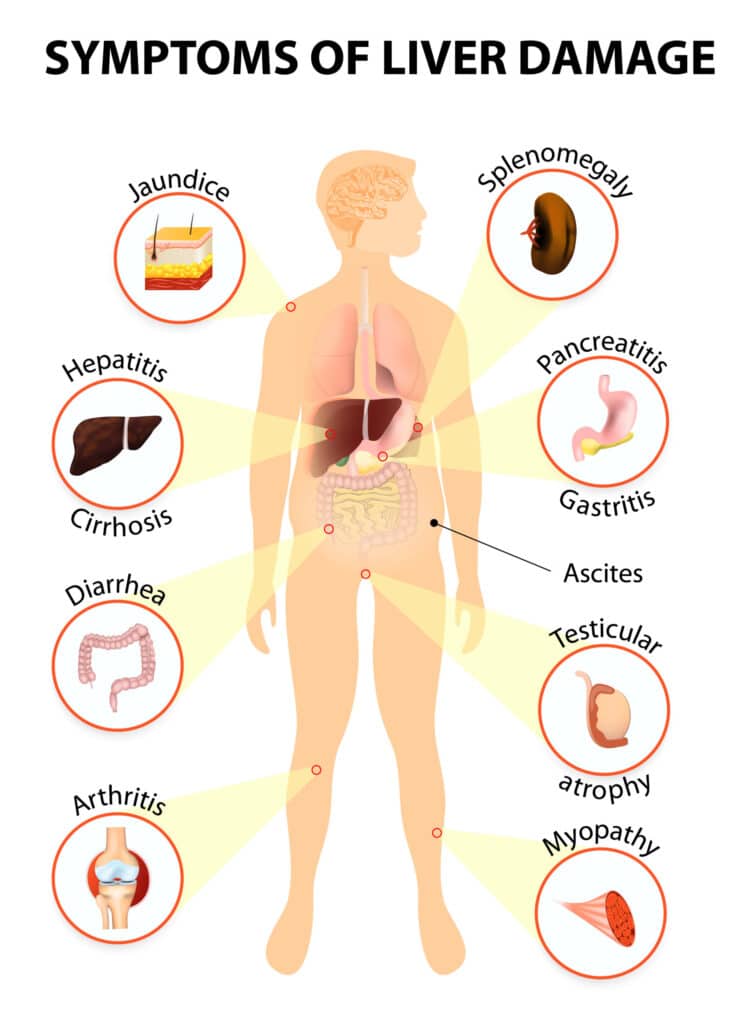
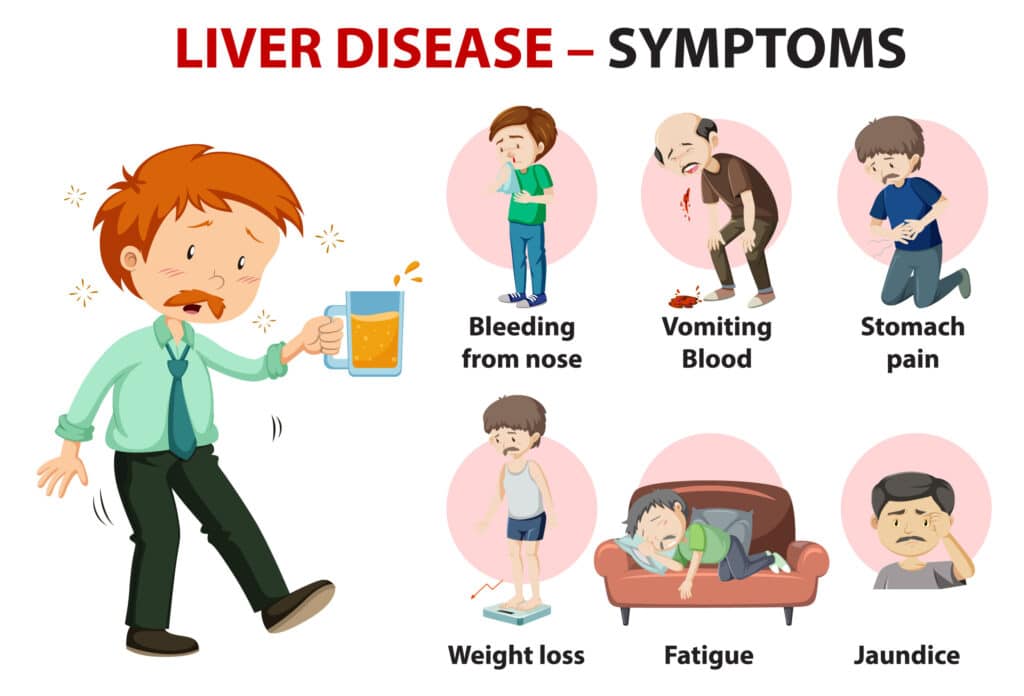
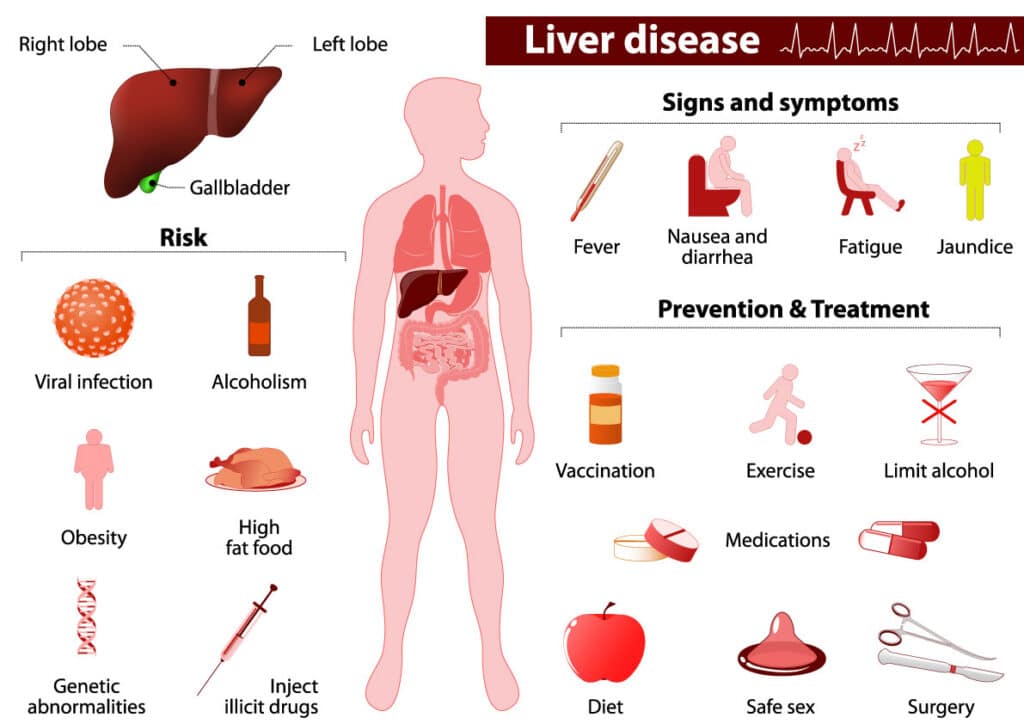
Symptoms of Liver Failure
Liver failure often presents with various symptoms, indicating the need for immediate medical attention. These symptoms may include:
Jaundice
Jaundice is characterized by yellowing of the skin and eyes due to the build-up of bilirubin, a substance produced during the breakdown of red blood cells. It is a common symptom of liver failure and indicates a dysfunction in the liver’s ability to filter and process bilirubin.
Abdominal pain and swelling
Liver failure can cause abdominal pain and swelling due to the accumulation of fluid in the abdomen. This condition, known as ascites, is a direct result of impaired liver function and can cause discomfort and a distended abdomen.
Easy bleeding and bruising
The liver produces proteins necessary for blood clotting. When liver function is compromised, the production of these clotting factors is disrupted, leading to easy bleeding and bruising. Small injuries may result in prolonged bleeding, and frequent bruising may occur even with minimal impact.
Fatigue and weakness
Liver failure can cause extreme fatigue and weakness, making it challenging for individuals to perform daily activities. This fatigue is a result of the liver’s inability to store and release glucose, which is essential for providing energy to the body.
Nausea and vomiting
Liver failure can lead to nausea and vomiting due to the liver’s impaired ability to process toxins and remove them from the body. This build-up of toxins can cause gastrointestinal disturbances and contribute to feelings of nausea and bouts of vomiting.
Loss of appetite and weight loss
A decreased appetite and unintentional weight loss are common symptoms of liver failure. The liver plays a crucial role in the digestion and metabolism of nutrients. When liver function is compromised, individuals may experience a loss of appetite and difficulty maintaining a healthy weight.
Mental confusion or disorientation
When the liver fails to eliminate toxins from the body, these substances can build up in the blood and affect brain function. This can result in mental confusion, disorientation, and difficulty concentrating. In severe cases, liver failure may lead to hepatic encephalopathy, a condition characterized by cognitive impairment and altered consciousness.
