If you or someone you know has ever experienced the discomfort of bronchitis or asthma, you may have wondered about the potential link between the two conditions. In this article, we will explore the fascinating connection between bronchitis and asthma and shed light on how understanding this relationship can help manage and alleviate the symptoms associated with both. By gaining insight into the shared characteristics and triggers of these respiratory conditions, you will be better equipped to take control of your health and breathe easier.
Overview of Bronchitis and Asthma
Bronchitis and asthma are two respiratory conditions that can affect your breathing and overall lung health. While they are distinct conditions, there is some overlap in terms of symptoms and treatment options. In this comprehensive article, we will explore the definitions, symptoms, causes, diagnosis, treatment options, prevention, and management strategies for both bronchitis and asthma.
Definition of Bronchitis
Bronchitis is an inflammation of the bronchial tubes in the lungs. The bronchial tubes are responsible for carrying air to and from the lungs. When these tubes become inflamed, they produce excess mucus, leading to a persistent cough. Bronchitis can either be acute or chronic.
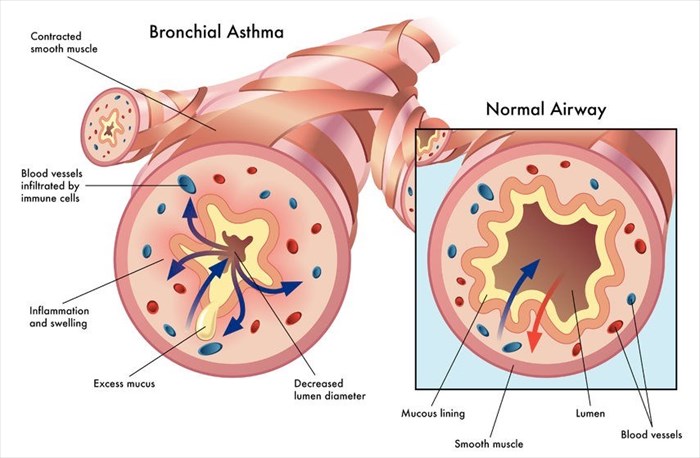
Definition of Asthma
Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways. This inflammation makes the airways hypersensitive, causing them to constrict when exposed to certain triggers. This can result in difficulty breathing, wheezing, and a feeling of tightness in the chest.
Common Symptoms of Bronchitis
The symptoms of bronchitis can vary depending on whether it is acute or chronic. Acute bronchitis often develops following a respiratory infection such as a cold or the flu. Common symptoms include coughing (with or without mucus), chest discomfort or tightness, fatigue, and low-grade fever. Chronic bronchitis, on the other hand, is a long-term condition and is generally characterized by a productive cough that lasts for at least three months a year for two consecutive years.
Common Symptoms of Asthma
Asthma symptoms can range from mild to severe and can vary from person to person. Common symptoms include wheezing (a high-pitched whistling sound during breathing), shortness of breath, chest tightness, and coughing, especially at night or in the early morning.
Types of Bronchitis
Acute Bronchitis
Acute bronchitis is usually caused by a viral infection and is characterized by a sudden onset of symptoms that last for a short period of time. The most common cause is the same viruses that cause the common cold or flu. Acute bronchitis typically resolves on its own within a few weeks with rest and supportive care.
Chronic Bronchitis
Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD) and is typically caused by long-term exposure to irritants such as cigarette smoke or air pollution. It is characterized by a persistent cough that lasts for at least three months a year for two consecutive years. Chronic bronchitis may require ongoing medical management to control symptoms and prevent complications.
Types of Asthma
Allergic Asthma
Allergic asthma is the most common type of asthma and is triggered by exposure to allergens such as pollen, dust mites, pet dander, or mold. When a person with allergic asthma comes into contact with an allergen, their immune system overreacts, leading to the inflammation and constriction of the airways.
Non-allergic Asthma
Non-allergic asthma is not triggered by allergens but is instead caused by factors such as exercise, cold air, respiratory infections, or irritants like smoke or strong odors. Non-allergic asthma can occur in people with no other known allergies.