Personality or mood changes
Liver failure can also cause changes in personality and mood. These changes may manifest as irritability, mood swings, depression, or anxiety, and can significantly impact an individual’s overall well-being and quality of life.
Swelling in the legs and ankles
Impaired liver function can lead to fluid retention in the body, causing swelling in the legs and ankles. This swelling, known as edema, occurs due to a decrease in the production of albumin, a protein responsible for maintaining fluid balance in the body.
Frequent infections
The liver plays a vital role in the immune system, helping to fight off infections. When liver function is compromised, individuals have a higher risk of developing frequent infections. This is because the liver’s ability to produce proteins and filter bacteria and toxins from the blood is impaired.
Diagnosis of Liver Failure
To diagnose liver failure, healthcare professionals utilize various diagnostic methods to assess liver function and identify underlying causes. These diagnostic procedures may include:
Physical examination
During a physical examination, a healthcare provider may assess the signs and symptoms commonly associated with liver failure. This may include evaluating the patient’s skin color, looking for jaundice, palpating the abdomen for tenderness or enlargement, and checking for signs of fluid retention.
Blood tests
Blood tests are essential in evaluating liver function and identifying any abnormalities or signs of liver damage. Liver function tests can measure levels of liver enzymes, bilirubin, albumin, and other substances to assess liver function and detect any potential liver-related issues.
Imaging tests
Imaging tests such as ultrasound, computed tomography (CT) scan, or magnetic resonance imaging (MRI) may be used to visualize the liver and surrounding structures. These tests can help identify any abnormalities, such as tumors, cysts, or signs of cirrhosis.
Liver biopsy
In some cases, a liver biopsy may be performed to obtain a sample of liver tissue for further examination. This procedure involves taking a small piece of liver tissue using a needle, which is then analyzed under a microscope to check for signs of inflammation, scarring, or liver diseases.
Medical history and symptoms evaluation
A thorough evaluation of the patient’s medical history and a detailed understanding of the symptoms experienced are crucial in diagnosing liver failure. This information helps healthcare providers identify potential risk factors, underlying causes, and any previous liver-related conditions.
Electroencephalogram (EEG)
In cases where hepatic encephalopathy is suspected, an electroencephalogram (EEG) may be performed to measure brain activity. This test can help assess the extent of cognitive impairment and monitor changes in brain function over time.
Complications of Liver Failure
Liver failure can lead to several complications that warrant prompt medical attention. These complications may include:
Portal hypertension
When liver failure occurs, blood flow through the liver becomes obstructed, leading to increased pressure in the portal vein, a major blood vessel supplying the liver. This condition, known as portal hypertension, can result in the development of varices (enlarged veins) in the esophagus and stomach, which are at risk of bleeding.
Hepatic encephalopathy
Hepatic encephalopathy is a severe complication of liver failure characterized by impaired brain function. It occurs as a result of the liver’s inability to process toxins, leading to an accumulation of substances in the blood that can affect brain activity and cognition.
Ascites
Ascites refers to the build-up of fluid in the abdomen caused by portal hypertension and a decrease in the production of albumin in the liver. Ascites can cause abdominal discomfort, difficulty breathing, and further complications if left untreated.
Hepatorenal syndrome
Hepatorenal syndrome is a potentially life-threatening condition that can occur in advanced stages of liver failure. It is characterized by kidney dysfunction and a decrease in renal blood flow. Prompt medical intervention is crucial to manage hepatorenal syndrome and prevent irreversible kidney damage.
Liver cancer
Liver failure increases the risk of developing liver cancer, also known as hepatocellular carcinoma (HCC). Chronic liver diseases, such as cirrhosis, significantly contribute to the development of liver cancer. Regular monitoring and appropriate treatment are essential to detect and manage liver cancer in individuals with liver failure.
Bacterial infections
Individuals with liver failure are more susceptible to bacterial infections due to the impaired immune function associated with compromised liver function. These infections can lead to sepsis and pose significant risks to overall health. Prompt treatment with antibiotics and close monitoring are necessary to prevent complications.
Treatment Options for Liver Failure
When diagnosed with liver failure, several treatment options are available to manage the condition and improve the patient’s quality of life. These treatment options may include:
Liver transplantation
Liver transplantation is considered the most effective treatment for severe cases of liver failure. This procedure involves replacing the damaged liver with a healthy liver from a deceased or living donor. A liver transplant can significantly extend a patient’s life and restore normal liver function.
Medications
Medications may be prescribed to manage the underlying causes of liver failure, such as antiviral drugs for viral hepatitis or immunosuppressive drugs for autoimmune hepatitis. Medications can also help alleviate symptoms, control complications, and slow down the progression of liver disease.
Lifestyle changes
Adopting a healthy lifestyle is crucial in managing liver failure. This includes avoiding alcohol consumption, maintaining a healthy weight, and exercising regularly. Lifestyle changes can help reduce the strain on the liver and improve overall health.
Dietary modifications
A well-balanced diet is essential for individuals with liver failure. It is crucial to limit the intake of substances that may further damage the liver, such as alcohol and certain medications. Additionally, a diet low in sodium can help manage fluid retention and minimize swelling.
Antibiotics for infections
Bacterial infections are common in individuals with liver failure. Antibiotics may be prescribed to treat these infections and prevent further complications. It is essential to promptly seek medical attention if any signs of infection, such as fever or increased pain, occur.
Monitoring and management of complications
Close monitoring and management of complications, such as ascites and hepatic encephalopathy, are necessary in individuals with liver failure. Regular follow-ups with healthcare providers are vital to assess and address any emerging issues promptly.
Supportive care
Supportive care, including symptom management and pain relief, plays a crucial role in improving the quality of life for individuals with liver failure. Palliative care can also be integrated to ensure the patient’s comfort and emotional support for both the patient and their loved ones.
Prevention and Risk Factors of Liver Failure
Liver failure can often be prevented by taking proactive measures and addressing the risk factors associated with the condition. Some prevention strategies and risk factors include:
Alcohol moderation or abstinence
Excessive alcohol consumption is a major risk factor for liver failure. Limiting alcohol intake or completely abstaining from alcohol can help reduce the risk of developing alcohol-related liver disease and other liver-related conditions.
Vaccination against viral hepatitis
Vaccination is available for hepatitis A and B, providing protection against these viral infections. Vaccinating against viral hepatitis reduces the risk of chronic liver disease, cirrhosis, and liver failure.
Safe needle practices and blood transfusion screening
Practicing safe needle practices, such as avoiding sharing needles, and ensuring the screening of blood transfusions for infectious diseases can prevent the transmission of viral hepatitis and reduce the risk of liver failure.
Avoidance of illicit drug use
Illicit drug use, particularly intravenous drug use, significantly increases the risk of viral hepatitis and liver damage. Avoiding illicit drug use and seeking treatment and support for addiction can help prevent liver failure.
Maintaining a healthy weight
Obesity and excessive weight gain are associated with nonalcoholic fatty liver disease (NAFLD). Maintaining a healthy weight through regular exercise and a balanced diet reduces the risk of developing liver-related conditions.
Maintaining a well-balanced diet
A well-balanced diet, low in processed foods and high in fruits, vegetables, and whole grains, can support liver health. Eating foods rich in antioxidants and limiting saturated fats can help prevent liver damage.
Regular exercise
Regular exercise benefits overall health, including liver health. Engaging in physical activity helps maintain a healthy weight, improve circulation, and enhance overall liver function.
Monitoring and managing chronic liver conditions
Individuals with chronic liver conditions should regularly consult with their healthcare providers to monitor their liver health and manage any potential complications. Regular check-ups and appropriate treatment can help prevent further liver damage and progression to liver failure.
Avoiding exposure to toxins and chemicals
Limiting exposure to toxins and chemicals, such as industrial chemicals and environmental pollutants, reduces the risk of liver damage. This includes utilizing protective measures in occupations involving potential exposure to hazardous substances.
Proper medication use
Follow proper dosage instructions and precautions when taking medications. Some medications can have adverse effects on the liver, especially if taken in excessive doses or over a prolonged period. Always consult a healthcare professional if there are concerns about liver-related side effects of medications.
Prognosis and Outlook for Liver Failure
The prognosis for liver failure varies depending on several factors, including the underlying cause, severity of liver damage, timeliness of diagnosis and intervention, the patient’s overall health, and the availability of treatment options like liver transplantation. The prognosis also heavily relies on the management of complications, adherence to prescribed treatments, and lifestyle changes.
For individuals with early-stage liver failure and favorable conditions, timely intervention and adherence to treatment plans can help improve liver function and quality of life. However, in advanced cases with severe liver damage, the prognosis may be more challenging, and liver transplantation may be the most viable option.
Regular monitoring, managing complications, and appropriate lifestyle modifications are essential for maintaining stable liver function and ensuring a better prognosis for individuals with liver failure.
Support and Resources for Liver Failure Patients
Living with liver failure can be physically and emotionally challenging. Fortunately, there are numerous support and resources available to help individuals and their loved ones navigate this difficult journey. Some of these include:
Liver failure support groups
Joining liver failure support groups provides an invaluable opportunity to connect with others facing similar challenges. These groups offer a safe space for sharing experiences, receiving advice, and finding emotional support from individuals who understand the unique struggles of living with liver failure.