Exercise-induced Asthma
Exercise-induced asthma, also known as exercise-induced bronchoconstriction, occurs when physical exertion triggers the narrowing of the airways. Symptoms usually occur during or after exercise and may include coughing, wheezing, shortness of breath, and chest tightness.
Occupational Asthma
Occupational asthma is caused by exposure to certain substances in the workplace. These substances can include chemicals, dust, gases, or fumes. Symptoms may arise shortly after exposure or may take months or even years to develop.
Causes and Risk Factors
Viral and Bacterial Infections
Both bronchitis and asthma can be triggered by viral and bacterial infections. In the case of bronchitis, acute bronchitis is often caused by viral infections, while chronic bronchitis can be exacerbated by bacterial infections. Similarly, respiratory infections can trigger asthma attacks in individuals with asthma.
Environmental Irritants
Exposure to environmental irritants such as cigarette smoke, air pollution, strong odors, and chemical fumes can worsen symptoms of both bronchitis and asthma. These irritants can inflame the airways and make breathing more difficult.
Smoking
Smoking is a significant risk factor for both bronchitis and asthma. The chemicals in cigarette smoke irritate the airways and can lead to chronic inflammation, making it more difficult to breathe for individuals with these conditions.
Family History
A family history of bronchitis or asthma can increase your risk of developing these conditions. There may be a genetic predisposition that makes some individuals more susceptible to respiratory problems.
Allergens
Exposure to allergens such as pollen, dust mites, pet dander, or mold can trigger symptoms in individuals with bronchitis or asthma, especially those with allergic asthma. Allergens can cause an allergic reaction in the airways, leading to inflammation and breathing difficulties.

Similarities and Differences
Airway Inflammation
Both bronchitis and asthma involve inflammation of the airways. In bronchitis, the inflammation is typically caused by a viral or bacterial infection, while in asthma, it is a chronic condition characterized by ongoing airway inflammation.
Causes of Inflammation
The causes of inflammation in bronchitis and asthma differ. Bronchitis is often caused by respiratory infections, while asthma is typically triggered by allergens, irritants, exercise, or respiratory infections.
Triggers
The triggers for bronchitis and asthma can overlap but also differ. Both conditions can be triggered by respiratory infections and environmental irritants. However, asthma is more commonly triggered by allergens or exercise, while specific triggers for bronchitis may include exposure to irritants such as cigarette smoke or air pollution.
Reversible vs. Irreversible
Bronchitis and asthma differ in terms of reversibility. Acute bronchitis is usually reversible and resolves within a few weeks, while chronic bronchitis is often irreversible and requires ongoing management. Asthma symptoms can be reversible with appropriate treatment and management.
Diagnosis
To diagnose both bronchitis and asthma, healthcare professionals will typically perform a thorough evaluation, including:
Medical History
Your healthcare provider will inquire about your symptoms, medical history, and family history of respiratory conditions. This information will help in determining the underlying cause and appropriate treatment options.
Physical Examination
A physical examination will be conducted, including listening to your lungs for abnormal sounds such as wheezing or crackling. Your healthcare provider will also check for signs of respiratory distress.
Spirometry
Spirometry is a common diagnostic test used to evaluate lung function. It measures the amount of air you can breathe in and out, as well as how quickly you can exhale. This test can help diagnose and monitor both bronchitis and asthma.
Peak Flow Measurements
Peak flow measurements are used primarily in the diagnosis and monitoring of asthma. This test measures how forcefully you can exhale and helps assess the severity of airflow obstruction.
Chest X-ray
A chest X-ray may be ordered to rule out other respiratory conditions and to check for any abnormalities in the lungs.
Allergy Testing
Allergy testing may be performed to identify specific allergens that may be triggering your asthma symptoms. This can help in developing an appropriate management plan.

Treatment Options
Treatment options for both bronchitis and asthma aim to alleviate symptoms, reduce inflammation, and improve overall lung function. The specific treatment plan will depend on the severity of your condition and individual needs.