Online forums and communities
Virtual platforms and online forums dedicated to liver failure allow individuals to connect with a wider community of patients, caregivers, and medical professionals. These platforms provide a platform for information exchange, crowd-sourced advice, and mutual support.
Liver disease awareness organizations
Liver disease awareness organizations play a vital role in advocating for liver health and offering educational resources. These organizations often provide information about liver diseases, treatment options, and available support services.
Educational materials and information
Educational materials, websites, and pamphlets specific to liver failure can help individuals understand the condition better, its causes, treatment options, and lifestyle modifications. Accessible information empowers individuals to take an active role in managing their health and making informed decisions.
Financial assistance programs
The cost of treating liver failure can be significant. Financial assistance programs and resources exist to provide support to individuals who may struggle with medical expenses. These programs can help alleviate financial burdens associated with liver failure treatment.
Peer support networks
Peer support networks connect individuals with experienced mentors or volunteers who have firsthand knowledge of liver failure. These networks offer guidance, answer questions, and provide encouragement to individuals and their families as they navigate the challenges of liver failure.
Healthcare providers and specialists
Healthcare providers and liver specialists offer medical expertise and guidance throughout the liver failure journey. Establishing a strong relationship with a knowledgeable and compassionate healthcare team is essential for receiving the best possible care and support.
Mental health support services
Living with liver failure can take a toll on mental well-being. Mental health support services, such as therapists and counselors, can provide emotional support, coping strategies, and help individuals navigate the emotional challenges that often accompany a serious medical condition.
Counseling and therapy
Counseling and therapy services can provide individuals and their families with a safe space to discuss their fears, concerns, and emotions related to liver failure. These sessions can help individuals develop healthy coping mechanisms and improve overall well-being.

Research and Advancements in Liver Failure
Continuous advancements in medical research provide hope for individuals living with liver failure. Ongoing studies and developments aim to improve diagnostic methods, treatment options, and overall outcomes for patients. Some areas of research and advancements in liver failure include:
Medical research studies
Medical research studies focus on understanding the causes, progression, and treatment of liver failure. These studies help uncover new insights into liver diseases and facilitate the development of innovative treatment approaches.
Advances in liver transplantation techniques
Advances in liver transplantation techniques have led to improved outcomes for patients with liver failure. Innovations in surgical procedures, organ preservation, and immunosuppressive therapies have increased the success rates of liver transplantation and extended the survival of transplant recipients.
Regenerative medicine and stem cell therapies
Regenerative medicine and stem cell therapies hold promise for individuals with liver failure. Researchers are investigating the potential of using stem cells to repair damaged liver tissue and promote liver regeneration.
Pharmacological developments in treatment
Researchers are constantly exploring new pharmacological options for treating liver failure. The development of targeted therapies, new antiviral medications, and novel drugs that inhibit liver fibrosis are among the areas of pharmacological advancement in liver failure treatment.
Genetic studies and personalized medicine
Advancements in genetic studies and personalized medicine offer the potential for tailored treatments based on a patient’s unique genetic makeup. Understanding the genetic factors contributing to liver failure can help identify individuals at risk and develop personalized interventions and treatments.
Liver biome research
Research focused on the liver biome, the collection of microorganisms within the liver, aims to understand the interaction between the microbiome and liver health. This emerging field of study has the potential to uncover new therapeutic approaches and preventive strategies for liver failure.
Improved diagnostic methods
Improved diagnostic methods, including non-invasive techniques and biomarker identification, are being developed to aid in the early detection and accurate diagnosis of liver failure. These advancements can lead to earlier intervention and better outcomes for individuals with liver failure.
Public health initiatives
Public health initiatives play a crucial role in the prevention and management of liver failure. Awareness campaigns, vaccination programs, and initiatives aimed at promoting healthy lifestyles can help reduce the incidence of liver failure and improve overall liver health within communities.
Conclusion
Liver failure is a serious condition that can significantly impact an individual’s health and quality of life. Understanding the causes, symptoms, and available treatment options for liver failure is essential for early detection, timely intervention, and effective management of the condition.
By addressing underlying causes, managing symptoms, and adopting healthy lifestyle practices, individuals can take proactive steps towards preventing liver failure. Proper diagnosis, treatment, and supportive care can help improve outcomes and ensure better quality of life for those living with liver failure.
Through ongoing research and advancements in medical knowledge, the future holds the promise of more targeted treatments and improved outcomes for individuals with liver failure. Support networks, resources, and organizations dedicated to liver health provide valuable assistance and guidance to individuals and their loved ones as they navigate the challenges of living with liver failure.