Bronchodilators
Bronchodilators are medications that help relax the muscles in the airways, allowing for easier breathing. They can be in the form of inhalers, tablets, or syrups. Short-acting bronchodilators are used for quick relief of symptoms, while long-acting bronchodilators are used for long-term management.
Anti-inflammatory Medications
Anti-inflammatory medications, such as corticosteroids, are often prescribed to reduce airway inflammation in asthma. These medications help prevent asthma attacks and can be taken orally, inhaled, or through injection.
Corticosteroids
Corticosteroids are powerful anti-inflammatory medications that can help reduce inflammation in the airways in both bronchitis and asthma. They can be taken orally or inhaled, depending on the severity of symptoms and the individual’s response to treatment.
Antibiotics
If bronchitis is caused by a bacterial infection, antibiotics may be prescribed. However, antibiotics are not effective against viral infections, which are the most common cause of acute bronchitis.
Oxygen Therapy
In severe cases of bronchitis or asthma, where there is a significant decrease in blood oxygen levels, oxygen therapy may be administered. This involves the delivery of supplemental oxygen through a mask or nasal cannula to improve oxygenation.
Lifestyle Changes
Making certain lifestyle changes can help manage both bronchitis and asthma. This may include avoiding triggers, maintaining a healthy weight, exercising regularly, and practicing good respiratory hygiene.
Allergy Shots
Allergy shots, also known as immunotherapy, may be recommended for individuals with allergic asthma. These shots gradually expose the individual to increasing amounts of allergens to desensitize their immune system and reduce the severity of allergic reactions.
Prevention
Avoiding Triggers
One of the most effective ways to prevent bronchitis and asthma flare-ups is to avoid triggers. This may involve staying away from cigarette smoke, reducing exposure to allergens, and avoiding situations that may exacerbate symptoms, such as exercising in cold air.
Proper Hygiene
Practicing good respiratory hygiene, such as covering your mouth and nose when coughing or sneezing, can help prevent the spread of respiratory infections that can lead to bronchitis. Regular handwashing can also reduce the risk of infection.
Vaccinations
Ensuring that you are up to date with vaccinations, such as the flu vaccine and pneumonia vaccine, can help reduce the risk of respiratory infections and complications.
Maintaining a Healthy Lifestyle
Maintaining a healthy lifestyle, including eating a balanced diet, getting regular exercise, and managing stress, can help support your overall lung health and reduce the risk of respiratory conditions.
Quitting Smoking
If you are a smoker, quitting smoking is one of the best things you can do for your lung health. It can help reduce the risk of developing bronchitis and asthma, as well as improve the effectiveness of treatment for existing respiratory conditions.
Managing Bronchitis and Asthma
Developing an Asthma Action Plan
For individuals with asthma, developing an asthma action plan in consultation with your healthcare provider is crucial. This plan outlines specific steps to take when symptoms worsen, including adjusting medication dosages and seeking medical attention.
Monitoring Symptoms
Monitoring symptoms is important for both bronchitis and asthma. It can help identify triggers and assess the effectiveness of treatment. Regularly monitoring symptoms allows for early intervention and prevents complications.
Regular Follow-up Care
Regular follow-up care with your healthcare provider is essential for managing bronchitis and asthma. They can assess your lung function, adjust treatment plans if necessary, and provide ongoing support and education.
Supportive Self-care Measures
Engaging in supportive self-care measures can help manage both bronchitis and asthma. This includes getting plenty of rest, staying hydrated, using a humidifier to moisten the air, and avoiding exposure to smoke or other irritants.
Conclusion
Bronchitis and asthma are respiratory conditions that can significantly impact your breathing and overall quality of life. While they have distinct characteristics, understanding the connection between the two can help in better managing and preventing exacerbations. By recognizing the symptoms, triggers, and treatment options, individuals can take the necessary steps to lead a healthier and more comfortable life. It is essential to work closely with healthcare professionals to develop a personalized treatment plan and to consistently follow self-care measures to effectively manage bronchitis and asthma.